26
Wrist Instabilities
Shrikant J. Chinchalkar and Joey G. Pipicelli
Osseous Anatomy
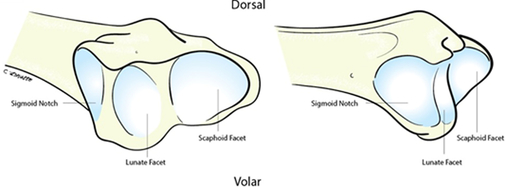
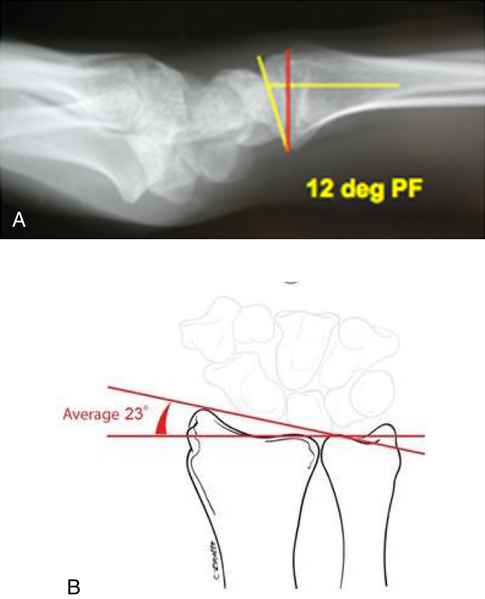
The wrist consists of the distal radius and ulna forming the distal radioulnar joint. The distal radius is typically tilted in anterior/posterior (A/P) plane by an average of 11° (Fig. 26-1, A) and radioulnar plane by 23° (see Fig. 26-1, B). The distal radius is composed of two fossae—a rectangular and shallow fossa for the articulation of lunate, and a deep triangular fossa for the scaphoid (Fig. 26-2). The distal surface of the ulna is covered by the triangular fibrocartilage complex (TFCC). The proximal carpal row is formed by the scaphoid, lunate, and triquetrum, whereas the distal carpal row is formed by the trapezium, trapezoid, capitate, and hamate. The joint formed by both these rows is the midcarpal joint. The midcarpal joint has three articulations: lateral, central, and medial. The lateral segment of the midcarpal joint is formed by the convexity of the distal pole of the scaphoid articulating with the concavity formed by the trapezium, trapezoid, and lateral aspect of the capitate. The central portion of the joint is formed by the proximal concavity of the scaphoid and lunate and distally by the convexity of the head of the capitate and the proximal pole of the hamate representing a “ball and socket” articulation. Medially the joint is formed by the articulation of the hamate and triquetrum. The midcarpal joint is highly synovial, thus allowing for maximal motion in all the planes. The scaphoid bridges both proximal and distal carpal rows. The pisiform, a sesamoid bone, is in the substance of the flexor carpi ulnaris (FCU) tendon, which articulates with the triquetrum. The proximal carpal row has been termed as an intercalated segment between the distal carpal row and the radius. The bones of the proximal carpal row move directly in response to the muscular force regulated by the ligaments that connect to the forearm and the distal carpal rows.1–4
Ligamentous Anatomy
The ligamentous structures are divided into extrinsic, intrinsic, palmar, and dorsal.5 The palmar extrinsic ligaments arise from the distal radius and ulna, and they connect to proximal and distal carpal rows. These ligaments are labeled in accordance with their length and insertion.
Palmar Ligaments
The radioscaphocapitate (RSC) is the radial most ligament originating from the radial styloid, and it traverses across the distal pole of the scaphoid connecting to the waist of the capitate. This ligament blends into the ulnocapitate (UC) ligament arising from the ulnar side. The RSC ligament is a primary radial stabilizer of the wrist and resists ulnar translation of the carpus over the radius. Lateral to the RSC ligament, the radioscapholunate (RSL) ligament provides neurovascular supply to the carpal bones and has no contribution to carpal stability. Lateral to the RSL ligament, the long radiolunate (LRL) and short radiolunate (SRL) ligaments offer primary resistance to lunate displacement, thereby preventing perilunate dislocation.6
Dorsal Ligaments
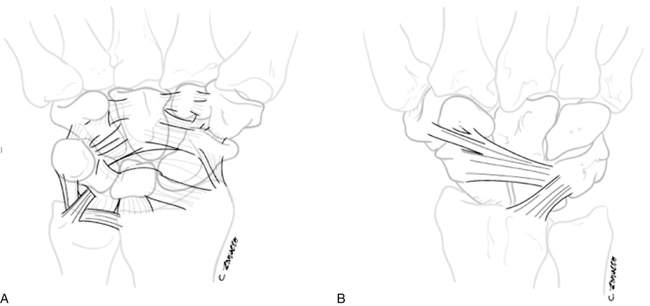
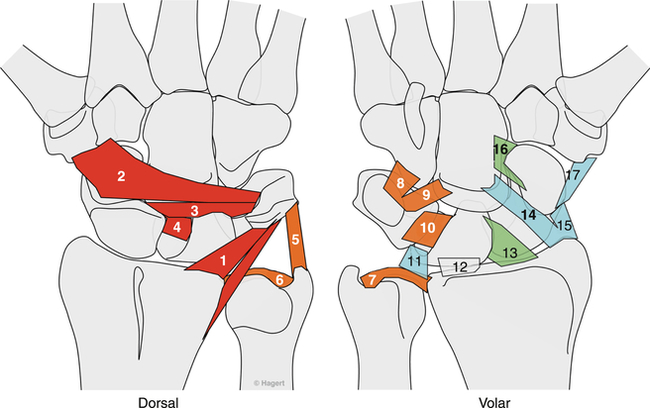
The dorsal intrinsic wrist ligaments are intracapsular and are not as well-defined and strong as the volar intrinsic ligaments (Fig. 26-3, A). The dorsal extrinsic ligaments of the wrist consist of dorsal radiocarpal (DRC) and dorsal intercarpal (DIC) ligaments (see Fig. 26-3, B). The DRC originates from the dorsal distal radius at Lister’s tubercle crossing, obliquely inserting on the triquetrum. The DRC ligaments prevent ulnar translation of the carpus. The DIC ligament originates from the triquetrum and extends towards the distal pole of the scaphoid and trapezoid where it inserts. This ligament provides stability to the midcarpal joint preventing dorsal dislocation of the capitate from the SL interval.
Normal Kinematics of the Wrist Joint
Understanding the complexities of carpal motion is based on various evolutionary studies that identified the instability patterns of the wrist. Navarro7 originally proposed the column theory. He suggested that the carpus was made up of three columns: central, radial, and ulnar. This column theory was later modified by Taleisnik.5 Other studies including work by Lichtman, et al.2 identified the four-unit concept, whereas Linscheid, et al.1 introduced a slider crank mechanism of the scaphoid. Linscheid, et al.1 also identified that regardless of the previously published studies illustrating the normal kinematics, the scaphoid maintains an average of 47° of flexion orientation in relation to the lunate and radius on lateral radiograph. The SL ligament plays an important role in neutralizing the flexion tendency of the scaphoid under physiologic loads. Gillula and Weeks8 identified that there is a distinct parallelism between the curvatures of the proximal and distal carpal rows on A/P radiograph. The proximal carpal row’s behavior during flexion/extension or radio/ulnar motion is based on its central placement between two rigid structures (that is, distal radius proximally and stable distal carpal row distally).
The motion of the carpal bones during flexion/extension and radial/ulnar deviation of the wrist is extremely complex. The motion of the proximal carpal row is dependent on the compressive loads placed by the distal carpal row. The musculotendinous units inserting distal to the distal carpal row produce this physiologic load on the carpus. Having normal anatomic relationship of the proximal carpal row structures along with the radius is critical for normal functioning of the wrist joint to occur.9
Flexion/Extension Motion
During extension of the wrist, the lunate extends and translates palmarly, whereas the capitate rotates dorsally.10 The palmar radiolunate ligament prevents excessive rotation of the lunate, preventing dorsal intercalated segmental instability (DISI). When the wrist is flexed, the lunate translates dorsally and the capitate rotates palmarly. The DRC and DIC ligaments prevent excessive rotation of the lunate, preventing volar intercalated segmental instability (VISI).
Motion of the Carpus during Gripping
Studies on load distribution during gripping activities have demonstrated that 80% of the load is transmitted on the radiocarpal joint and 20% on the ulnocarpal region, especially when the radioulnar relationship is in neutral ulnar variance.11 Out of the 80% radial load, 60% of the load transmission is on the scaphoid, whereas 40% of the load is transmitted on lunate. The load variation changes proportionately, either negative or positive, if ulnar variance is present. In neutral ulnar variance, the forces produced by the flexors and extensors are transmitted from the digits to the distal carpal row upon gripping and then through the proximal pole of capitate to the SL interval. A radiologic investigation using a classic stress test by making a fist is recommended to diagnose partial SL ligament tears, especially in the carpal instability non-dissociative (CIND) category of carpal instability. (This will be discussed later in the chapter.) The carpal motion studies during gripping have shown that the scaphoid demonstrates a tendency to rotate in flexion and pronation; the lunate rotates dorsally, whereas the triquetrum rotates in flexion. The rotatory tendency of the carpus during gripping activities suggest that the proximal carpal row (that is, the intercalary segment) moves together because of the intact SL and LT ligaments. In addition, the dislocation of the carpus is prevented by the palmar intrinsic, as well as the dorsal and palmar extrinsic ligaments.
Dart Throwing Motion
Other physiologic motions of the wrist that are commonly used in activities of daily living (ADLs) involve motion in an oblique plane. The majority of ADLs, such as combing hair or hammering a nail, are performed in a distinct manner. The motion of the wrist involves a combination of wrist extension in radial deviation and flexion with ulnar deviation. This motion has been coined as a dart throwing motion (DTM).12 The International Federation of Societies of the Hand (IFSSH) Committee13 recommends the motion taking place at the wrist joint in the so-called DTM be called radial extension and ulnar flexion. In vivo investigation of length changes in carpal ligaments during DTM demonstrates that the palmar radiocarpal ligaments’ length decreased significantly, whereas the DIC ligaments inserting on the trapezoid lengthened, and the UL and DIC inserting on the scaphoid remained shortest in neutral wrist position. These findings also suggest that DTM does not cause greater loads on the carpal ligaments. In addition, the arcuate ligament (that is, RSC and UC ligaments) resisted excessive motion of the capitate contributing to the midcarpal joint stability.14 From a carpal motion point of view, the DTM, revealed minimal scaphoid and lunate motion when compared to pure radioulnar or flexion extension arc of motion.15–17 The muscles that produce DTM are the FCU and the ECU and ECRB and ECRL. DTM will be discussed further later in this chapter.
Muscular Contributions to the Motion of the Wrist and Their Effect on Carpal Stabilization
The motion of the wrist joint in flexion, extension, and radioulnar direction is dependent on various muscular contractions. The palmaris longus, FCR, and FCU produce flexion of the wrist. The digital flexors also contribute secondarily to the flexion of the wrist joint. The ECRB, ECRL, and ECU are the prime extensors of the wrist. Additionally, the digital extensors also contribute secondarily to the extension action at the wrist. Radial deviation is primarily dependent on the action of FCR and ERCL; in addition APL, because of its radial orientation, contributes to radial deviation of the wrist joint. Motion in ulnar deviation is a result of ECU and FCU contraction. The kinematics of the carpus in flexion/extension, as well as the radioulnar arc, were described in the previous section. Based on the kinematics, it is apparent that the deforming forces are produced at the distal pole of the scaphoid, resulting in the intercalary motion of the proximal carpal row. Cadveric studies by Garcia-Elias18 and Hagert, Forsegren, & Ljung19 on the effect on carpal alignment during loading of the muscles have shown that ECU contraction stresses the SL ligament, whereas FCU, FCR, and APL activity reduces the load on the injured SL ligament. In addition, Garcia-Elias18 identified that FCU and hypothenar muscle contraction produced dorsally directed forces on the triquetrun through the pisiform, which stabilized midcarpal as well as LT joint instability. Based on these cadaveric studies, the authors recommend that the proprioceptive training of these muscles would be beneficial in SL, LT, and midcarpal instabilities. These suggestions are based on cadaveric experimentations, and implementation in clinical situations needs further investigation.
Carpal Instability Classification
Attempts to simplify our understanding of carpal motion have led to the development of multiple classification systems of carpal instability.5,20–22 Perhaps the most widely-adopted classification system is the Mayo Classification,23 which classifies carpal instability into four major categories:
• Carpal instability dissociative (CID)
• Carpal instability non-dissociative (CIND)
• Carpal instability complex (CIC)
Carpal Instability Dissociative
Scapholunate Ligament Tears
SL instability occurs most commonly in young- to middle-aged populations and is typically a result of a fall on out-stretched hand (FOOSH). Patients with acute injury often present to the physician’s office with a painful and swollen wrist, which may be diffusely tender. With time, pain becomes more localized over the SL ligament dorsally. Clinical examination needs to be exhaustive and systematic. Palpation of maximal areas of tenderness should be noted, and if sharp pain is elicited by pressing on the area just distal to Lister’s tubercle, a SL ligament tear is a high probability.24 Evaluation of the wrist should always include radiographic evaluation. Radiographs will often demonstrate the following in the presence complete SL ligament tears:5,11,25–27
• A/P views may demonstrate a SL gap of greater than 2 mm to 3 mm (Fig. 26-4, A). This has been termed the Terry Thomas sign.
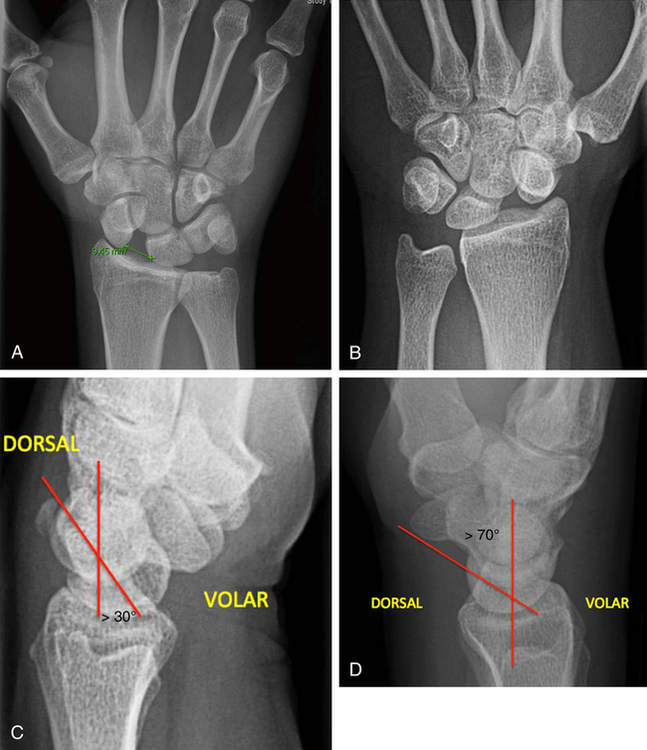
• Scaphoid may be palmarly flexed, giving the appearance of a ring on the AP film (see Fig. 26-4, B).
• Lateral views of the wrist may demonstrate the lunate dorsiflexed 15° or greater in relation to the capitate. This deformity is called a DISI (see Fig 26-4, C).
• Lateral views will also demonstrate an abnormal SL angle of more than 60° to 70° (see Fig 26-4, D).
• Long-standing instability may show degenerative changes to the radial styloid and at the capitolunate joint.
Luno-Triquetral Instability
• Lateral radiographs may demonstrate a VISI deformity, which is a capitolunate angle of greater than 30° (Fig 26-5).
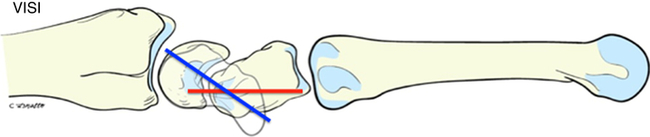
• Lateral radiographs will demonstrate that the lunate is more palmarly flexed.
Rehabilitation of Carpal Instabilities: Current Practice
The literature describing the rehabilitation of carpal instability is limited. Most rehabilitation programs described are based on author preference and experience.28–32 These rehabilitation programs are based on sound clinical reasoning; however, they have not been established as best practice, because clinical research studies are lacking. As such, carpal instability rehabilitation should be based on the stages of tissue healing when making clinical decisions regarding the length of time of immobilization, initiation of controlled protected motion, gradual tissue loading, and resumption of unrestricted hand use during functional activity, sport-, and work-related tasks. General rehabilitation following operative or non-operative management of wrist ligament injury should include the following:
• Through traditional means, including pharmacology, cryotherapy, compression, elevation, and cast/orthotic application
• Maintenance of range of motion (ROM) to the uninvolved joints
• Initiation of controlled, protected mobilization to the involved structures based on stages of tissue healing, observed intra-operative tension to repaired structures, and symptomology of the patient
• Avoidance of exercise or activity that may compromise tissue healing or place undue load to the healing/repaired structures
• Avoidance of generic wrist ROM and strengthening exercises
• Avoidance of aggressive ROM and excessive active ROM exercises
• Overall achievement of a stable wrist with functional ROM; functional ROM should be based on the work of Palmer and colleagues,13 which found that functional wrist ROM is between 5° of wrist flexion to 30° of extension, 10° of radial deviation, and 15° of ulnar deviation
Innovative and Emerging Approaches to Carpal Instability Rehabilitation
The term proprioception has been used since the early twentieth century to describe our body’s regulation of posture, balance, joint stability, and audiovisual-motor coordination.33 Our body maintains appropriate proprioceptive feedback through homeostasis. Homeostasis is defined as a dynamic process by which an organism maintains and controls its internal environment despite disturbances from external forces.34 The body is composed of many systems that operate automatically and subconsciously to maintain a homeostatic state.35
The term sensorimotor function was adopted by the participants of the 1997 Foundation of Sports Medicine Education and Research workshop in order to describe the sensory, motor, and central integration and processing components involved with maintaining joint homeostasis during movement.36 This was an attempt to recognize the portion of proprioceptive research dealing with only joint control.
The process of maintaining joint control and stability is accomplished through the relationship between the static and dynamic joint stabilizers. Ligaments, joint capsule, cartilage, and joint articulation bony geometry comprise the static stabilizers.37–39 Dynamic contributions to joint stability arise from the skeletal muscles that cross the joint structures. If there is a disruption in the static stabilizers of a joint, the dynamic joint stabilizers must work harder and become smarter and stronger in order to provide enhanced joint stability. However, in order for this to occur we must optimize ligamentomuscular reflexes.
Ligamentous and Muscular Reflexes, Proprioception, and the Wrist
The existence of mechanoreceptors in the ligaments of the wrist was first identified by Petrie, et al. in 1997.44 Since this time, there have been numerous studies on the innervation of the various wrist ligaments.20,40,41,45–47 These studies found that nerve endings in the various wrist ligaments are predominately located close to the ligament insertion into bone. This ensures firing of the mechanoreceptors only at the extremes of joint motion as the collagen fibers within the ligament have higher stiffness at their insertion into bone.48 Mechanoreceptors are also found in the DRC and DIC ligaments in the pliant epifascicular regions where they can be readily stimulated and able to provide information throughout the range of wrist motions.20,42 Interestingly, the ligaments of the radial and volar wrist ligaments have little to no innervation. However, the dorsal and triquetral wrist ligaments (DRC, DIR, dorsal SL, palmar LT, and triquetrocapitate/hamate ligaments) are the most densely innervated.40,49 What does this mean? The dense mechanically important ligaments that are designed to withstand axial loads are located in the radial column of the wrist. The sensory important ligaments are the dorsal wrist ligaments and ligaments emerging from the triquetrum and should be regarded as key elements in the generation of proprioceptive information required for adequate neuromuscular wrist control (Fig. 26-6).50
Dart Throwing Motion
DTM refers to the motion pattern commonly used during ADLs and functional tasks. Palmer and colleagues13 found that most tasks are performed in a plane from 40° of wrist extension and 20° radial deviation to 0° of flexion and 20° of ulnar deviation. Biomechanical studies of this motion pattern demonstrate that radiocarpal motion is minimized while most of the motion is occurring at the midcarpal joint.51–53 The relationship this movement pattern has on tension placed to the scapholunate interosseous ligament (SLIL) has also been studied. The results show that the DTM pattern of the wrist produces minimal elongation and thus minimal tension to the volar and dorsal SLIL.54,55 The clinical implications to hand therapy rehabilitation are that practice-guidelines can be developed implementing early-controlled motion utilizing the DTM pattern following partial SLIL injuries, SL repairs, or potentially other reconstructive procedures. Orthotic application can be utilized to ensure that wrist motion is within the arc of the DTM pattern of movement (Fig. 26-7). Caution must be used in implementing this type of controlled mobilization pattern following partial SLIL injuries and surgical procedures because no studies have determined the optimal time to introduce this pattern of movement following injury or surgery. It is also unknown how long to restrict motion along the DTM path following injury.
Proprioceptive Reeducation to the Wrist
Ligamentous insufficiency within the wrist may distort proprioceptive responses altering the normal reflex mechanism. This has an effect on dynamic joint stability.56 Although proprioceptive reeducation is a relatively new rehabilitation concept applied to wrist instability, it is a well-established part of the treatment of the unstable shoulder, knee, and ankle joint.57–62
Hagert49 proposed a proprioceptive rehabilitation program for to the unstable wrist joint. The foundation of proprioceptive reeducation is based on identifying muscles that serve a protective function for the specific ligament deficiency and training those muscles to respond more efficiently to prevent injury. Hagert49 suggests that the three major proprioceptive senses that have therapeutic implications include kinesthesia, JPS, and neuromuscular rehabilitation.
Kinesthesia
Kinesthesia is the ability to sense motion of a joint or limb. This sense is primarily influenced by muscle spindles and secondarily influenced by skin receptors and joint receptors.63–68 In clinical practice, kinesthesia is measured as the smallest change in joint angle required to elicit conscious awareness of joint motion.48,69 The common terminology used in proprioception training is “threshold to detection of passive movement.”49 It has been suggested that the joint be placed at a certain angle and then slowly moved passively at a speed of 0.5° to 2° per second until the patient signals that limb motion occurs.49 The patient should be blinded during initial kinesthesia testing, because limb movement is greatly influenced by visual cues. Also, it may be advisable to use a professional training device (such as, Biometrics Upper Limb Exerciser∗) in order to precisely control the speed and degree of joint motion.49
Joint Position Sense
JPS is a separate entity from kinesthesia.70 To describe the differences between JPS and kinesthesia is beyond the scope of this chapter. However, be aware that they differ due to their central processing and interpretation in the brain.69
In proprioceptive retraining, JPS is defined as the ability to accurately reproduce a specific joint angle.49 This form of retraining can be done with visual cues or blinded, as well as with active muscle contraction or through passive motion. Simply, JPS is when the patient is instructed to move the involved wrist to a predetermined joint angle established by using goniometry. This can be performed actively by the patient or passively by the therapist slowly moving the wrist until the patient identifies when the target position is reached. Hagert49 suggests beginning JPS with visual cues progressing to vision occluded exercises as tolerated by the patient. Patient progress and accuracy can easily be recorded simply by using a goniometer
Neuromuscular Rehabilitation
Hagert49 suggests that the purpose of neuromuscular wrist rehabilitation is to:
• Regain synchronous and balanced wrist motion following instability
• Use dynamic muscular compression to compensate for ligamentous insufficiency
• Promote ligamentous-friendly muscle contractions to provide joint protection and stability
The design of a neuromuscular rehabilitation program must be custom-tailored for each patient based on which structures are injured or operatively repaired. Furthermore, these techniques should be applied with caution, monitoring the patient’s response. As therapists we must ensure that we are not compromising wrist stability; thus, we should monitor for pain, swelling, and signs of instability. The components of a neuromuscular rehabilitation program that may be beneficial include, isometric, concentric, eccentric, isokinetic, co-activation, and reactive muscle activation (RMA) exercises.49
Concentric and Eccentric Exercises: Muscles actively shortening and lengthening
Eccentric strengthening is designed to increase strength by applying load while physically lengthening the activated muscle. Eccentric exercises may be beneficial during rehabilitation of carpal instability due to the concurrent shortening on the antagonist muscle(s). For the wrist to produce synchronous motion the muscles must work together in harmony in order to produce joint equilibrium. Following ligamentous injury the muscles which cross the joint are often weak, resulting in a neuromuscular imbalance during dynamic exercise.49
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree