Varus Derotation Osteotomy of the Proximal Femur
Alex L. Gornitzky
Wudbhav N. Sankar
A varus proximal femoral osteotomy is commonly used to treat a variety of abnormal conditions of the hip by realigning the femoral head within the acetabulum. This procedure can be used at any age but is seldom performed before 1 year of age. Although varus proximal femoral osteotomy may be done alone, it is commonly combined with other surgical procedures under the same anesthesia, such as adductor tenotomy, open reduction, and/or pelvic osteotomy. Intraoperative dynamic arthrography of the hip can be used to help determine the optimal position of the femoral head within the acetabulum, particularly if there is incomplete ossification of the proximal femoral epiphysis. The need for casting after proximal femoral osteotomy is determined by the stability of proximal femoral fixation, cooperativeness of the child, age of the child, or the need to stretch soft tissues that have been lengthened as an adjunctive procedure to the femoral osteotomy.
INDICATIONS/CONTRAINDICATIONS
A proximal femoral varus derotation osteotomy (VDO) is useful for the treatment of a wide variety of hip conditions including the following:
Coxa valga deformity
Developmental dysplasia of the hip (DDH)
Hip subluxation of nearly all etiologies
Spastic hip disease associated with cerebral palsy (CP)
Legg-Calvé-Perthes disease (LCPD)
VDO is also used for the surgical treatment of many other diseases, including hip subluxation or dislocation related to a variety of genetic and neuromuscular disorders too numerous to individually mention. In all of these conditions, in addition to the valgus deformity, VDO can be used to simultaneously correct deformities in other planes (derotation and flexion-extension). Although the exact manner in which the VDO is performed for a specific patient may vary, the principles are constant in each operative procedure. The goals of a VDO include improvement of hip motion, improvement in the distribution of forces across the hip to allow more normal hip development and growth, and prevention of premature degenerative articular cartilage changes.
VDO is relatively contraindicated in CP patients with long-standing hip dislocation, which is commonly associated with extensive articular cartilage erosion and flattening of the femoral head. If a malformed femoral head with articular cartilage erosions to subchondral bone is placed into the acetabulum, hip pain and motion may worsen, and further hip surgery is nearly always needed soon thereafter. Severe range-of-motion limitations, particularly lack of abduction, are also relative contraindications to VDO, unless the procedure is combined with aggressive soft-tissue releases. In ambulatory children and adolescents, it is preferable to not create excessive varus, as this may weaken the hip abductors sufficiently to cause persistent gait abnormalities. Therefore, preexisting
varus is another relative contraindication. Children with leg-length discrepancies also merit consideration, as the VDO itself will inherently cause further shortening. Finally, other contraindications to VDO include active joint infection and/or osteomyelitis or any other inherent bone disease that will limit the efficacy and safety of internal fixation.
varus is another relative contraindication. Children with leg-length discrepancies also merit consideration, as the VDO itself will inherently cause further shortening. Finally, other contraindications to VDO include active joint infection and/or osteomyelitis or any other inherent bone disease that will limit the efficacy and safety of internal fixation.
PREOPERATIVE PLANNING
The specifics of preoperative planning will vary based on the underlying diagnosis. One of the most common indications for VDO is in children with CP and spastic hip disease. Whereas children with DDH often have few or no medical comorbidities that may have an impact on surgical treatment with a VDO, those with hip dysplasia associated with CP and other neuromuscular disorders frequently have many coexisting medical conditions. Consequently, it is important to coordinate a multidisciplinary approach to care between anesthesia, pulmonology, cardiology, neurology, nutrition, and any other department, as indicated, to adequately and safely care for the child pre-, intra-, and postoperatively. For all patients, the parents should be informed that blood transfusion may be needed during or after the VDO. Typically, blood transfusion is not needed, but parents should be given the opportunity to provide donor-designated blood, if desired.
As part of single-event multilevel surgery (SEMLS), VDO in the CP population is frequently performed concurrently with other procedures. A growing body of literature suggests that this practice leads to improved outcomes due to fewer hospital admissions and streamlined periods of rehabilitation. Therefore, a key component of preoperative planning in neuromuscular patients is a thorough assessment for other maladies to be addressed at the same time. For further details on the surgical management of children with CP, please reference Chapter 14 on “Lower-Extremity Surgery in Children with Cerebral Palsy.”
Regardless of the indication for surgery, preoperative physical examination is important to help determine the planes and degrees of correction needed at the time of the VDO. Careful notation of hip range of motion prior to surgery is needed. Because performing a varus osteotomy on the proximal femur will result in loss of abduction and an increase in adduction, it is particularly important that the preoperative abduction be assessed. A concomitant adductor tenotomy is often necessary to restore some of the abduction that is lost by the procedure. Irrespective of the desired correction and disease process being treated, however, the amount of passive abduction present preoperatively (or after tenotomy) serves as the absolute upper limit for the amount of varus that can be achieved intraoperatively. A significant consequence of varus osteotomy is leg shortening. As the amount of shortening is affected by both the degree of varus and the size of the bone wedge removed, preoperative assessment for preexisting leg-length discrepancy may be indicated for further consideration during surgical planning.
Standard imaging studies for patients who are being considered for a VDO include an anteroposterior (AP) view of the pelvis and frog-leg lateral radiograph of the hip. Standard PACS software, which is widely available at most centers, can be used to measure the length and width of the femoral neck to help estimate the suitability for various sized implants. These views may also help the surgeon assess the degree of subluxation or dislocation present, the status of acetabular development, and whether the femoral heads can and will reduce into the acetabulum when the hip is abducted. If necessary, a dynamic hip arthrogram, done as the first stage of the VDO operative procedure, can be used to determine the exact position of the femoral head within the acetabulum, as well as to assess the lateral edge of the acetabulum.
Advanced imaging, including computed axial tomography (CT) and magnetic resonance imaging (MRI), may be necessary to evaluate the health of the femoral head and how amenable it is to reconstruction. Three-dimensional reconstructions can clearly show the bony anatomy of the femoral head and acetabulum, as well as acetabular version, to help the surgeon in deciding where acetabular coverage may be needed as part of the hip reconstruction procedure. These reconstructions can also be used to measure the degree of femoral anteversion present preoperatively in order to guide the amount of rotational correction needed through the VDO to address femoral version.
The most important part of preoperative planning for a VDO is determining how much you want to correct. The exact amount of correction will vary based upon the specific disease process and the goals of treatment. For example, in nonambulatory CP patients, the goal for the final neck-shaft angle is often between 90 degrees and 100 degrees. In ambulatory CP patients, that goal is typically 110 degrees. Conversely, in LCPD, it has been shown that 10 to 15 degrees of correction from the native neck-shaft angle is optimal.
Keep in mind what constitutes normal anatomy when assessing an individual’s specific deformity and the goals of correction:
The femoral neck-shaft angle is normally 135 degrees, ranging from 120 to 150 degrees, and is best measured with the hip internally rotated to compensate for femoral anteversion.
The neck-shaft angle is greater at birth (150 degrees) than at skeletal maturity (135 degrees).
Normal anteversion (45 degrees) decreases as children age, reaching approximately 10 degrees in boys and 15 degrees in girls by 8 years of age.
The following surgical technique for VDO is described using a cannulated blade plate system. Alternative implants such as proximal femoral locking plates or Altdorf plates may be employed to achieve equivalent corrections, as each (like a blade plate) is a fixed angle device. In certain cases of extremely poor bone density and/or revision osteotomy, there may be advantages to the use of locking plates in particular. The specific surgical technique for insertion of each of these implants varies slightly based on the individual implant design, but the principles of preoperative planning and osteotomy execution remain the same.
SURGICAL PROCEDURE
Positioning and Prepping
Although some surgeons prefer to perform a VDO with the patient prone, we prefer the patient to be positioned supine on a radiolucent operating table as this facilitates intraoperative imaging and also allows concomitant procedures (i.e., pelvic osteotomy) to be performed.
In patients with spastic CP, placement of an epidural catheter after general anesthesia is induced can help to diminish the need for intraoperative anesthetic medications and facilitate pain and spasm control postoperatively.
Alternatively, regional anesthesia (e.g., lumbar plexus block) can be utilized to help with postoperative analgesia.
A Foley catheter is utilized, if necessary, based on the use of an epidural and the planned length of the procedure.
If surgery is planned for only one hip, a roll can be placed under the thoracolumbar spine on the operative side to elevate that side of the pelvis about 20 degrees.
The entire leg and hemipelvis are prepped to midthoracic level, sterile drapes are placed, and prophylactic antibiotics are given.
Intraoperative Dynamic Examination of Hip
In cases of dislocation or subluxation, a dynamic examination of the hip may be performed under live fluoroscopy to determine if the femoral head reduces fully into the acetabulum or remains dislocated/subluxated.
If the hip is not reducible, then open reduction is recommended prior to osteotomy.
If the femoral head reduces into the acetabulum, then a 22-guage spinal needle is inserted into the hip joint.
A medial or anterolateral approach can be used, based upon surgeon preference.
Radiopaque dye is injected directly into the hip joint. The surgeon should aim to minimize extravasation.
The hip is placed through a full range of motion to allow for dispersal of the dye over the entire femoral head.
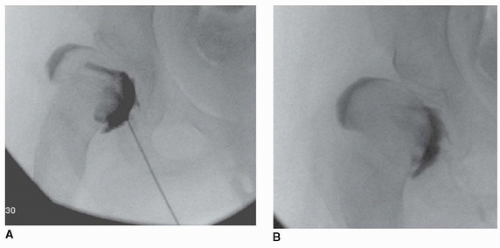
The hip joint may then be evaluated under live fluoroscopy to determine the congruency of the hip and the quality of the reduction based on the presence/absence of a medial or superior dye pool as well as the appearance of the cartilaginous lateral acetabulum (Fig. 17-1).
All things else being equal, the amount of abduction required to achieve full reduction and a congruent position of the femoral head in the acetabulum is the amount of varus correction that is required.
However, depending on the ambulatory ability of the patient and the specific disease process, it may be advantageous to avoid excessive varus (and its associated limb shortening and abductor weakness) and augment coverage through an acetabular procedure.
If there is limited abduction due to contracture of the hip adductors, lengthening may be indicated.
Hip arthrogram can also help determine the need for a pelvic osteotomy.
If there is insufficient lateral acetabular coverage once the femoral head is reduced, an acetabular surgical procedure may be done after the VDO has been completed.
Exposure
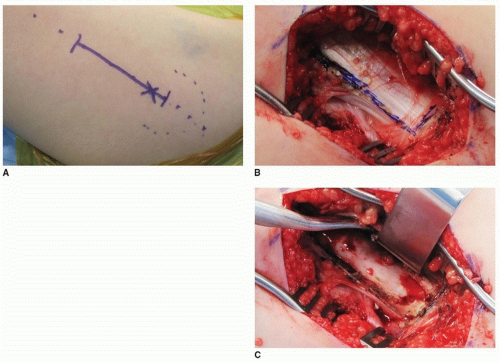
Palpate and mark the tip of the greater trochanter and vastus ridge along the proximal femur (Fig. 17-2A).
Skin incision is made in line with the proximal femur starting a few cm proximal to the vastus ridge and extending distally approximately 8 to 12 cm depending on the size of the patient and the intended implant.
The fascia lata is split in line with the fibers over the palpated lateral border of the femur.
The vastus lateralis fascia is incised longitudinally about 5 to 10 mm anterior to the intermuscular septum and is elevated atraumatically from the femur. Perforating vessels are identified and cauterized.
Proximally, the fascia of the vastus lateralis is opened anteriorly with the electrocautery along the vastus ridge, creating an L shape (Fig. 17-2B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree