Today, injured service members are surviving wounds that would have been fatal in previous wars. A recent RAND report estimates that approximately 320,000 service members may have experienced a traumatic brain injury (TBI) during deployment, and it is not uncommon for a soldier to sustain multiple associated injuries such as limb loss, paralysis, sensory loss, and psychological damage. As a result, many military service members and their families face significant challenges returning to a high quality of independent life. The architectural concepts of universal design (UD) and evidence-based design (EBD) are gaining interest as an integral part of the rehabilitation process of veterans with TBI. This article examines the possibilities presented by UD and EBD in accordance with the Americans with Disabilities Act of 1990, in terms of high-end building and interior design quality, and possible technological options for individuals with disabilities.
The US Census Bureau reports that more than 41.2 million individuals older than 5 years live with some type of disability. Of this population, more than 11 million persons older than 6 years require personal assistance with every day activities. Each year, approximately 1.5 million Americans sustain a traumatic brain injury (TBI), with direct medical costs and indirect costs (such as lost productivity) totaling to an estimated $60 billion in the United States in 2000. More than 5 million Americans are estimated to be living with long-standing disability from TBI, including cognitive, physical, behavioral, and emotional difficulties. For veterans with service-connected disabilities in the fiscal year 2007, more than $28.2 billion was spent in compensation. This number can only be expected to increase as military operations continue in support of the Global War on Terrorism.
Since military operations began in Iraq and Afghanistan, more than 1.6 million US service members have been deployed. Improvements in protective body armor, medical evacuation techniques, and forward area surgical resuscitation have dramatically improved battlefield survival rates. Today, injured service members are surviving wounds that would have been fatal in the previous wars. A recent RAND Corporation report estimates that approximately 320,000 service members may have experienced a TBI during deployment. Because of the mechanism of the injury, which is most commonly from a blast, it is not uncommon for a soldier to sustain multiple associated injuries in addition to the TBI, including limb loss, paralysis, sensory loss, and psychological damage. As a result, many military service members and their families face significant challenges returning to a high quality of independent life.
Military reports suggest that more than 850 service members have sustained a major limb loss as a result of military service since 2001, with more than 20% of them losing more than one limb and greater than 50% also sustaining a TBI. Many of these individuals have also sustained vision loss in one or both eyes, hearing deficits, pain syndromes, and difficulty with balance and orientation. Related cognitive difficulties, such as poor memory, decreased concentration, impaired executive functioning, and emotional labiality, which are manifested by irritability, anger, and depressed mood, make it difficult for many individuals to live alone or even with others. Further complicating the problem is the young age of many of the individuals who are challenged to live with their acquired disabilities for the rest of their lives.
Current paradigms in medical rehabilitation primarily focus on teaching individuals the strategies to adapt and reintegrate into existing environments. Architecture, however, focuses more on how to adapt the environment to the individual. Architects are skilled at integrating new materials, construction methods, and design to customize an environment for an individual client. By listening to a client’s needs, the architect attempts to optimize a living and work environment to improve productivity and efficiency, and also influence the mood of those who enter the space. By manipulating interior and exterior spaces through the use of volumes, light, and materials, it is the hope of architects to improve the quality of life for those who encounter their design. Just as there is a symbiosis between nature and animal life, one also exists between humans and the built environment around them. It seems only fitting, therefore, that architects work with medical and rehabilitation professionals to embrace the current challenges faced by many severely injured service members to create new environments for those with significant disabilities.
Since the signing of the Americans with Disabilities Act (ADA) of 1990, building codes have provided minimum standards to help reduce the architectural barriers experienced by individuals with disabilities. Unfortunately, architecture and its role in improving the lives of individuals with disabilities have been relatively stagnant over the past 2 decades. Although advocates for “universal design” (UD) and organizations such as the Paralyzed Veterans of America (PVA) continue to promote “barrier-free environments,” the field remains lacking in high-end design quality and options for individuals with disabilities.
The concept of UD was developed in the 1990s for the purpose of creating new products that are usable by all consumers, including those with disabilities and the elderly. UD involves the creation of new environments, devices, materials, and tools that provide accessibility, adaptability, ease of use, and safety to all users. The concept emphasizes the importance of designing buildings, appliances, and tools that are easy to use for all individuals of all ages and abilities.
Since the introduction of UD, research universities and organizations involved with disabled veterans have made efforts to spread the concept of UD to product designers and marketing firms. North Carolina State University was involved in this process, and subsequently developed 7 principles of UD. The principles include (1) equitable use, (2) flexibility in use, (3) simple and intuitive use (ie, single color pictograms), (4) perceptible information (ie, cell phones with speed dial), (5) tolerance for error (ie, temperature limiter on a shower to prevent burning), (6) low physical effort, and (7) size and space for approach and use (ie, sliding doors than hinging doors). The implementation of UD in hospitals, in and around the city, and at home can have many benefits for people with disabilities. When universally designed products are integrated into everyday living, individuals with disabilities can have more control over their environment, ultimately leading to more independence and a better quality of life.
“Evidence-based design” (EBD) has gained interest by architects, builders, and clients. EBD involves applying the use of sound research to make decisions on a project to achieve the best outcome. EBD is frequently used by architects and others involved in the design and construction of commercial buildings. An evidence-based designer works with an informed client, or group of clients, to determine the best solution that will meet the needs of the clients. By implementing EBD, needs of the clients can be met through a collaborative effort between architects, interior designers, facility managers, and anyone else closely involved with the project.
The Center for Health Design, created in 1993, is an advocacy and research organization that seeks to promote the implementation of EBD within the health care system. The mission of the Center is to “transform healthcare environments for a healthier, safer world through design research, education, and advocacy.” The organization seeks to promote forward thinking within the health care discipline, and it supports the implementation of personalized architecture or design. The Center for Health Design is involved in several research projects throughout the United States that are associated with the implementation of EBD. The Pebble Project is one initiative that has received growing attention throughout the past several years.
Founded in 2000, the Pebble Project is a nationwide research effort designed to provide evidence to health care professionals regarding the importance of a health care facility’s design. The goal of the initiative was to establish that the design and layout of a room or building has a significant impact on patient and staff outcomes. The Pebble Project has research initiatives throughout the United States, and preliminary data have been gathered from several research sites. The PeaceHealth Organization in Eugene, Oregon, for example, installed ceiling lifts and booms in the intensive care unit and neurology department to see what the effect would be on patient handling injuries. The results were encouraging; patient handling injuries decreased by 99%. Another medical center in Boise, Idaho, Saint Alphonsus Regional Medical Center, discovered that after renovations were made to a nursing unit (including larger rooms within the ward, carpet in the hallways, and acoustic tiles on walls and ceilings), noise levels had dropped significantly and quality of sleep improved from 4.9 to 7.3 (on a 10-point scale). Hospitals and clinics throughout the nation that are involved with the Pebble Project have experienced similar positive changes associated with patient outcomes, and staff morale has increased in hospitals where EBD has been implemented.
Health care organizations have begun to take notice of EBD principles. Schweitzer and colleagues conducted a review of optimal healing environments within the health care setting, emphasizing the need for designing healing spaces that contribute to making improvements in patient satisfaction and well-being. Schweitzer’s group discussed a variety of stimuli that have an effect on patient recovery and overall well-being. Examples include personal space, sensory environment (including smells and sound or noise), environmental complexity, fresh air and ventilation, light, color, viewing and experiencing nature, art esthetics and entertainment, and positive distractions (including humor entertainment). The complexity of the environment was reported to positively influence elderly cognitive function.
EBD supports the principle of using design to promote patient comfort and reduce any detrimental effects on the patients’ physical or psychological well-being. The use of EBD becomes particularly challenging, however, when given the unique considerations for each patient. Many health care settings treat patients of multiple different injuries and illnesses with varied social and cultural backgrounds. Regardless of the widespread patient diversity, EBD advocates that a patient’s physical, mental, emotional, and spiritual healing must be considered in the design of a health care facility.
The literature highlights several approaches that hospitals and clinics may take for better incorporation of patient needs. To begin with, research conducted on geriatric patients suggested that the arrangement of furniture within hospital lounges and even individual rooms has an effect on social interactions and communication. As a result, proper placement of furniture can lead to increased social interactions and increased communication between patients, family members, and staff. In addition to furniture arrangements, location and number of nursing stations can also affect patient and staff relationships. Increasing the number of nursing stations within a ward may be valuable for patients, because this may allow for increased confidentiality and more privacy between patients and staff. Likewise, increased visiting hours for family and friends can have a positive effect on patient well-being, because contact with caring individuals during the recovery process has been shown to reduce stress and is a positive contributor to health. Furthermore, widening doors to patient bathrooms may reduce patient falls, and single-bed hospital rooms have been reported to lead to fewer medication errors and improved comfort for the family and friends of the patient. Patients with depression may experience a reduction or relief from symptoms when their environment encourages physical activity. Finally, various images and symbols located within the hospital bedroom or hallways may influence the behavior of patients.
Improved environments within health care organizations may also positively influence the medical staff. For example, relationships among hospital staff members may be improved by designing an environment that encourages positive interactions among staff members, such as gardens and staff-only lounges. In addition, redesigning nursing stations to allow for more opportunities for patient and staff interactions may improve staff satisfaction and patient outcomes. It is well known that stress, anxiety, depression, and loss of control are detrimental to health. The opposite is also true: optimism, self-efficacy, and a sense of control are associated with positive outcomes and good health. Proponents of EBD believe that this can and should be influenced by architecture.
In addition to the initiatives taking place in advanced design, rehabilitation engineers and scientists continue to apply emerging technologies and materials to advance assistive technology (AT) to improve the lives of individuals with disabilities. AT devices, such as ultralight wheelchairs, robotic systems, and microprocessor prostheses, allow individuals with impaired mobility to be much more independent than they were even a decade ago. Current adaptive equipment will allow a person with tetraplegia, limb loss, or visual impairment to ski down a mountain, sail across a lake, or return to activities such as hunting, fishing, or even scuba diving. Cognitive aids, including a personal digital assistant (PDA), are frequently used to help individuals with memory problems to remember names, phone numbers, appointments, or medication regimens. Improved personal computers and new software applications are able to turn text into Braille, operate various entertainment systems from a single platform, interpret voice commands, and automatically activate emergency support systems as needed in cases of home fires or burglary. Despite these fascinating advances, there has been little effort in how to best incorporate these AT devices into modern architecture and design practice.
The concept of “smart homes” has also emerged as a way to bridge advanced technology, especially AT, into the home environment of individuals with disabilities. Over the past few years, the media have started reporting on the concept of a “smart home.” According to a CNN report by Julie Clothier, eNeo Labs, a company in Barcelona, Spain, has created an environment-friendly “smart home.” Clothier reported that eNeo Labs has designed and developed a home that is controlled by the click of a button: all household appliances are connected and controlled by a single remote control; settings can be personalized for different family members; and the house can accept, respond to, and send text messages to its owner, notifying him, for example, that there is a water leak. Although seemingly unreal, this concept is being tested on a family of 4 living outside Barcelona. The CNN report and another report featured in LiveScience highlighted the unique abilities of the house, stating that it would be “security-conscious and aware of its inhabitants at all times,” noting when a person enters and exits a room, and eventually being able to respond to voice commands.
The General Manager of eNeoLabs, Javier Zamora, stated that there are 2 main components to a smart home: the “information network” and the “brain.” The “information network” serves to connect all of the household appliances within the home, and the “brain” coordinates the activities of the appliances and connects them to the outside world. Although “smart home” technology is in its infancy in the United States, it seems promising that the technology will be obtainable in the coming years.
Of particular interest of many civilian, military, and veterans groups is what can be done to help service members with TBI and associated comorbidities reintegrate successfully into society. The authors believe that the importance of one’s environment during recovery and rehabilitation, whether in a hospital setting or at home, is underemphasized and that through collaborative efforts between architects, designers, engineers, and clinicians, better solutions can be achieved to improve the quality of life for many severely injured service members.
The authors’ team recently explored the role that architecture could play in helping injured service members with TBI. Through a collaborative effort between the Catholic University of America; University of Pittsburgh, the US Department of Veterans Affairs, the Rehabilitation Research and Development Service, and the Walter Reed Army Medical Center (WRAMC), a team of architects and students met clinical experts and also individuals with TBI and their family members to better understand their needs. Focus groups conducted structured and nonstructured interviews with medical staff, patients, and families. In addition, as part of his architectural master’s thesis, Jeffrey Giuggio immersed himself at WRAMC, where he directly observed patients and families, and also interviewed members of the TBI clinical teams to best understand their unique needs.
It was clear that existing environments, whether in hospitals, commercial buildings, or private residences were not optimal for individuals who had difficulty with orientation, irritability, light sensitivity, or emotional labiality, even though all these environments met ADA standards. More troubling, however, was the patient’s and family’s report of the difficulty in returning home. Fundamental in the rehabilitation and recovery of individuals with severe injury is their return home and reintegration in society. In fact the World Health Organization places great emphasis on “participation” as a meaningful measure of outcomes from a disability. “Participation” may involve activities such as work, education, parenting, or volunteerism, but at its core seeks to improve the lives of individuals with disabilities by having them be active participants in the world and in the lives of people around them. Many individuals with TBI continue to have significant difficulty in living independently. Some injured service members, who were once high-functioning soldiers responsible for operating million-dollar equipment and who were models of self-reliance and independence, due to their acquired disability are now forced to move back in with their parents, relying on them for basic functions such as feeding, bathing, and toileting. This loss of independence only exacerbates their state of mind and may often cause the development of serious negative mental health.
Hearing these concerns, the authors’ team sought to concentrate its efforts by trying to improve the home environment for this challenging patient population. The authors offer the following thesis, which was developed by Mr Giuggio and his advisors, as an example of how architecture, design, and technology may be applied to help mitigate the effect of disabilities on a military population with TBI, at the same time hoping that it will be only the first step in further studies for bringing professionals together from various disciplines to improve the lives of all persons with disabilities.
The thesis was to design a contemporary living environment for service members with TBI and its associated disabilities. While emphasis was placed on incorporating the latest technology in AT, equal importance was also given to the functionality of the environment and to the esthetics. To avoid the “sterile” atmosphere created in most medical facilities, this project sought to create a unique, clean, and modern space, commiserate with a young population of individuals with disabilities, with the belief that this would also be more conducive to healing. Because of the complexities of associated injuries and resultant disabilities, it was decided that such an intervention would need to be modular, so that it could be customized for each individual and family.
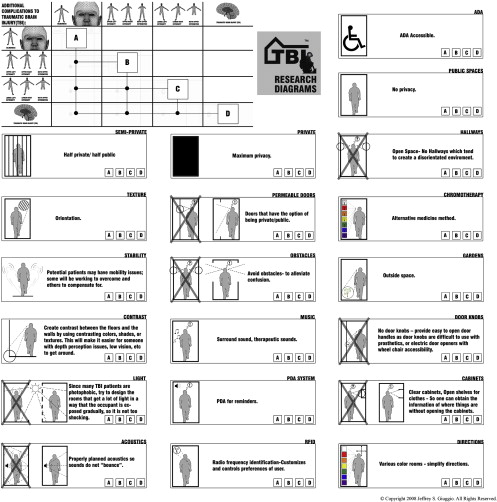
During the early stages of development, it was clear that a new “vocabulary” of design features needed to be formulated to meet the unique needs of this patient population. To this end, a legend of design graphics was created that could be translated into architectural drawings to denote specific needs ( Fig. 1 ). Patients with TBI may have multiple cognitive impairments, accompanied by loss of vision or the use of one or more limbs. A suitable environment, therefore, must address issues such as privacy, pathfinding, acoustics, orientation, mobility, access, comfort, and mood control. In architectural terms, these must be displayed in graphic form to facilitate the design process. The conceptual diagrams in Fig. 1 were derived to designate UD features that would accommodate a multitude of impairments in association with TBI. The conceptual diagrams serve as guidelines in the design to accommodate both patient and caregiver needs.