Ulnar Head Implant Arthroplasty
Sam Fuller
Randy R. Bindra
DEFINITION
As with any synovial joint, the distal radioulnar joint (DRUJ) can degenerate due to osteoarthritis, inflammatory arthritis, chronic instability, infection, and trauma.4
Standard treatments such as partial (“matched resection”) or complete (Darrach procedure) distal ulnar resection have the potential to destabilize the forearm axis and cause painful forearm rotation.
The normal compressive muscle forces acting between the radius and ulna help stabilize the DRUJ.1
When the distal ulna has been resected and the forearm is rotated under such a compressive load, a palpable grinding between the ulnar stump and the radius may develop; this is referred to as ulnar impingement.6 This may progress from minor irritation to painful erosion of the radius. These patients present with pain on stress loading of the upper extremity, weakness in grip strength, decreased forearm rotation, and difficulty with lifting.2
Ulnar head implant arthroplasty is designed to maintain the DRUJ, thereby avoiding ulnar impingement. An adequate soft tissue envelope repaired over the implant provides stability.
The first prosthesis used was a silicone cap designed to provide a soft end to the ulnar stump. These prostheses understandably failed under loading.
Newer designs aim to restore the ulnar head using a metallic prosthesis to articulate with the sigmoid notch.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients who have had an ulnar head resection complain of painful forearm rotation, often associated with instability of the forearm axis, decreased strength, and joint grinding.
In addition to recording the range and fluidity of DRUJ motion, the examiner must determine the stability of the joint and the contribution of ulnar impingement to the patient’s pain.
Radioulnar compression creates radioulnar impingement by external passive compression.
The examiner should encircle the patient’s distal forearm with his or her hands and apply firm compression.
A positive sign is reproduction of the patient’s pain.
Active radioulnar impingement is reproduced by active muscle contraction, specifically the brachialis.
The patient has pain lifting a load of 2 pounds with the forearm in neutral position.
Ulnar stump instability results from compromised soft tissue stabilizers of the distal stump, which tends to fall away from the radius as the forearm is rotated.
The patient is asked to actively rotate the forearm. Dorsal and palmar subluxation of the ulnar stump is visible.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard posteroanterior, lateral, and oblique radiographs of the wrist
These x-rays demonstrate scalloping of the ulnar cortex of the radial metaphysis and some corresponding pencilling of the distal ulnar stump.
Posteroanterior stress-loaded radiographs
May demonstrate impingement between the radius and ulna
The patient stands with the involved forearm facing the x-ray tube. The wrist is stress-loaded by asking the patient to hold a 2.2-kg lead cylinder with the shoulder adducted, the elbow flexed to 90 degrees, and the forearm in the position of neutral rotation.
The forearm rests on the x-ray cassette and the radiograph is then taken with the beam aligned in the coronal plane, creating a posteroanterior view of the neutral forearm.
Radiographs are obtained before and after stress-loading.
Computed tomography (CT) scanning
In patients with osteoarthritis of the DRUJ, axial scans are essential for evaluation of the extent of degenerative changes in the ulnar head and the need for total or partial replacement.
CT scanning is also essential for evaluation of the sigmoid notch for osteophytes and erosion in patients with painful ulnar head replacement.
CT scanning with forearm in pronation and supination is also useful in detecting radioulnar instability if clinical examination is equivocal.
DIFFERENTIAL DIAGNOSIS
In addition to radioulnar impingement, a patient who has pain at the DRUJ after resection of the ulnar head may have pain due to the following conditions:
Ulnar neuropathy
Painful surgical scar due to sensory nerve injury or scarring
Radiocarpal or midcarpal arthritis
NONOPERATIVE MANAGEMENT
SURGICAL MANAGEMENT
The most common indication for distal ulnar implant arthroplasty is to relieve impingement symptoms in patients who have undergone previous ulnar head resection.
Other less common indications include the following:
Treatment of patients with primary degenerative arthritis of the DRUJ who have failed to respond to splinting and steroid injections
Reconstruction of the ulna after excision of a tumor involving the ulnar head
After unreconstructable fractures of the ulnar head as either a primary or delayed procedure
Relative indication: patients with well-controlled inflammatory arthritis but well-preserved bone stock
The amount of the DRUJ that is replaced may vary for any given case.
Partial ulnar head replacement
Unconstrained replacement of the entire distal ulna with or without sigmoid notch resurfacing
Constrained total DRUJ replacement, including the sigmoid fossa of the distal radius
Partial ulnar head replacement preserves the styloid process and the attachment of the triangular fibrocartilage.
This procedure is indicated when the disease process, typically arthritis, is limited to the distal ulnar articular surface.
Contraindications include active infection, inadequate soft tissue coverage or poor bone stock, instability of the distal ulna, excessive ulnar positive variance, and degeneration at the sigmoid notch.
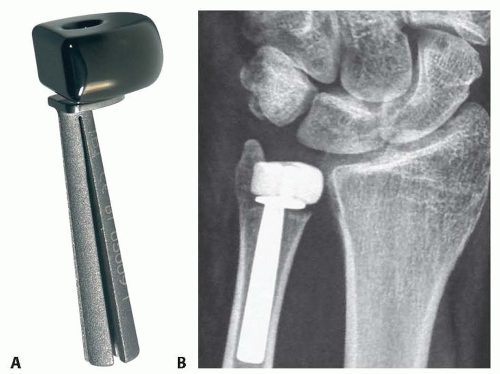
Two types of implants are available: a one-piece stemmed metal prosthesis and a two-piece prosthesis with a titanium stem and an articulating pyrolytic carbon disc that replaces the head (FIG 1).5
Long-term results of partial ulnar head replacement are not known. The articulating two-piece prosthesis has the theoretical advantage of less radius erosion from articulation with the pyrocarbon head.
Unconstrained complete ulnar head replacement is indicated for reconstruction of ulnar impingement after resection or replacement of an arthritic DRUJ associated with instability of the distal ulna. With mild instability, repair of the soft tissue envelope is adequate to restore stability. In cases with more obvious instability, an additional soft tissue procedure is indicated along with ulnar head replacement.
Ulnar head prostheses are generally spherical and made of metal or ceramic. An eccentric-shaped metallic head has been designed to more closely approximate the shape of the normal head. However, biomechanical studies have demonstrated normal tracking patterns of the distal ulna around the radius, closely simulating the normal joint, even with the use of spherical heads.8
Ulnar head prostheses may articulate with a metal-backed polyethylene resurfacing of the sigmoid notch in an unconstrained manner (FIG 2).
An adequate soft tissue envelope is essential to prevent subluxation of a complete ulnar head replacement. The triangular fibrocartilage complex (TFCC) is no longer attached to the distal ulna, making the prosthesis prone to dislocation. Thus, an essential part of the surgical technique is reconstructing the capsuloligamentous envelope surrounding the ulnar prosthesis.
Other contraindications include previous open fracture, infection in or around the joint, skeletal immaturity, and known sensitivity to the implant materials.
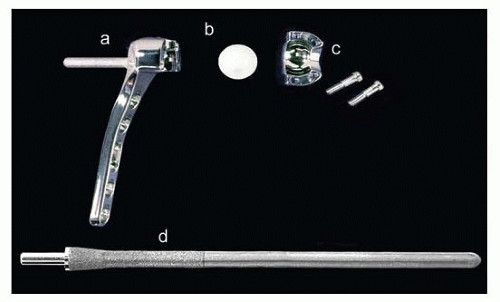
In cases of marked instability, with lack of an adequate soft tissue stabilizing envelope and ablation of the DRUJ
after trauma or tumor resection, a constrained total DRUJ replacement should be used (FIG 3).
The radial component consists of a plate with a polyethylene-lined metal sphere affixed to the interosseous surface of the radius.
The ulnar stem has a protruding peg that is captured and rotates within the polyethylene liner. The stem has limited freedom of proximodistal and limited dorsopalmar motion, simulating normal DRUJ mechanics.
Preoperative Planning
Preoperative radiographs of both sides are used for templating (FIG 4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree