Volar Wedge Bone Grafting and Internal Fixation of Scaphoid Nonunions
Evan D. Collins
DEFINITION
The scaphoid is the most commonly fractured carpal bone in the wrist. Scaphoid fractures that fail to heal after 6 months of treatment are categorized as nonunions and represent about 5% to 10% of all scaphoid fractures.
Untreated nonunions reportedly lead to progressive arthrosis and wrist pain.6
Volar wedge bone grafting is an effective surgical technique in the treatment of certain scaphoid nonunions based on the following:
Location of the fracture
Degree of the deformity
Vascularity of the scaphoid
This general technique can also be adapted to increase its versatility.
ANATOMY
Nearly 80% of the scaphoid’s surface is covered by articular cartilage.6
Through ligamentous connections, the scaphoid serves as the bridge or link between the proximal and distal rows (FIG 1). Due to these strong tethers proximally and distally, it is highly susceptible to an acute fracture after a fall on an outstretched hand.18
Other key factors that influence scaphoid fracture healing are its tenuous vascular supply and its unique bony architecture.
The vulnerable vascularity of the scaphoid, especially the proximal pole, is well described in the literature.8,14,15,16,20 This is the result of the scaphoid’s retrograde blood supply, with approximately 70% of the vascular supply provided through the dorsal ridge vessel and 30% through branches to the scaphoid tubercle (at the level of the radiocarpal joint via superficial palmar branch perforators off the radial artery).
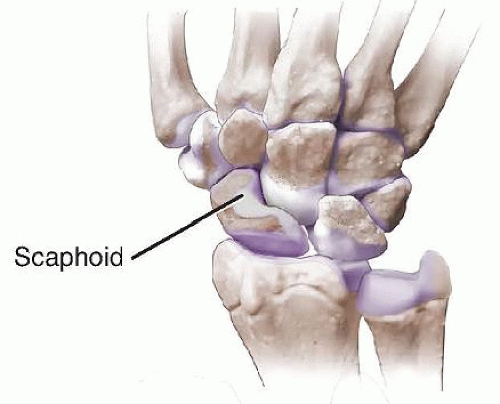
FIG 1 • Anatomy of the wrist joint. The scaphoid bridges the proximal and distal carpal rows and is largely covered by articular cartilage.
The complex geometry of the bone makes it difficult to anatomically reduce the bone fragments.
PATHOGENESIS
Although there may be a variety of reasons for the development of a scaphoid nonunion, a fractured scaphoid usually fails to heal for three primary reasons:
The fracture is either undetected or untreated within the first 4 weeks after the injury.
The location of the fracture is proximal, resulting in poor vascularity of the most proximal fragment.
The fracture is displaced more than 1 mm.
NATURAL HISTORY
Scaphoid nonunion advanced collapse (SNAC), described in the literature, is a predictable sequence of changes that occurs as a result of scaphoid nonunion leading to wrist arthrosis, often associated with pain and limitation of motion.4,5
In studying patients with painful wrists over a 15-year period to determine who will develop symptoms, it is evident that the incidence of symptomatic wrist pathology requiring reconstruction is significantly higher for scaphoid nonunions that have gone untreated.1
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient who presents with a scaphoid nonunion is usually a man between the ages of 18 and 35 years.
Unrecognized injuries in adolescence may present with pain related to early SNAC wrist arthrosis in the middle-aged adult.
Patients generally complain of wrist pain that limits range of motion or hinders activities such as push-ups, weightlifting, or simple daily tasks such as opening a door. Moderate to heavy pinch and grip pain have also been described.
A specific event resulting in the original scaphoid fracture years before is rarely cited by the patient on presentation.
Consistent physical examination findings include subtle tenderness in the region of the scaphoid tubercle or the anatomic snuffbox, limited wrist extension compared to the contralateral side, and localized pain on the radial side along the radiostyloid or scaphoid with loaded wrist extension. If arthrosis has developed, soft tissue swelling may be noted over the dorsal and radial wrist.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard radiographs include posteroanterior (PA), lateral, and scaphoid oblique 45- and 60-degree pronated views (FIG 2). Such views
Confirm the diagnosis
Provide information regarding displacement, angulation, shortening, and the presence of a “humpback deformity”
Reveal compensatory carpal instability, dorsal intercalated segment instability (DISI)
As part of a treatment algorithm, dividing scaphoid fracture nonunions into either proximal, middle, or distal is very helpful.
Other factors considered in diagnostic assessment include previous wrist fracture or sprain later becoming symptomatic; tenderness on the scaphoid tubercle or in the anatomic snuffbox; localized pain to the radial side of the wrist along the radiostyloid or scaphoid itself, with a loaded dorsiflexed wrist; and pinching and heavy grip pain.
Once the scaphoid nonunion is diagnosed, a computed tomography (CT) scan performed in the plane of the scaphoid helps define bony architecture. Sagittal and coronal images are particularly helpful in characterizing the nonunion site and its orientation, displacement, and degree of bone loss.
Scaphoid collapse (or humpback deformity) is most clearly determined by measuring the lateral intrascaphoid angle on the sagittal CT views.
Magnetic resonance imaging (MRI), especially when combined with intravenous gadolinium, is helpful in defining the presence or absence of osteonecrosis and any associated ligamentous or cartilaginous injuries. If osteonecrosis of the proximal fragment is seen, the surgeon should consider a vascularized bone graft10 (see Chap. 38) rather than the nonvascularized grafting procedure described in this chapter.
NONOPERATIVE MANAGEMENT
Surgery is generally indicated for established scaphoid nonunions that are displaced and symptomatic because of the strong likelihood that radiocarpal arthrosis may develop with this type of persistent nonunion.18,20
Nonoperative management may be appropriate for minimally symptomatic scaphoid nonunions. All factors should be taken into consideration when determining the most appropriate treatment: Scaphoid nonunion alone is not an absolute reason for surgery.12
SURGICAL MANAGEMENT
Volar wedge bone grafting is the preferred surgical technique for treatment of a scaphoid nonunion without osteonecrosis but with shortening, an increased intrascaphoid angle causing a humpback deformity, and concomitant carpal collapse. Although many scaphoid nonunions without deformity can be effectively treated with the described procedure, other approaches and grafting techniques that are less invasive may be an option, especially for proximal pole nonunions.2
Determining which bone graft is necessary depends on how much shortening is anticipated.3
The benefits of distal radius bone grafting include its location within the same surgical field and can be harvested as a vascularized or nonvascularized graft. One important disadvantage is the creation of a relatively large defect and stress riser within the distal radius. Also, it is not possible to obtain a bicortical or a tricortical piece of bone for a more structural bone graft.
Iliac crest bone graft may be harvested in large quantities and as a bicortical or tricortical piece of bone. It is relatively simple to procure and has a long history of success in such cases, a standard by which all others are currently measured. The disadvantages of this type of bone graft include a separate incision with associated morbidity as well as a reported risk of cutaneous nerve injuries. Also, it cannot be converted to a vascularized pedicle bone graft.
When an MRI reveals the presence of osteonecrosis, a vascularized procedure should be considered (see Chap. 38).14,15,20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









