Chapter 8 Whiplash-Associated Disorders of Joints and Ligamentous Structures
Trauma from whiplash can cause joint and ligamentous disorders of the cervical spine. When the rapid stretch of the spinal muscles fails to protect the vulnerable cervical articulations, injury and, more commonly, dysfunction occur. Left untreated, these disorders significantly prolong healing time and can result in chronic problems. The residuals of cervical spine injury are most commonly characterized by neck pain, restricted motion, and headaches. In addition, upper extremity symptoms frequently present. Conditions that produce recognizable signs and symptoms are not entities but rather syndromes.1 This chapter discusses several syndromes related to whiplash-associated disorders of the cervical zygapophyseal joints and associated ligaments.
Stability of the Cervical Spine and Whiplash Injury
The wide range of motion of the cervical spine makes stability problematic and predisposes the neck to traumatic injury.2 When the physiological limits of cervical structures are exceeded, disruption of the soft tissues of the neck occurs. When the muscles of the cervical spine, which offer the first line of defense from whiplash injuries, are unable to compensate for the rapidity of head and torso movement caused by the acceleration forces generated at the time of impact (see Chapter 3), ligamentous structures may be injured along with dysfunction and damage to cervical articulations.
Cervical Joint Sprain
Cervical joint sprain is noted when there is ligamentous and capsular damage, which may be evident on functional imaging. (See Chapter 5.) Differentiation of sprain from strain is indicated by the patient’s complaints. Muscle strain is indicated with pain on active motion when injured muscles contract. Pain at the end range of movement with passive motion induced by the clinician indicates joint sprain. (See Chapter 4.) Joint sprains are divided into four categories according to severity of the ligamentous damage. A mild sprain is characterized by only a few torn fibers, and the problem quickly resolves in a few days. A moderate sprain exhibits more severe tearing of the fibers, but the ligament remains intact. A severe sprain results in complete tearing of the ligament either from its attachment or within the ligament itself. A sprain or fracture occurs when a fragment of bone (avulsion) is torn from the ligamentous attachment.3 Functional imaging is necessary to determine the severity of ligamentous damage. (See Chapter 5.)
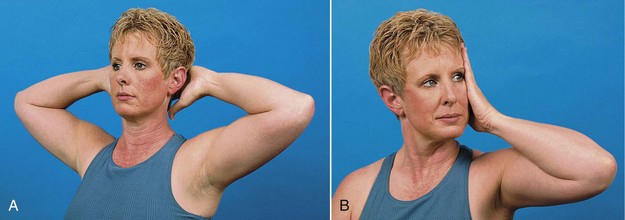
The inflammatory reaction from a ligamentous sprain can produce scar tissue that is less elastic and less functional if inflammation persists. Immobilization of joints and/or functional inactivity in mild to moderate cervical joint sprain is not recommended, as it can cause post-traumatic joint stiffness. The patient should be encouraged to move within the normal range of movement while avoiding excess movement. If a cervical collar is recommended, it should not be designed to restrict total movement but used to prevent further injury when riding in an automobile or when the patient complains of extreme fatigue in the cervical region. Isometric neck exercises can be introduced within 2 weeks of injury (Figure 8-1), and patients should be encouraged to return to their normal activities as soon as possible. Repair of injured capsular and ligamentous tissue is slow, taking up to 6 to 8 weeks. During this period, the patient must be careful to avoid overstretching the damaged ligaments, without restricting the joints from their normal range of movement. The Quebec Guidelines for Whiplash Associated Disorders recommend a multimodal approach to management (see Chapter 6) and suggest that the patient be instructed to repeat active cervical movements, within a comfortable range.4
Whiplash-Associated Joint Dysfunction
Various terms are used to describe joint dysfunction. The term “subluxation” or “fixation” is used by chiropractors, “joint dysfunction” or “somatic dysfunction” by osteopaths, and “spinal stiffness” by physical therapists. Some manual medicine practitioners prefer “joint blockage.” The common feature of these terms is that they refer to hypomobility (restricted motion) of the joints. Cervical joint dysfunction, including subluxation following whiplash, may take the form of simple joint restriction or, more likely, be accompanied by hypermobility in other motion segments. It is critical that hypermobile segments be differentiated from those with restricted motion. It is not rational to introduce forceful manipulation at the level of spinal segmental hypermobility, which can create further damage to sprained articulations. Subluxation has been defined by chiropractors through a rigorous consensus process as a motion segment in which alignment, movement integrity and or physiological function are altered although joint surfaces remain intact.5 Manipulation is not appropriate for all subluxations, and the medical use of the term often refers to an unstable segment (nonmanipulable subluxation) that may require a surgical procedure. It is important to differentiate between restricted joint motion and hypermobile motion segments because the therapeutic approaches to these syndromes are not the same. On a continuum of segmental motion, manipulation is appropriate for articulations with restricted motion, whereas on the other end of the spectrum, hypermobile and unstable segments require a stabilizing approach. Hypermobility has been described as the mobility of a motion segment that is excessive but not so extreme as to be life threatening or require surgery. Instability, on the other hand, is more severe and may require surgery if life threatening or if the patient is exhibiting neurological deficits attributable to the unstable segment.6 Functional imaging is useful if clinical findings suggest instability. (See Chapter 5.) The biomechanical injuries to joints and ligaments that result from whiplash commonly seen clinically tend to follow characteristic patterns that are recognizable as subluxation syndromes. The torque and lofting of the head produced by the whiplash action tends to produce hypomobility and subluxation of the upper cervical and lower cervical articulations, with hypermobility common at the apex of the curve in the mid cervical region where ligaments are stretched. Radiographically degenerative changes that occur following whiplash injury suggest that the greatest amount of soft tissue injury occurs at the C4-C5, C5-C6 motion segments. Jaeger’s report7 on 11 cervicogenic headache patients related to whiplash noted that tenderness and misalignment around the transverse process of C1 was the most frequent finding. Clinically, blocked movement of spinal motion segments is seen anywhere in the spine with whiplash injuries,3,8 but upper cervical subluxations7 are most common followed by restriction at the C7-T1 spinal motion segment, and first costovertebral articulations.3
Clinical Indicators of Cervical Subluxation
Clinical indicators of subluxation outlined by the Medicare Benefit Policy Manual (Box 8-1)9 include palpatory and radiographic findings. Radiographic and other imaging indicators of subluxation can be found in Chapter 5. Specific palpatory findings along with functional radiographs give the most useful clinical indications of subluxation of the zygapophyseal joints of the spinal motion segments.
Box 8-1
From Medicare Benefit Policy Manual, Chapter 15. Covered medical and other health services. http://www.cms.gov/manuals/Downloads/bp102c15.pdf
Diagnostic Criteria for Detection of Cervical Subluxation
Palpatory Findings Indicating Cervical Subluxation
Static palpation for alignment, tenderness, tone, and texture of the bony and soft tissue structures of the neck provides valuable information in the post-whiplash patient.10 Palpation for tenderness relies on the patients’ pain response and their verbal confirmation that the site is a pain generator. This alone is not a valid indicator for manipulation, as pain and tenderness can be caused by multiple disorders, including sprain or strain, neoplasia, and fractures.
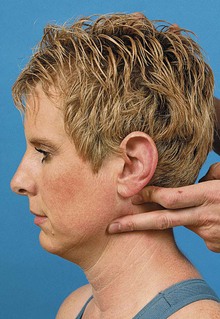
Cervical muscle tone and texture is palpated with the patient supine to promote optimal relaxation in injured structures10 (Figure 8-2). Palpation is a skill learned only through patience and perseverance. The ability to differentiate abnormal from normal tissue characteristics and aberrant motion is essential for identification of manipulable lesions. The art of manipulation is easier to master than the determination of where and how to perform this procedure,11 but caution is advised when using long lever procedures because the forces generated can easily cause injury.

Figure 8-2 Cervical muscle tone and texture are palpated with the patient supine to promote optimal relaxation.
Palpation of bony landmarks must take into consideration the possibility of osseous anomalies when assessing symmetry. The least pressure possible provides more information and prevents pain that can induce protective muscle splinting.11 Surface anatomy and osseous landmarks of the cervical spine are outlined in Table 8-1.
TABLE 8-1 Surface Anatomy and Osseous Landmarks of the Cervical Spine
| Landmark | How to Locate | Clinical Significance |
|---|---|---|
| External occipital protuberance (EOP) | Posterior: Midline projection of posterior aspect of skull at junction of head and neck. | A reference landmark for manipulative contact points lateral to EOP used with occipital (C0-C1) subluxations. |
| C2 spinous process | Posterior: First bony point palpated in midline inferior to EOP. | A reference landmark and contact point for manipulation. Tender with spinal fractures, infections, sprain/strains, neoplasia, and subluxations. |
| C6 spinous process | Posterior: Easily palpated in cervical flexion; moves (anteriorly) away from palpating finger during cervical extension. | Commonly used as a reference landmark and contact point for manipulation. |
| C7 spinous process | Posterior: Commonly the most prominent spinous process in this region. (T1 in some individuals). C7 moves on T1 during cervical flexion and extension. | Reference landmark and contact point for manipulation. Tender with spinal fractures, infections, sprain/strain, neoplasia, and subluxations. |
| Cervical facet joints | Posterior: Palpated 1.5-2 cm lateral to spinous processes. | Tenderness of soft tissue over these areas with common with joint sprain/strain, and subluxations. |
| C1 transverse process | Lateral: Palpated between mastoid process and angle of the jaw. | Commonly used as a contact point for manipulation. Tender with subluxation, sprain/strain. |
Modified from Scaringe JG, Faye LJ: Palpation: the art of manual assessment. In Redwood D, Cleveland C, editors, Fundamentals of chiropractic, St Louis, 2003, Mosby, 211-237.
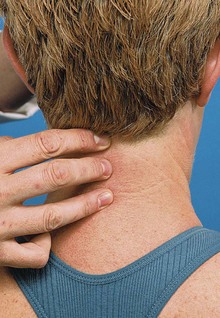
Palpation for flexion, extension, or rotation alignment of C1 in relation to C2 evaluates the C1 transverse process to mandible distance (Figure 8-3). Lateral flexion alignment of the atlanto-occipital articulation employs the inferior tip of the mastoid to C1 transverse process distance (Figure 8-4). Rotational and lateral flexion alignment at the atlantoaxial articulation can be palpated by comparing the bilateral relationship of the C1 transverse processes to the C2 articular pillars (Figure 8-5). Palpation for the alignment of the spinous processes in the lower cervical spine is conducted with the patient in the sitting position with the head flexed (Figure 8-6).12
Palpation for segmental motion includes evaluation of the discrete short-range movements of a joint that are independent of the action of voluntary muscles. This is determined by springing each vertebra in the neutral position (joint play), or at the limit of its passive range of movement (end feel), in addition to segmental range of motion. Joint play in the articulations of the cervical spine can be evaluated with the patient seated or in the supine position. In the supine position the patient’s head rests on the table, which is more comfortable when the patient is acute. Joint play and posterior-to-anterior glide are assessed in the cervical spine with the patient in the sitting position by bilaterally contacting the posterior joints with the palmar surfaces of the finger and thumb of the contact hand with the patient’s forehead supported by the stabilizing hand (Figure 8-7). Each individual motion segment is evaluated for a fluid posterior-to-anterior gliding motion along the horizontal plane. With the patient in the supine position, joint play and posterior-to-anterior glide are assessed by contacting the posterior joints with the fingertips (Figure 8-8). Lateral-to-medial glide may be assessed by contacting the posterolateral surface of adjacent vertebrae with the index fingers. One hand springs the segment toward the midline as the other hand stabilizes the patient’s neck.12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree