Syphilis
Charles R. Woods
Worldwide, syphilis, a venereal disease of adolescence and adulthood, remains important in pediatrics as an acquired and a congenital infection. Syphilis was recognized as a disease in Europe during the fifteenth century and initially was called the “great pox,” in distinction from smallpox. Treponema pallidum, the etiologic agent of syphilis, was described in 1905, but symptoms specific to syphilis were not determined until 1938 because of frequent dual infection with gonorrhea. Humans are the sole natural host of T. pallidum.
MICROBIOLOGY
T. pallidum is a member of the genus Treponema (order Spirochaetales), which contains three other pathogens [T. pertenue (yaws), T. carateum (pinta), and T. endemicum (endemic syphilis, or bejel)], and at least six nonpathogens that can be normal flora in the oral cavity and in the genitourinary and intestinal tracts. Treponemes are microaerophilic gram-negative bacteria that are 6 to 20 μm long and 0.1 to 0.5 μm in diameter. Morphologically, they are rod-shaped, with 8 to 14 flat waves that give a helical appearance. They possess six axial fibrils that are intracellular, flagellumlike organelles that extend pole to pole, vary in length, and determine the shape and characteristic motility of the microbe. Treponema reproduce by transverse fission.
Survival outside an infected host is very limited. Difficulties in cultivating T. pallidum have hampered efforts to understand the pathogenesis of disease caused by these organisms. Virulent strains have been propagated by intratesticular inoculation in rabbits, and limited in vitro culture on monolayers of several cell types has been achieved, but in vitro culture for diagnostic purposes remains unavailable.
EPIDEMIOLOGY
Syphilis occurs most often in adolescents or in adults via sexual contact. The risk of acquiring infection per sexual contact with an infected partner is approximately 30%. The microbe can invade intact mucous membranes or areas of abraded skin. Acquisition by direct contact with an infected lesion rarely occurs, but health care providers can become infected by contact if appropriate barrier precautions are not used. Congenital syphilis occurs through the transplacental passage of T. pallidum from an infected mother to a fetus or by contact with an infectious lesion in the birth canal. Transplacental transmission can occur throughout pregnancy. The risk of vertical transmission is greater among pregnant women with primary or secondary syphilis than with latent disease, and this risk diminishes after the fourth year of untreated infection. In children with acquired syphilis manifesting in childhood, sexual transmission should
be assumed unless another mechanism is identified. Syphilis seldom is found in children who have been sexually abused.
be assumed unless another mechanism is identified. Syphilis seldom is found in children who have been sexually abused.
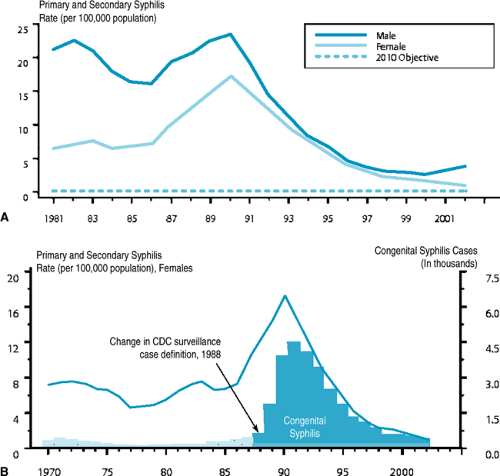
An upsurge in the number of syphilis cases in the United States during the late 1980s subsequently diminished during the 1990s (Fig. 178.1A). Risk factors associated with this increase, and with many current cases, include poverty, crack cocaine use, trading sex for drugs and money, and infection with human immunodeficiency virus (HIV). Dual infection with gonorrhea is present in 8% of cases. Syphilis is more prevalent in men than in women, and the gender gap in primary and secondary syphilis cases that had been closing in the United States during the 1990s began to widen again in 2001 (Fig. 178.1A). In 2002, the national rate among men was 3.8 cases/100,000 compared with 1.1 among women. The increase in male cases occurred primarily among men who have sex with men.
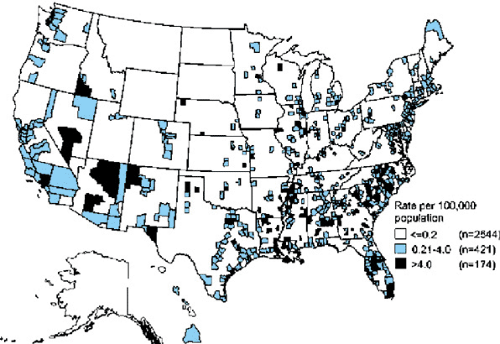
African Americans have had rates higher than those of other groups in the United States, but this disparity narrowed from more than 50-fold compared with non-Hispanic whites in 1991 to eightfold in 2002. The peak age range of syphilis is 15 to 55 years, coinciding with increased sexual activity. Female case rates are higher than those of males from ages 15 to 19 years, reflecting sexual activity with older males who have higher infection rates. The rates of syphilis vary widely across the United States (Fig. 178.2). In 2002, the South continued to have higher rates (3.1 per 100,000) than those of the West (2.3 per 100,000), Midwest (2.1 per 100,000), and Northeast (1.7 per 100,000), although rates increased in the latter three regions in 2002.
The rates of congenital syphilis in the United States have declined since 1991 and correspond closely with those of acquired syphilis in women of childbearing age (Fig. 178.1B). Inadequacy or lack of prenatal care is a risk factor for vertical transmission to the fetus or newborn (the mother goes untreated). Syphilis remains a considerable public health issue in developing countries and Eastern Europe. Congenital syphilis increased 26-fold in the Russian Federation from 1991 to 1999.
PATHOGENESIS
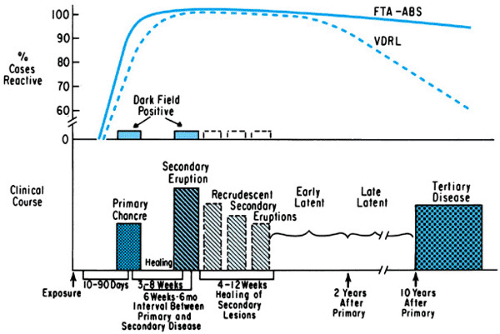
Four stages of syphilitic disease are defined: primary, secondary, latent, and tertiary (Fig. 178.3). Syphilis begins when T. pallidum penetrates the skin or mucous membrane at a site of
exposure. An outer membrane protein of the microbe appears to attach to a receptor(s) on the host cell surface, initiating invasion. The organism multiplies locally and spreads through the perivascular lymphatic system to the systemic circulation, which disseminates the infection widely even before a primary lesion is evident. Capillary cells are a prime target of parasitism. During the typical 3-week incubation period, a local, intense inflammatory response by plasma cells, macrophages, and lymphocytes ensues, with obliterative endarteritis in the area of inflammation. This response produces the red, indurated, ulcerative, spirochete-filled lesion of primary syphilis: the chancre. A concomitant cellular proliferation in the regional lymph nodes produces adenopathy.
exposure. An outer membrane protein of the microbe appears to attach to a receptor(s) on the host cell surface, initiating invasion. The organism multiplies locally and spreads through the perivascular lymphatic system to the systemic circulation, which disseminates the infection widely even before a primary lesion is evident. Capillary cells are a prime target of parasitism. During the typical 3-week incubation period, a local, intense inflammatory response by plasma cells, macrophages, and lymphocytes ensues, with obliterative endarteritis in the area of inflammation. This response produces the red, indurated, ulcerative, spirochete-filled lesion of primary syphilis: the chancre. A concomitant cellular proliferation in the regional lymph nodes produces adenopathy.
The secondary lesions of syphilis, a consequence of dissemination, are caused by an inflammatory response in ectodermal tissue of skin, mucous membranes, and the central nervous system (CNS). The host response to these lesions is similar to that which occurs to primary lesions. The condylomata lata (venereal warts) of secondary syphilis are characterized by epithelial hyperplasia, hyperkeratosis, plasma cell infiltrate, and presence of spirochetes.
Tertiary syphilis can involve any organ and is caused by slowly developing immune-mediated host responses to the infection. This stage is characterized by a diffuse, chronic inflammation in affected tissues, generally skin, CNS, and cardiovascular tissues. Gummata are late-appearing focal areas of nonsuppurative inflammatory necrosis surrounded by fibrotic scarring. Viable organisms are rare findings or absent in these lesions, which appear to result from a granulomatous hypersensitivity reaction.
Congenital syphilis from the transplacental passage of treponemes during maternal spirochetemia can occur as early as 9 to 10 weeks of gestation. Pathologic changes have been observed as early as 15 weeks. Transmission in utero causes the wide dissemination of the organism in the fetus. The organs affected most severely include brain, liver, lung, and the skeletal system. Early infection can lead to spontaneous abortion of syphilitic fetuses, generally after 18 weeks of gestation. Infected fetuses and newborns may have extramedullary hematopoiesis. The placenta typically is large and thickened, having hypercellular villi with acute and chronic inflammation, as well as proliferative fetal vascular changes. The umbilical cord often contains abscesslike necrotic foci around the vessels within the Wharton jelly. Spirochetes are present in the umbilical vessel walls.
IgM and IgG antibodies are detectable by the time the chancre appears, but humoral immunity is insufficient to control the infection. Cell-mediated immunity is suppressed during the primary and secondary stages of infection. After effective treatment, IgM antibody declines over the course of 1 to 2 years, but IgG antibodies usually persist throughout the life of the infected person. The host immune response is not protective, such that reinfection after treatment commonly occurs.
CLINICAL MANIFESTATIONS AND COMPLICATIONS
Most cases of syphilis encountered in pediatric practice are seen in infants (congenital) or in sexually active adolescents. The stages of acquired syphilis are based on the different clinical manifestations and underlying pathophysiology. The hallmark of primary syphilis is the chancre, a skin lesion that appears at an inoculation site after a mean incubation period of 21 days (range, 3 to 90 days). The chancre, usually single and nontender, occurs most often on the genitalia and is associated with nontender lymphadenopathy. Regional lymphadenopathy may be the only readily apparent sign of primary syphilis in women when chancres occur on the cervix or vaginal wall. Primary syphilis heals spontaneously in 3 to 12 weeks.
Symptoms of secondary syphilis appear 2 to 12 weeks after the onset of primary syphilis and result from the dissemination of treponemes. Symptoms include low-grade fever, sore throat, headache, malaise, and diffuse lymphadenopathy. The most notable manifestation is a rash that consists of macular, maculopapular, papular, or pustular lesions that inevitably harbor organisms. The classic rash begins on the trunk and, at this stage, is generalized and maculopapular, eventually involving most of the body, including the palms and soles. Secondary syphilis may cause condylomata lata, which are hypertrophic papular skin lesions found in such moist areas as the anus or vulva. All skin and mucous membrane lesions of secondary syphilis are highly contagious. Neurosyphilis occurs in approximately 30% of patients during the course of secondary syphilis. Pleocytosis and proteinosis are present in the cerebral spinal fluid (CSF) and may be clinically silent or become manifest as meningeal and cranial or spinal nerve involvement that are reversible with proper therapy. Immune complexes comprised of treponemal antigen, fibronectin, antibody, and complement are implicated in the pathogenesis of iritis, anterior uveitis, arthritis, and nephrotic syndrome that can occur during secondary syphilis.
The rash and other findings of secondary syphilis resolve in 1 to 2 months, giving way to a latent period, defined by positive syphilis serology with no evidence of disease. Recurrences of secondary manifestations can occur during the first year (early latency) but not thereafter (late latency). Approximately 60% of untreated patients will have persisting latency. Patients are relatively immune to reinfection during latency.
Tertiary, or late, infection occurs in approximately 40% of untreated patients after a latent period of at least 1 year or, more frequently, 3 to 10 years. Gummata, the classic lesions of tertiary syphilis, develop in skin, soft tissue, and bone in 15% of cases. These lesions have minimal clinical impact, and their presence has been called benign late syphilis. Cardiovascular syphilis, including syphilitic aortitis with medial necrosis, occurs in 10% of patients with late syphilis, with onset occurring usually 10 to 40 years after primary disease. Neurosyphilis persists in approximately one-half of untreated patients and may remain asymptomatic or mimic almost any other neurologic disease. Common presentations include tabes dorsalis (degeneration of dorsal columns of the spinal cord), paresis, dementia, meningitis, and amyotrophic lateral sclerosis (ALS). The interval between primary syphilis and the onset of late neurosyphilis usually is more than 5 years, but disease may progress more rapidly in children than in adults.
Congenital Syphilis
Untreated syphilis that occurs during pregnancy is transmitted to the fetus in nearly all cases and can lead to spontaneous abortion (usually after the first trimester), stillbirth, premature delivery, and nonimmune hydrops fetalis. Live-born infected infants may be asymptomatic (as many as two-thirds) or manifest early signs (those appearing in the first 2 years of life) and/or late signs (those appearing later, over the first two decades of life). Any organ system can be affected because of the widespread dissemination that occurs after transplacental infection. In the newborn, congenital syphilis can have presentations similar to those of congenital infections caused by cytomegalovirus, toxoplasmosis, herpes simplex virus, rubella, bacterial sepsis, blood group incompatibility, and numerous other neonatal conditions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree