Varicella-Zoster Virus Infections
Charles F. Grose
Chickenpox is the common childhood exanthem caused by the human herpesvirus varicella-zoster virus (VZV). Before varicella vaccine was recommended for all susceptible children in 1995, most children acquired chickenpox during early school years, thereby developing lifelong immunity. However, approximately 10% of young adults are susceptible to primary VZV infection because they did not contract chickenpox as children and have not received varicella vaccine. After a person recovers from chickenpox, the virus remains in a latent state in the dorsal root ganglion cells for decades. As immunity wanes in late adulthood, occasionally the virus reactivates and causes the dermatomal exanthem known as shingles or zoster. Zoster also occurs in some children who have had chickenpox, often in association with treatment with immunosuppressive chemotherapy and irradiation for acquired disease (e.g., leukemia and lymphoma).
THE VIRUS AND ITS PATHOGENESIS
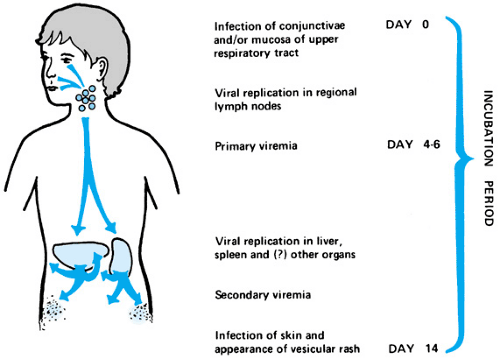
VZV is one of the eight known human herpesviruses. The other seven are herpes simplex type 1 (oral) and type 2 (genital), cytomegalovirus, Epstein-Barr virus, and the newly discovered human herpesviruses types 6, 7, and 8. The route by which primary VZV infection causes disease is illustrated in the schema for pathogenesis (Fig. 199.1). The interval between infection
and appearance of the vesicular rash (incubation period) usually is 14 to 15 days, with a range of 10 to 20 days. The initial site of infection is the conjunctivae or upper respiratory tract. Then the virus replicates at a local site in the head or neck for approximately 4 to 6 days. Thereafter, the virus is transmitted throughout the body during the primary viremia. After a second cycle of replication, the virus is released in larger amounts 1 week later (secondary viremia) and quickly invades the cutaneous tissues. As the virus exits the capillaries and enters the epidermis, characteristic vesicles of chickenpox appear on the skin.
and appearance of the vesicular rash (incubation period) usually is 14 to 15 days, with a range of 10 to 20 days. The initial site of infection is the conjunctivae or upper respiratory tract. Then the virus replicates at a local site in the head or neck for approximately 4 to 6 days. Thereafter, the virus is transmitted throughout the body during the primary viremia. After a second cycle of replication, the virus is released in larger amounts 1 week later (secondary viremia) and quickly invades the cutaneous tissues. As the virus exits the capillaries and enters the epidermis, characteristic vesicles of chickenpox appear on the skin.
The entire VZV genome was sequenced in 1986. For some time, VZV was thought to be an identical virus around the world. However, in 1998 and 2002, two mutant viruses were discovered, one in Minneapolis, Minnesota, and the second in Vancouver, Canada. Whether these viruses will spread more widely is unknown.
EPIDEMIOLOGY
Chickenpox is transmitted by virus in water droplets carried by air currents from infected children to susceptible individuals. Epidemiologic observation studies document that children in the late incubation period may be infectious 1 or 2 days before the appearance of the exanthem. They remain infectious through the first few days of the rash but probably no longer than the sixth day. Affected children can return to school when lesions have become encrusted. Susceptible children can also contract chickenpox from elderly persons with zoster, although the period of contagion appears to be much shorter.
In most communities in North America, Japan, and Europe, outbreaks of chickenpox occur annually from January to May. The fewest cases occur in August and September. The periodicity of chickenpox derives from bringing susceptible children together in school every autumn. The epidemiology pattern in the United States is changing because of the introduction of varicella vaccination programs in 1995. However, chickenpox will continue to be seen in North America in the foreseeable future because neither Canada nor Mexico has a national varicella immunization program. Moreover, varicella immunization will not be given in most countries of South America, Africa, or Asia (except Japan).
CLINICAL FEATURES OF CHICKENPOX
The characteristic feature of chickenpox is the vesicle. In healthy children, the exanthem develops over 3 to 6 days, usually beginning along the hairline on the face. Each lesion begins as a macule that progresses to papule and vesicle, then to a crusted vesicle. Subsequently, the rash emerges in successive crops over the trunk, then the extremities. Lesions in different stages of development are present throughout the first week. The rash is more confluent wherever the skin has been abraded previously, such as the diaper area.
The typical course of chickenpox is documented meticulously in U.S. children. Usually, the prodrome is mild, with malaise and low-grade fever. Once the pox lesions appear, the temperature rises, but rarely to more than 102°F. The average number of skin lesions ranges between 200 and 300 in the index case within a family. Secondary cases may have a more severe course, with up to 500 or more pox lesions, presumably because such patients receive a larger inoculum of virus from infected siblings. By the end of the first week, infected children again are afebrile, and the cutaneous lesions continue to form crusts that dry and fall off. Infants younger than 1 year may have more severe disease; likewise, older teenagers and adults are at greater risk when they develop chickenpox. The mortality for chickenpox in otherwise healthy children (ages 1 through 14 years) is approximately 1 in 50,000, whereas that for infants younger than 1 year is 1 in 13,000. One subgroup at highest risk for fulminant chickenpox is children receiving high-dose corticosteroid therapy for such diseases as asthma.
The most frequent complication of chickenpox in a healthy child is bacterial infection of a vesicular lesion (Box 199.1). The most common infecting organism is group A Streptococcus, although staphylococcal infections also occur. Secondary diseases range from cellulitis and erysipelas to cutaneous abscesses, impetigo, and suppurative lymphadenitis. More serious, but less common, bacterial sequelae include septic arthritis and osteomyelitis, streptococcal necrotizing fasciitis, and staphylococcal pyomyositis.
The viral sequelae of chickenpox can involve virtually all organ systems and can include pneumonitis, hepatitis, arthritis, pericarditis, glomerulonephritis, orchitis, and involvement of
the nervous system. Neurologic manifestations include meningoencephalitis, myelitis, and polyneuritis. In particular, the acute cerebellar syndrome is the most common VZV-induced neurologic disease in children. Usually, ataxia begins during the second week of the illness, but it can precede the exanthem. Often, cerebellar signs and symptoms persist for several weeks but resolve with no permanent neurologic deficits. The preferred method for diagnosis of viral cerebellitis is magnetic resonance imaging, which can detect abnormal signals within the cerebellum better than can computed tomography. Eye findings include unequal pupil size (anisocoria). Chickenpox also is associated temporally with Reye syndrome.
the nervous system. Neurologic manifestations include meningoencephalitis, myelitis, and polyneuritis. In particular, the acute cerebellar syndrome is the most common VZV-induced neurologic disease in children. Usually, ataxia begins during the second week of the illness, but it can precede the exanthem. Often, cerebellar signs and symptoms persist for several weeks but resolve with no permanent neurologic deficits. The preferred method for diagnosis of viral cerebellitis is magnetic resonance imaging, which can detect abnormal signals within the cerebellum better than can computed tomography. Eye findings include unequal pupil size (anisocoria). Chickenpox also is associated temporally with Reye syndrome.
BOX 199.1. Complications of Chickenpox
Bacterial
Cellulitis
Erysipelas
Cutaneous abscess
Impetigo
Suppurative lymphadenitis
Septic arthritis
Osteomyelitis
Necrotizing fasciitis
Pyomyositis
Viral
Pneumonitis
Hepatitis
Arthritis
Cerebellar syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree