Wrist Implant Arthroplasty
Thomas Ebinger
Brian D. Adams
DEFINITION
The wrist is a common site for end-stage joint degeneration, particularly in patients with rheumatoid disease. Osteoarthritis and posttraumatic arthritis following distal radius fractures, scaphoid nonunion advanced collapse (SNAC), and scapholunate advanced collapse (SLAC) are other common causes for advanced arthritis.
The gold standard of treatment for severe wrist arthritis has historically been complete wrist arthrodesis. Although arthrodesis provides good pain relief and durability, it is associated with substantial functional loss, especially if both wrists have arthritis.1,9,13
Total wrist arthroplasty is a motion-preserving alternative to arthrodesis that provides excellent pain relief. Sufficient motion and strength is retained for activities of daily living.
Preservation of wrist joint motion is of particular importance for patients who are debilitated by arthritis affecting multiple joints and those with specific joint motion requirements.9
Similar to arthroplasty in other joints, early wrist arthroplasty implants had poor long-term survivorship.2,3,7
Wrist arthroplasty has continually improved since the introduction of articulated implants more than 40 years ago. Advancements in design include distal component fixation being primarily within the carpus and not the metacarpal; intercarpal fusion to provide broad, solid support for the component; screw augmentation for carpal component fixation; minimal bone resection; preservation of the wrist capsule; cementless fixation; a broad semiconstrained ellipsoid articulation; and an option to preserve the distal radioulnar joint (DRUJ).
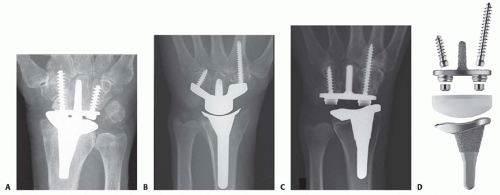
FIG 1 • A-D. Total wrist arthroplasty implants (from left to right): Re-Motion (Small Bone Innovations), Maestro (Biomet), Universal 2 (Integra LifeSciences), and Freedom (Integra LifeSciences).
Through improved materials, designs, and fixation techniques, total wrist arthroplasty has emerged as a viable option for selected patients with end-stage wrist arthritis.
Regardless of the desire for arthroplasty, patients must commit to a lifetime of restricted activities to obtain a durable outcome.
There are currently three total wrist implant systems in the United States: Re-Motion (Small Bone Innovations, Inc., Morrisville, PA), Maestro (Biomet, Warsaw, IN), and most recently Freedom (Integra LifeSciences, Plainsboro, NJ) (FIG 1). The Freedom wrist system evolved from its predecessor, the Universal 2 (Integra LifeSciences).
The Re-Motion wrist offers a mobile bearing attached to the carpal component that theoretically improves motion and load transfer, thus reducing stresses known to contribute to loosening.
The Maestro allows complete resection of the proximal carpal row and has a polyethylene surface proximally. The system is also approved for hemiarthroplasty using the distal component alone.
The Freedom wrist is the newest design, with a more anatomic articulation that provides physiologic wrist motion, improved bone fixation, and precise instrumentation.
ANATOMY
The wrist joint consists of the distal radial articular surface, distal ulna, triangular fibrocartilage complex (TFCC), eight carpal bones arranged in two rows (proximal and distal), and five metacarpal bases.
There are four major wrist articulations: radiocarpal (and ulnocarpal), midcarpal, carpometacarpal (CMC), and distal radioulnar joints.
In addition to the wrist capsule, multiple interosseous, intrinsic and extrinsic ligaments provide joint stability, with intrinsic ligaments referring to those between carpal bones and located primarily within the joint and extrinsic ligaments located within the joint capsule.
Normal radiographic parameters of the distal articular surface of the radius include 11 degrees of volar tilt, 22 degrees of radial inclination, and 11 mm of radial height.
Ulnar variance refers to the length of ulna relative to the radius, with positive variance indicating the ulna is longer. Approximately 70% of the population is ulnar neutral.
The sigmoid notch of the distal radius provides the radial articulation for the DRUJ. The DRUJ is stabilized by dorsal and volar radioulnar ligaments. Current implant systems are designed to preserve both the joint surfaces and ligaments of the DRUJ.
The center of wrist motion is located near the center of the head of the capitate.
PATHOGENESIS
Severe wrist arthritis is commonly caused by rheumatoid arthritis.
Early rheumatoid arthritis begins with minor joint erosions at synovial reflections such as the scaphoid waist and fovea of the ulnar head.
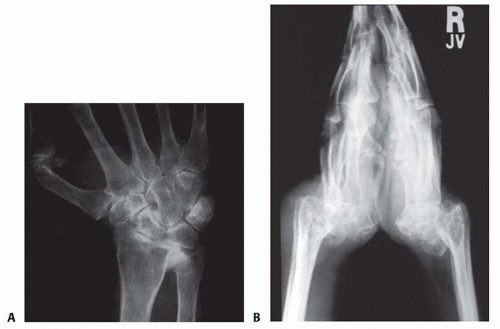
Progression of rheumatoid arthritis results in radial deviation and ulnar translocation of the carpus (FIG 2A), followed by carpal supination and volar subluxation (FIG 2B).
DRUJ deformity is very common in rheumatoid arthritis, resulting in dorsal subluxation of the ulna, often referred to as caput ulna.
Progression of rheumatoid disease may cause substantial ligament damage and bone erosion resulting in wrist deformity and decreased function.
Posttraumatic arthritis may develop years after an intraarticular distal radius fracture or fracture-dislocation of the carpus. In regard to implant arthroplasty, a malunion of the radius presents additional surgical challenges, but with proper planning and technique, a successful outcome is possible.
SNAC and SLAC wrist conditions are the most common causes of nonrheumatoid wrist arthritis, often with predictable degenerative patterns but only modest deformity.
NATURAL HISTORY
End-stage wrist arthritis, no matter the cause, is a painful condition resulting in progressive stiffness and diminished function.
In addition to pain and functional loss, deformity may be a cosmetic concern for patients.
Inflammatory arthritis may cause severe deformity and bone loss, precluding wrist implant arthroplasty.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history should confirm the presence of substantial pain that indicates the need for wrist arthroplasty.
Age, activity desires, hand dominance, presence of contralateral wrist arthritis, use of walking aids, and occupation are important factors in the preoperative assessment.
In rheumatoid patients, disease activity should be optimally controlled medically prior to surgical treatment because highly active disease reduces the durability of an arthroplasty.12
Lower limb surgery, such as total hip or knee arthroplasty, should be done prior to wrist replacement surgery to avoid weight bearing through the wrist implant during rehabilitation.
The ideal candidate for total wrist arthroplasty is an elderly patient with a low-demand lifestyle who desires pain relief
and can accept modest motion and strength and be willing to avoid stressful use.
Younger patients may qualify for wrist arthroplasty if activities can be modified, particularly when the nondominant wrist is involved.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard posteroanterior (PA), lateral, and oblique views of the wrist are adequate to assess the extent of disease, alignment, and bone stock.
In patients with rheumatoid arthritis, cervical spine radiographs are indicated to assess for instability.
DIFFERENTIAL DIAGNOSIS
Rheumatoid arthritis
Posttraumatic arthritis
Osteoarthritis, including SLAC and SNAC wrists
Avascular necrosis (eg, Kienböck disease)
Other inflammatory arthritis (eg, psoriatic)
NONOPERATIVE MANAGEMENT
Conservative treatment for severe wrist arthritis includes activity modification, bracing, nonsteroidal anti-inflammatory medications, and corticosteroid injections.
Failure of pain relief by conservative treatment or progression of deformity are indications for surgical treatment.
SURGICAL MANAGEMENT
Relative contraindications include poor bone stock, lack of wrist motor control, and wrist instability due to severely damaged tendons or ligaments,
Active infection locally or systemically is an absolute contraindication to total wrist arthroplasty.
Inflammatory arthritis should be well controlled medically prior to proceeding with surgical treatment.
Preoperative Planning
If severe bone loss or erosive disease is suspected but not confirmed by preoperative imaging, then the surgical permit should include other options such as arthrodesis. Proper instruments and devices should be available.
The proper implant size is estimated using PA and lateral wrist x-rays; however, final sizing is determined intraoperatively.
The DRUJ is assessed preoperatively for arthritis and instability.
A partial or complete resection of the distal ulna is planned when needed.
If the DRUJ is unaffected, then the DRUJ is not exposed.
Positioning
The patient is positioned supine with the affected limb resting on a hand table.
A padded tourniquet is placed on the upper arm.
Prophylactic antibiotics are administered intravenously.