Vascularized Bone Grafting of Avascular Scaphoid Nonunions
Alexander D. Mih
DEFINITION
Scaphoid fractures account for 60% of carpal bone fractures.
Nonunions occur in up to 15% of scaphoid fractures and often result from delayed treatment, inadequate immobilization, displacement of the fracture, or proximal pole involvement or in the setting of avascular necrosis (AVN).
ANATOMY
The blood supply to the scaphoid travels in a distal to proximal direction and emanates from the radial artery. Intraosseous vessels traverse the scaphoid to supply the proximal pole.
In about 30% of scaphoids, there is either a single or no vascular channel found reaching the proximal pole.
Studies of vascularity of the distal radius have identified several sources of vascularized bone graft available for nonunion treatment.
Animal studies of vascularized bone grafts have documented a significant increase in blood flow present when compared to nonvascularized grafts.
PATHOGENESIS
Without adequate blood flow, the normal bone healing response cannot be completed. The scaphoid fracture site fills with fibrous connective tissue and motion persists at the site of the fracture.
In some cases, the bone undergoes changes of AVN with cellular death, edema, and the eventual loss of trabecular architecture.
Studies have shown that in cases in which the trabecular bone pattern has been lost, union may be difficult if not impossible to achieve.
NATURAL HISTORY
Nonunion of the scaphoid severely alters the normal carpal biomechanics and subjects the cartilage to shear forces detrimental to its survival.
PATIENT HISTORY AND PHYSICAL FINDINGS
Often, patients recall injuring their wrists several years before developing pain severe enough to seek medical attention.
Patients usually complain of limited range of wrist motion and pain, often with grip or weight bearing. The patients have often significantly reduced their activity level due to persistent pain.
In most cases, the patient will experience tenderness to palpation at the anatomic snuffbox (FIG 1A), the radial styloid-scaphoid joint (FIG 1B), or the distal pole of the scaphoid (FIG 1C), which is palpable on the palmar side of the wrist.
Wrists with established scaphoid nonunions have an arc of motion that is significantly reduced from the uninvolved side, primarily in extension.
IMAGING AND OTHER DIAGNOSTIC STUDIES
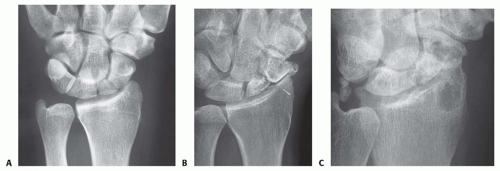
Standard radiographic studies include posteroanterior (PA), lateral, and scaphoid (ulnar deviation) views (FIG 2).
Classic radiographic findings begin at the radial styloid distal pole of scaphoid interface and proceed to involve the entire scaphoid fossa, the midcarpal joint, and eventually, the entire radiocarpal articulation.
Computed tomography (CT) is essential for determining union as well as for identifying patients in whom the normal trabecular bone pattern has been lost. Proximal pole sclerosis and absence of converging trabecular bone at the fracture site correlate to AVN.
Magnetic resonance imaging (MRI) is useful in evaluating the scaphoid for vascularity, although definitive determination of avascularity may be difficult. Although contrast-enhanced MRI has shown improved sensitivity over noncontrast studies in detecting AVN, it may not be effective in detected AVN in up to 25% of cases.
DIFFERENTIAL DIAGNOSIS
Ligamentous injury to the wrist
Wrist synovitis
Intraosseous ganglia
Primary AVN of the scaphoid
NONOPERATIVE MANAGEMENT
Nonoperative treatment is of limited usefulness for established nonunions.
Investigators have attempted the use of bone stimulators, which use either electrical stimulation or ultrasound.
There is little evidence in the literature supporting the use of these units for treatment of established scaphoid nonunions with AVN.
SURGICAL MANAGEMENT
A vascularized distal radial bone graft is indicated for scaphoid nonunions with and without evidence of avascularity.
Correction of a “humpback deformity” requires extensive mobilization of the pedicle when attempting the use of a dorsally sourced graft, and a palmar vascularized graft may be more appropriate.
For significant collapse, a nonvascular iliac crest graft may be required to create a compression-resistant construct.
When early degenerative changes are present, a radial styloidectomy should accompany the use of a vascularized distal radial graft.
The presence of more advanced degenerative joint disease or carpal malalignment is a contraindication to performing surgery to obtain bony union.
Preoperative Planning
Radiographs must be evaluated to rule out carpal instability or the degenerative changes frequently found in established nonunions. When there has been the development of dorsal intercalary segmental instability (DISI), over 50% of patients undergoing vascularized grafting will suffer failure to achieve union.
Positioning
The patient is placed supine on the operating table with the arm placed on an arm board.
Surgery is performed under tourniquet control.
Approach
Vascularized grafting may be carried out through a dorsal or palmar approach. Anatomic studies have shown that the dorsal irrigating vessels are further from the articular surface than irrigating vessels on the palmar surface of the radius.5,8,10 The palmar vessels have been shown in some anatomic studies to be of greater diameter.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree