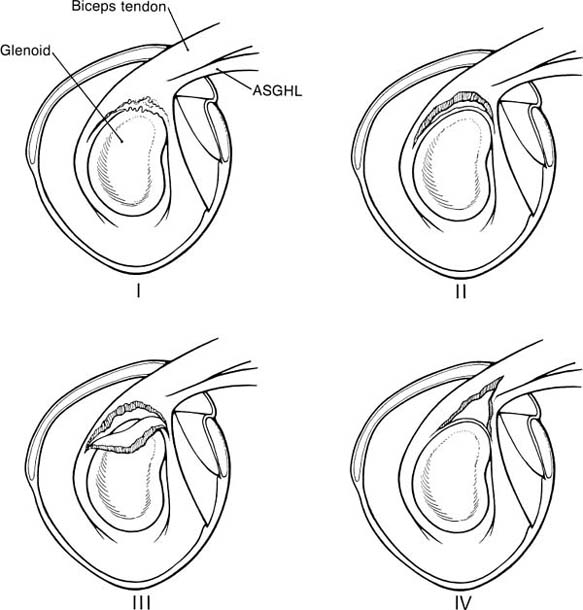
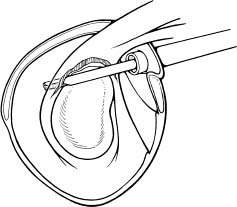
Case 15 A 27-year-old right-hand-dominant laborer presents to the office 3 months after an injury that he described as a downward jerk on the arm occurring when a heavy box of tools slipped off of its support while he was holding the tool box handle. He reported an acute onset of shoulder pain, but he denies a frank dislocation. Since that episode, he has been unable to do overhead work secondary to pain and popping in the shoulder. He also reports weakness and subtle “looseness” in the shoulder, but denies any numbness or other neurologic complaints. Range of motion of the shoulder is normal both actively and passively. He has normal strength, but has pain to resisted forward flexion. He has a positive Speed’s test and a positive compression-rotation test accomplished by applying a compressive load along the long axis of the humerus while rotating the shoulder. This compression-rotation test elicited pain and a palpable click in the shoulder. Translation testing failed to demonstrate any dramatic increase in anterior, posterior, or inferior translations. However, selective loading of the anterior-superior quadrant structures caused pain and a reproduction of the patient’s symptoms. No atrophy, asymmetry, or other irregularity was identified in the involved shoulder. 1. Anterior shoulder instability 2. Rotator cuff tear 3. Superior labrum anterior and posterior (SLAP) lesion 4. Impingement syndrome An anteroposterior (AP), axillary view, and scapular Y view failed to reveal any abnormalities. SLAP Lesion. There are no unique signs for lesions of the superior labrum. SLAP lesions present with a variable history of symptoms and a variety of mechanisms initiating those symptoms. Mechanisms and symptoms include falls directly on to the lateral aspect of the shoulder; a sudden, acute traction injury to the arm, and vague discomfort with overhead use without specific injury. Patients with SLAP lesions generally complain of pain, decreased endurance, popping, and sometimes subluxation. Physical examination can lead the physician to suspect a SLAP lesion, but no test is pathognomonic. Active and passive range of motion are usually normal, but impingement signs, including pain on frontal flexion (Neer sign) and rotation from external rotation to internal rotation in 90 degrees of abduction (Hawkins sign), are often positive due to secondary rotator cuff involvement. Although the standard apprehension position may be painful, Jobe’s augmentation and relocation test are usually negative. Snyder and colleagues (1990) coined the term “SLAP” in referring to these lesions. They classified the lesions into four categories based on physical characteristics identified at the time of shoulder arthroscopy (Fig. 15–1). Four specific clinical examination tests have been described for lesions in this area. The authors described the SLAP test for diagnosing unstable type II and type IV superior labral lesions (Fig. 15–2). In this test the arm is held abducted to 90 degrees with the hand fully supinated. Standing behind the patient the examiner places one hand on the shoulder with the thumb in the 6 o’clock position inferiorly (in the axilla). The exam-iner’s opposite hand is used to exert a downward force on the outstretched hand of the patient, creating a fulcrum of the thumb and shifting the humeral head in a superior direction. Crepitation, buckling, and pain represent a positive finding. Kibler (personal communication) described a maneuver in which the patient places the hand of the injured extremity on the ipsilateral hip. The examiner then pushes upward and forward on the elbow in line with the humerus, producing pain and crepitation when a SLAP lesion is present (Fig. 15–3). O’Brien and colleagues (1996) described the O’Brien test for SLAP lesions (Fig. 15–4). In this test the patient’s arm is placed in 90 degrees of forward flexion, full internal rotation, and cross-chest adduction. The patient is then asked to resist a downward force on the hand. This position winds the long head biceps around the humeral head, producing traction on the glenoid attachment of the biceps. Pain or buckling indicates a positive test. The O’Brien test will often be negative when a similar maneuver (arm forward flexed and adducted) is carried out with the arm in neutral or external rotation, presumably resulting from the release of traction on the biceps. O’Brien and colleagues feel that this test serves to differentiate symptoms attributable to the acromioclavicular (AC) joint from those attributable to a SLAP lesion because AC joint symptoms should occur regardless of the arm rotation as long as resisted cross-chest adduction is tested. Figure 15–1. The four types of superior labral lesions described by Snyder. Figure 15–2. Superior labrum anterior posterior (SLAP) test. The fourth examination test involves a “load and shift” maneuver. The examiner uses his thumb to exert a force in the direction of the area to be tested. For example, in SLAP lesions, the thumb is placed inferiorly so as to force the head into a 12 o’clock direction on the glenoid face. This is performed while the opposite hand of the examiner brings the flexed and neutrally rotated elbow in the opposite direction (Fig. 15–5). One additional test that it is often positive in SLAP lesions, and is particularly sensitive for rotator cuff pathology, is the Whipple test. The Whipple test, described by Terry Whipple (personal communication), is generally positive only in patients in whom there is a tear of the anterior portion of the supraspinatus tendon. For this test the arm is placed in 90 degrees of frontal flexion with the elbow extended and the palm facing toward the floor. The arm is adducted slightly so that the hand of the involved extremity is in front of the opposite shoulder (Fig. 15–6). The patient is then asked to resist a downward force applied to the hand. Pain and buckling represent positive findings, indicating a partial or even complete rotator cuff tear. A positive Whipple test in combination with one or more of the above provocative maneuvers indicates a variant of the subluxation-impingement syndrome or anterior-superior instability with associated secondary rotator cuff tearing (superior labrum anterior cuff, SLAC). Figure 15–3. Kibler test for anterior-superior labral tears. Figure 15–4. O’Brien test for SLAP lesions. Figure 15–5. Load and shift test to evaluate the superior labrum. Figure 15–6. The Whipple test for anterior supraspinatus tears. SLAP lesions are best managed using arthroscopic techniques. There are a number of surgical options available to accomplish repair of these lesions. Regardless of the technique employed, extreme care must be exercised in this area of the shoulder, as the suprascapular nerve courses in close proximity to the superior labrum–biceps tendon complex. Straying too far in a medial direction puts this nerve at risk. Also, because of the anatomic constraints in this area, care must be taken to avoid injuring the articular cartilage of the glenoid, which can occur when drilling the pilot hole for suture anchors or bioabsorbable tacks. Repairs fall into three basic categories. Absorbable devices such as the Suretac, transglenoid (Caspari) techniques with absorbable sutures, and suture anchor techniques can all accomplish reapproximation of the superior labrum–biceps tendon complex. The initial step, regardless of technique, is to first accurately define the lesion and debride the frayed and damaged soft tissues. If repair is indicated, abrasion of the superior glenoid neck beneath the tear is required (Fig. 15–7). Use of a bioabsorbable tack is occasionally employed by the authors. Using this technique, a cannulated drill bit and guide wire are inserted through the labrum into the glenoid neck. Alternatively, the drill can be used without the guide wire in place and a hole drilled in its proper position. The guide wire then can be used separately to spear the soft tissue prior to placement of the guide wire into the previously drilled hole. The optimal portal for Suretac placement is in the anterior superior corner. After the guide wire is passed through the soft tissues and into the previously drilled hole, the Suretac is passed over the guide wire and into the bone using a driving device, securely repairing the superior labrum–biceps tendon complex. These steps can be repeated using a posterior-superior portal with placement of a posterior Suretac when necessary (Fig. 15–8). Figure 15–7. Debridement of superior labral tissue and abrasion of the underlying glenoid neck are carried out prior to stabilization. • Spinal needle localization using an outside-in technique will assist in the determination of the best position and angle of insertion for the anterior-superior working portal.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree