Ulnar Shortening Osteotomy
Lance G. Warhold
Nelson L. Jenkins
DEFINITION
Ulnar impaction syndrome (ulnocarpal abutment) results from a chronic compressive overloading of the ulnocarpal articulation secondary to static or dynamic ulnar positive variance.
Ulnar variance defines the relationship of the length of the ulna to that of the radius.
Ulnar positive variance can be the result of a congenital anomaly; traumatic radial shortening from a distal radius, Essex-Lopresti, or Galeazzi fracture; injury to the distal radius physis; or a variant of normal anatomy.
An ulnar shortening osteotomy is designed to decompress the ulnocarpal joint while simultaneously tightening the ulnocarpal and radioulnar marginal ligaments of the triangular fibrocartilage complex (TFCC).16
Ulnar shortening osteotomy has been shown to be an effective alternative to TFCC repair in in the management of Palmer type IB tears.20
Ulnar shortening osteotomy has been shown to be effective in reducing symptoms of isolated posttraumatic lunotriquetral ligament tears regardless of preoperative ulnar variance.13
ANATOMY
The distal radius has three articular surfaces: the scaphoid fossa, the lunate fossa, and the sigmoid notch.
The radius articulates with and rotates around the ulnar head via the sigmoid notch. The sigmoid notch has welldefined dorsal, palmar, and distal margins, whereas the proximal margin is indistinct.
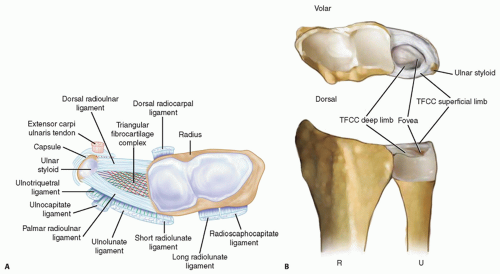
The distal radioulnar joint (DRUJ) and ulnocarpal relationships are maintained by numerous ligamentous structures (FIG 1A).
The interosseous membrane is a complex structure with a thickened central portion. It almost completely spans the radius and ulna, acting as a hinge for forearm rotation.
The diaphysis of the distal half of the ulna is supplied by small segmental branches from the anterior and posterior interosseous arteries. These enter the ulna in 1- to 3-cm intervals from the direction of the interosseous membrane and must be protected during the surgical approach.26
The dorsal capsule of the DRUJ contains two ligaments: the proximal metaphyseal arcuate ligament and the distal radioulnar ligament. The palmar capsule is composed of a single radioulnar ligament.1
The TFCC spans the ulnocarpal joint and connects the distal radius to the distal ulna (FIG 1B). The TFCC functions to cover the distal ulna, to partially dampen and transmit a portion of the axial load of the wrist through the ulna, to stabilize the DRUJ, and to provide support for the ulnar side of the carpus.
The TFCC contains a central avascular articular disc composed of types I and II collagen. It is of variable thickness (average, 2 mm) and chiefly functions in load transmission between the ulnar head and ulnar carpus.
The articular disc is connected to the peripheral palmar and dorsal radioulnar (marginal) ligaments, which originate on the medial border of the distal radius and insert into the base of the ulnar styloid at the fovea. These ligaments are composed of linear type I collagen and are stabilizers of the DRUJ.
The ulnolunate and ulnotriquetral ligaments originate from the ulnar fovea and pass palmar to the palmar radioulnar ligament. They traverse the palmar surface of the TFCC to insert on their respective carpal bones. These ulnocarpal ligaments stabilize the ulnar side of the carpus relative to the ulna and resist carpal supination.
The periphery of the TFCC is supplied by dorsal and palmar branches of the anterior interosseous artery and the ulnar artery. Because of this vascular distribution, injuries to the periphery of the TFCC are capable of healing and are often amenable to repair. Injuries to the central avascular portion of the articular disc do not heal in a predictable manner and are often treated with débridement.
PATHOGENESIS
Normal ulnar variance ranges from neutral to plus or minus 2 mm. The average axial load transmitted across the TFCC and subsequently the ulna is 20% if ulnar variance is neutral. An ulnar positive variance of 2.5 mm increases the load across the distal ulna to 42.7%, whereas an ulnar variance of −2.5 mm decreases the ulnar load to 3.1% (Table 1).19
Congenital or acquired ulnar positive variance (FIG 2) can lead to degenerative wear of the TFCC and surrounding structures.
The Palmer classification divides TFCC lesions into traumatic (type I) or degenerative (type II).18 Type II lesions are associated with ulnocarpal impaction and are further subdivided based on the severity and the other structures involved. Type II TFCC tears are generally not amenable to direct repair.
Type IIA: TFCC wear
Type IIB: TFCC wear plus lunate or ulnar head chondromalacia
Type IIC: TFCC perforation plus lunate or ulnar head chondromalacia
Type IID: TFCC perforation plus lunate or ulnar head chondromalacia plus lunotriquetral ligament perforation
Type IIE: TFCC perforation plus lunate or ulnar head chondromalacia plus lunotriquetral ligament perforation plus ulnocarpal arthritis
Table 1 Percentage of Force Transmitted through the Ulna (Nine Arms) | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||
NATURAL HISTORY
Defining the natural history of ulnocarpal impaction syndrome is at best challenging.
The Palmer classification provides an accurate anatomic description of the degenerative changes seen in the ulnocarpal structures, but it does not dictate treatment, suggest prognosis, or indicate timing of progression.
Deterioration of the ulnocarpal structures is very common regardless of ulnar variance. Numerous cadaveric studies have found TFCC perforations and chondromalacia of the ulnar head, lunate, and triquetrum in up to 70% of “normal specimens.”12,19
Ulnar positive variance and persistent heavy demand across the ulnocarpal joint can hasten the development of the disease.
An individual’s ability to unload the ulnar side of the wrist with conservative measures and change of lifestyle may slow or even prevent progression.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient history must be detailed and must include the following:
Medical history
Description of previous surgical procedures involving not only the wrist but also the elbow
Analysis of whether the pain was caused by an acute injury or brought on by repetitive motion activities
A distal radius or radial head fracture can lead to ulnocarpal impaction, as can a chronic distal radius physeal injury (ie, the gymnast’s wrist).
Characterization of the pain
Description of the location, duration, and radiation of the pain as well as any associated swelling, burning or tingling sensations, or sounds (clicks, etc.)
Aggravating and alleviating factors
The physical examination should always begin with inspection.
The wrist and elbow should be examined for surgical scars.
Prominence of the ulna either palmarly or dorsally may indicate instability of the DRUJ. A palmar sag and a supination posture of the wrist may indicate the capsuloligamentous instability that occurs in rheumatoid arthritis.
Swelling, bruising, perforations of the skin, or obvious dislocations may indicate trauma.
Intrinsic atrophy and clawing may indicate ulnar nerve pathology.
Splinter hemorrhages beneath the nails and decreased turgor in the volar digital pads suggest vascular insufficiency.
Single-finger palpation should proceed in a systematic fashion by isolating anatomic structures. The examination should be performed with the patient’s elbow resting on a table, the hand pointing toward the ceiling, and the forearm in a neutral position.
Tenderness over any anatomic structure suggests a specific clinical diagnosis.
Active and passive range-of-motion (ROM) maneuvers may illicit pain, suggesting pathology. Limitations of ROM may be the result of swelling or obstruction (blocking). The examiner should listen for sounds of pathology throughout ROM.
Specific provocative tests should be performed in an attempt to further define the injured structure(s).
Piano key test: A positive result is characterized by painful laxity in the affected wrist compared with the contralateral wrist, suggesting DRUJ synovitis.
Ulnar compression test: A positive test is exacerbation of pain, which suggests arthritis or instability; dorsal or palmar subluxation may be noted.
Lunotriquetral ballottement test: Used to elicit laxity associated with pain and crepitus in the presence of lunotriquetral instability
Reagan shuck test: Positive if pain and clicking at the lunotriquetral joint is present, suggesting lunotriquetral ligament perforation or disruption
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographic views should include neutral rotation posteroanterior and lateral projections of both wrists. These are obtained with the patient seated and the elbow flexed at 90 degrees and the shoulder abducted at 90 degrees.
The contralateral wrist films may be used as a template for reconstruction.
Radiographic assessment of ulnar variance has used a neutral rotation radiographic view of the wrist that provides an image of the radioulnar length with the wrist unloaded. Such views may underestimate variance in wrists in which power grip and pronation result in significant proximal migration of the radius. Tomaino25 found that ulnar variance increased an average of 2.5 mm using the pronated grip view and ranged from an increase of 1 to 4 mm (FIG 3A).
Other plain views may be obtained based on clinical suspicion.
The carpal tunnel (FIG 3B) view visualizes the hook of the hamate and the pisotriquetral joint.
An oblique view in 30 degrees of pronation (FIG 3C) allows evaluation of the dorsoulnar wrist.
The reverse oblique view (30 degrees of supination) (FIG 3D) allows evaluation of the palmar ulnar wrist with a profile of the pisotriquetral joint.
An ulnar deviation posteroanterior view (FIG 3E) may reveal lunotriquetral instability or evidence of ulnocarpal abutment. If ulnocarpal abutment is suspected, it is often useful to obtain a posteroanterior radiograph with the forearm in pronation and the fist clenched (see FIG 3A), which increases ulnar variance.
Videofluoroscopy is useful for evaluating dynamic ligament instabilities. The wrist should be examined through an entire active and passive ROM as well as with provocative maneuvers in an attempt to demonstrate pathology while reproducing symptoms.
Arthrography may demonstrate a TFCC defect or interosseous ligament disruption if contrast material injected into one compartment leaks into an adjacent space.
Magnetic resonance imaging (MRI) can aid in the detection of soft tissue and osseous lesions, including interosseous and extrinsic ligament tears, TFCC defects, tumors, avascular necrosis, and occult fractures (FIG 3F).
Sensitivity of the MRI increases if it is combined with arthrography. The ability to show marrow changes in the ulnar portion of the lunate and simultaneous central TFCC pathology is very helpful in confirming a diagnosis of ulnocarpal impaction.
Arthroscopy can confirm a diagnosis suggested by findings from other diagnostic modalities.
This is the most sensitive tool for diagnosis of chondral and ligamentous pathology.
It has therapeutic applications in the management of ulnar abutment, TFCC defects, interosseous ligament tears, chondral defects, loose bodies, synovitis, and degenerative arthritis.
Bone scan, ultrasonography, and computed tomography serve a very limited role in the diagnosis of ulnar impaction syndrome.
DIFFERENTIAL DIAGNOSIS
Extensor carpi ulnaris (ECU) subluxation or tenosynovitis
DRUJ arthritis (degenerative or inflammatory), incongruity, intra-articular pathology, instability
Ulnar styloid fracture nonunion
Isolated TFCC tears
Lunate and triquetrum lesions: chondromalacia, cyst, interosseous ganglion (lunate/capitate), or intraosseous pathology (enchondroma, osteoid osteoma)
Kienböck disease
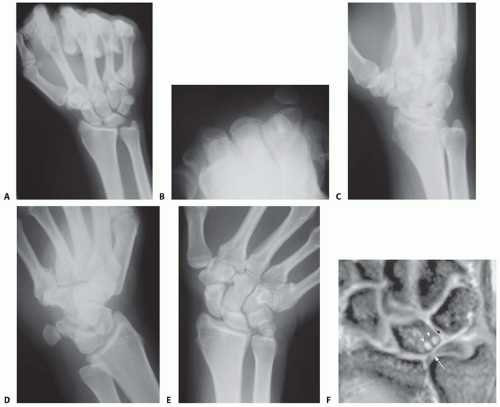
FIG 3 • A. Clenched fist view. B. Carpal tunnel view. C. Oblique view in 30 degrees of pronation. D. Oblique view in 30 degrees of supination. E. Ulnar deviation view. F. Coronal gradient-echo magnetic resonance (MR) image reveals a central triangular fibrocartilage perforation (white arrow), subchondral cystic changes in the lunate bone (arrowheads), and a lunotriquetral ligament tear (black arrow) in a 41-year-old man with ulnar impaction syndrome with positive variance and chronic ulnar-sided wrist pain (Palmer class IID lesion).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access