Pulmonary Valve Atresia with Intact Ventricular Septum
Donald A. Riopel
Pulmonary valve atresia with intact ventricular septum (PA:IVS) results in varying degrees of hypoplasia of the right ventricle and tricuspid valve. The clinical course of severe hypoplasia of the right ventricle can be almost as devastating as that of severe hypoplasia of the left side of the heart. Infants with moderate or mild hypoplasia, however, have a more favorable clinical course.
INCIDENCE
The defect is estimated to occur in 0.1 to 0.4 per 10,000 births. No distinct gender preference exists.
ETIOLOGY
At stage 15 of embryologic development, four mounds of endocardial cushion tissue, which eventually form the thin aortic and pulmonary valve cusps, are present in the outflow channel of the developing heart tube. Abnormalities of one valve without abnormalities of the other suggest that the cause of the condition occurs after the valve cusps are formed. The association of pulmonary artery obstruction with rubella infection is one indication that a fetal inflammation may be causative.
PATHOLOGY
The pulmonary valve obstruction is complete. The valve tissue is a membrane, usually with fused commissures depicted by raphes and with three formed cusps. The right ventricular cavity ranges in size from tiny to larger than normal, although it is smaller than normal in most cases.
Communications between the right ventricle and the coronary artery system via myocardial sinusoids frequently are seen. They are unique to this lesion and carry an unfavorable prognosis.
The tricuspid valve, by definition, is patent in all cases, and the size of the tricuspid orifice appears to be proportional to the right ventricular cavity. The deformity of the tricuspid valve results in varying degrees of severity of stenosis or insufficiency. The size of the right atrium depends on the degree of tricuspid insufficiency and on the presence and size of the communication between the atria.
PHYSIOLOGY
Fetal
With no outlet of the right ventricle, the fetus with PA:IVS directs all systemic venous blood to the left side of the heart through a communication in the atrial septum. Therefore, the blood flow through the entire left side of the heart is greater than that in the physiologically normal fetus.
Postnatal
Systemic venous blood enters the right atrium from the vena cavae. With no exit possible through the pulmonary valve, the blood must cross the atrial septum through the foramen ovale or an atrial septal defect. Systemic saturation depends on the amount of pulmonary blood flow, which, in turn, depends on the size and patency of the ductus arteriosus. As the ductus undergoes a natural tendency to close, oxygen tension decreases and symptoms of hypoxia occur.
The presence of communications between the coronary artery system and the right ventricle via right ventricular sinusoids affects coronary blood flow and causes ischemia and subendocardial fibrosis of both ventricles.
CLINICAL MANIFESTATIONS
Symptoms
Most of these infants are born at term, have not had growth retardation in utero, and are vigorous. Symptoms of cyanosis occur within a few hours to several days after birth and are dependent on ductal flow. Cyanosis may be intermittent and associated only with the stress of feedings or may be sudden and severe because of sudden closure of the ductus arteriosus. Infants with severe cyanosis also have accompanying acidosis and deep compensatory respirations in an attempt to correct the metabolic acidosis. Hypoxia, acidosis, or hypoglycemia, singly or in combination, can lead to seizure activity.
Signs
In the symptomatic infant, severe cyanosis of the mucous membranes and nail beds occurs, with paleness of the skin occurring secondary to a low cardiac output and peripheral vasoconstriction. Hyperpnea is present, and no rales are heard on auscultation of the lungs. Cardiac auscultation may reveal only the single second heart sound of aortic closure with no murmur. When tricuspid insufficiency is present, a long systolic murmur is heard along the lower left sternal border. Rarely is a continuous murmur heard. The liver may be engorged and pulsatile because of passive congestion, such as occurs with tricuspid atresia. Pulses are weak and thready. Cyanosis of the nail beds and clubbing occurs in infants older than 4 months of age.
LABORATORY FINDINGS
Arterial blood gases in severely cyanotic infants who are not receiving prostaglandins have a low pH, a very low PO2 (often
in the teens), and a somewhat low PCO2 with a negative base deficit. In infants receiving prostaglandins, arterial blood gas values may approach normal.
in the teens), and a somewhat low PCO2 with a negative base deficit. In infants receiving prostaglandins, arterial blood gas values may approach normal.
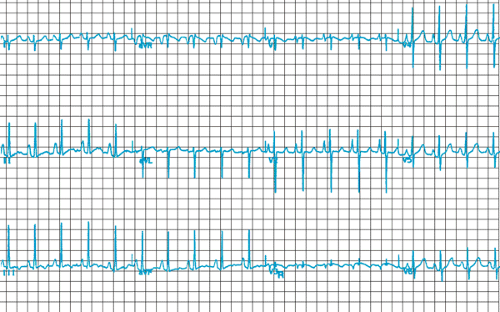
Electrocardiographic findings in PA:IVS depend on the anatomy of the defect. The rhythm is sinus with normal time intervals, and the P wave often is tall and peaked. The QRS frontal plane vector tends to be in the lower left quadrant in cases of a small right ventricle, whereas it usually is rightward (greater than 120 degrees) in cases with a normal or a large right ventricle. With a severely hypoplastic right ventricle, the R-to-S ratio in the horizontal plane favors the posterior forces, a finding suggesting absent or diminished right ventricular forces (Fig. 275.1). The T wave usually is normal, except when ischemia of ventricles is present, whereupon discordant T vectors are seen and ST changes of strain are present.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree