Two-Part Proximal Humerus Fractures
Julie Y. Bishop
Evan L. Flatow
J. Y. Bishop: Department of Orthopaedic Surgery, Mount Sinai School of Medicine, New York, New York.
E. L. Flatow: Department of Orthopaedic Surgery, Mount Sinai School of Medicine, New York, New York.
PATHOLOGY
Risk Factors
Most fractures of the proximal occur in older, often female patients, with osteoporotic bone.38 Their cortical bone is thin, osteoporotic, and brittle, and the cancellous bone is very porous. This particular population is at high risk for poor postoperative compliance because many have poor coordination, often live alone without help, and may have limited understanding of the importance of careful protection followed by rehabilitation. Proximal humerus fractures also occur in the high-energy trauma group. Although this may result in such fractures at any age, young patients typically experience these fractures38 because their cortical and cancellous bones are of excellent quality. They are often better able to comprehend and comply with the postfracture rehabilitation protocol.
There are additional factors to consider when choosing a treatment plan and predicting outcomes in two-part proximal humerus fractures. Concomitant injuries, such as associated dislocations, nerve injuries, or rotator cuff tears, must all be considered when formulating a treatment plan. The young patient with a high-energy proximal humerus fracture and associated polytrauma will often require a different treatment plan than the treatment plan associated with an isolated fracture. Patient factors, such as alcoholism, ability to comply with postoperative care, and systemic injuries (e.g., brain injury, metabolic bone disease, parkinson, renal osteodystrophy, or any other forms of osteopenia)26 may affect outcomes and should influence the treatment choice. Functional demands, activities of daily living, patient expectations, and patient mental status must all be determined prior to treatment. Failure to properly assess these patient risk factors could certainly lead to poor results and, at times, devastating outcomes.
Mechanism of Injury
The most common mechanism of injury for proximal humerus fractures is a fall onto an outstretched hand from a standing height.49,50,57 In most cases, severe trauma does not play a significant role. Instead, trauma need only be minor to moderate because of the osteoporosis that may be present. In younger patients, high-energy trauma, such as a motor vehicle accident, is the more typical injury. Strong muscular contraction has also been proposed as a mechanism, especially for the greater tuberosity fractures,27 but this is usually seen with electric shock or seizure.47,89
Although, in theory, a direct blow to the upper arm could shatter the proximal humerus, most fractures are believed to result from indirect violence.16,28 However, it is surprising that little is known about how this actually occurs. Howard and Eloesser39 constructed an elaborate cadaver model to investigate these mechanisms. Contact with the acromion and glenoid rim, as well as traction from the rotator cuff, has been thought to initiate the fracture planes.16,28 The lower incidence of isolated greater tuberosity fractures in older patients, then, may represent a result of age-related weakening of the cuff tendons, resulting in a diminution of their contribution to an avulsion force.38
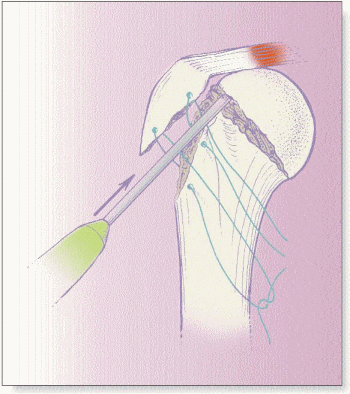
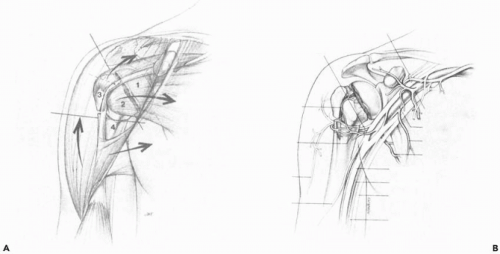
Once the fragments separate, muscle forces contribute to their displacement (Fig. 12-1A). The shaft is generally drawn anteriorly and medially by the pectoralis major.23 The greater tuberosity may be pulled posteriorly by the infraspinatus and superiorly by the supraspinatus.22,74 At other times, however, an intact rotator interval between the supraspinatus and subscapularis may limit greater tuberosity displacement. The subscapularis tends to retract medially as an isolated lesser tuberosity fragment or to rotate internally as a head segment, to which only the lesser tuberosity remains attached.74
Concomitant Injuries
Proximal humerus fractures may be isolated or may be a part of a multitrauma.86 All patients must be examined for any evidence of other fractures and injuries, especially the neck or the chest wall. In the polytrauma patient, a dramatic shoulder injury can obscure other findings. The entire upper extremity should be palpated, in particular, to rule out any concomitant wrist fractures. Rib fractures have also been reported in association with proximal humerus fractures.33 If the patient has amnesia, bilateral injuries, or a posterior fracture-dislocation, the physician must rule out a seizure disorder or electric shock.
A detailed neurovascular exam of the upper extremity is essential in all fractures of the proximal humerus (Fig. 12-1B). Axillary artery and brachial plexus injuries have been reported,33,35,58,96,106 with increasing frequency in fracture dislocations.83 The axillary artery and its lateral branches, the anterior humeral circumflex arteries, and the posterior humeral circumflex arteries are the relevant vessels when determining proximal humerus fractures. Arterial injuries that accompany proximal humerus fractures often involve the axillary artery near the origin of the circumflex arteries for several reasons: (a) this region is close to the surgical neck, whose sharp spikes are often drawn toward the artery by the pull of the pectoralis major; (b) the two circumflex origins and the lateral continuation of the axillary artery represent a “tethered trifurcation” that is unable to fall away from bone edges easily; and (c) glenohumeral dislocation dumps the head segment into this area and stretches the axillary artery across it. The finding of asymmetric radial pulses may be a subtle clue to axillary artery injuries. If vascular injury is suspected, an angiogram is indicated,.
Isolated axillary nerve injuries and mixed brachial plexus injuries are the most common neurologic injuries found after proximal humerus fractures.7,106 Although nerve lesions occur at a higher frequency with four-part proximal humeral fractures,7,75 a meticulous neurologic
exam should always be performed. Neurologic injuries associated with closed reduction methods are difficult to distinguish from those injuries that occur at the time of fracture or surgery due to the acutely injured, swollen, and painful shoulder. Thus, again, emphasizing the importance of the initial examination. Sensation should be tested over the deltoid muscle in the axillary nerve distribution, although this may be an unreliable finding. Testing for deltoid activity may be painful; however, the ability of the patient to actively set the deltoid muscle in an isometric contraction should be assessed. In addition to axillary nerve function, the motor function and sensory distribution of the musculocutaneous nerve, as well as other peripheral nerves, should be specifically examined.
exam should always be performed. Neurologic injuries associated with closed reduction methods are difficult to distinguish from those injuries that occur at the time of fracture or surgery due to the acutely injured, swollen, and painful shoulder. Thus, again, emphasizing the importance of the initial examination. Sensation should be tested over the deltoid muscle in the axillary nerve distribution, although this may be an unreliable finding. Testing for deltoid activity may be painful; however, the ability of the patient to actively set the deltoid muscle in an isometric contraction should be assessed. In addition to axillary nerve function, the motor function and sensory distribution of the musculocutaneous nerve, as well as other peripheral nerves, should be specifically examined.
Closed injury to the brachial plexus or peripheral nerves requires documentation and may be treated expectantly. Electromyography is usually reserved for late evaluation of lingering neurologic deficits. Neurologic injury should not delay the definitive management of the fracture because most nerve injuries are neuropraxias and will resolve sufficiently to allow adequate function.5 Complete lesions that do not resolve can be evaluated and treated appropriately between 3 and 6 months after the injury.
IMAGING
Classification
Classifying proximal humerus fractures has evolved in the recent past; however, controversies still exist in the choice of the best classification system and, most importantly, the implications for treatment that they may have. The Neer classification system, proposed in 1970,73 is still widely used by most orthopedic surgeons for the diagnosis and treatment of proximal humerus fractures. This classification was based on Codman’s contribution, that fractures occur along the anatomic lines of epiphyseal union, and on 26 years of clinical experience treating proximal humerus fractures. This system emphasizes the degree of displacement rather than the pattern of fracture lines. It is easy because it requires a knowledge of anatomy, not the memorization of a complex classification scheme. Fractures are classified by displacement of any of the four principal fragments. If no segment is displaced more than 1 cm or rotated more than 45 degrees, the fracture is considered a one-part fracture, regardless of the number or location of fracture lines. A two-part fracture has a single displaced segment. The most common two-part fractures are surgical neck (the shaft is separated from the head and both attached tuberosities) and greater tuberosity fractures (Fig. 12-2). Lesser tuberosity two-part fractures are rare, while anatomic neck fractures are almost never seen in isolation. Neer also categorized two-part fracture-dislocations with either anterior or posterior dislocation of the articular segment.
Accurate Radiographs
Accurate, careful radiographs are essential to plan treatment and to determine the prognosis of a two-part proximal humerus fracture. All too often, a surgeon receives inadequate oblique views from the emergency department and orders a computed tomography (CT) scan, as if this will substitute for carefully repeating and obtaining high-quality, plain radiographs. As inconvenient as it is, personally positioning the patient is usually the best way to obtain the proper information.
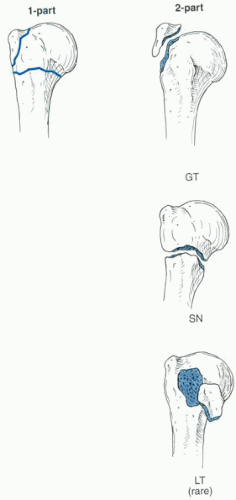
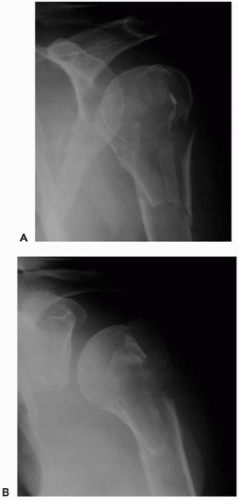
Clear delineation of the fracture pattern is best accomplished with the radiographic trauma series. This consists of an anteroposterior (AP) view of the scapula, a lateral “Y-view”
of the scapula, and an axillary view (Fig. 12-3). The lateral “Y-view” can be useful in evaluating the facets of the greater tuberosity, which has three facets into which the tendons of the supraspinatus, the infraspinatus, and the teres minor insert. Recognizing these facets on radiographs can be helpful in determining the extent of involvement of the greater tuberosity in a fracture. The axillary view is useful for correctly identifying a fracture-dislocation and for evaluating the articular surfaces of the glenoid and humerus. This view is often omitted even though its importance has been stressed by several authors over the years.5,8,18,73,94 The arm can be held in gentle abduction of about 30 degrees by a knowledgeable person so that further displacement of the fracture does not occur. However, the senior author’s preference is the velpeau axillary view, in which the arm stays in the sling, the patient leans back, and the beam is aimed down the shoulder, as the plate is placed below the shoulder. This view has the advantage of not shifting the fracture pattern because a portion of the motion required for abduction of the shoulder in the routine axillary view may occur through the fracture site.20 In this fashion, three orthogonal views may be taken without removing the arm from the sling.
of the scapula, and an axillary view (Fig. 12-3). The lateral “Y-view” can be useful in evaluating the facets of the greater tuberosity, which has three facets into which the tendons of the supraspinatus, the infraspinatus, and the teres minor insert. Recognizing these facets on radiographs can be helpful in determining the extent of involvement of the greater tuberosity in a fracture. The axillary view is useful for correctly identifying a fracture-dislocation and for evaluating the articular surfaces of the glenoid and humerus. This view is often omitted even though its importance has been stressed by several authors over the years.5,8,18,73,94 The arm can be held in gentle abduction of about 30 degrees by a knowledgeable person so that further displacement of the fracture does not occur. However, the senior author’s preference is the velpeau axillary view, in which the arm stays in the sling, the patient leans back, and the beam is aimed down the shoulder, as the plate is placed below the shoulder. This view has the advantage of not shifting the fracture pattern because a portion of the motion required for abduction of the shoulder in the routine axillary view may occur through the fracture site.20 In this fashion, three orthogonal views may be taken without removing the arm from the sling.
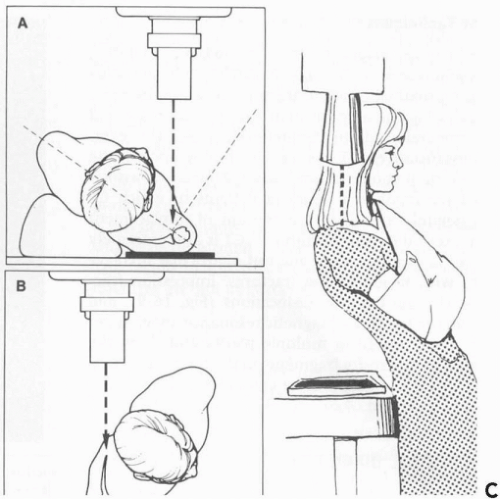
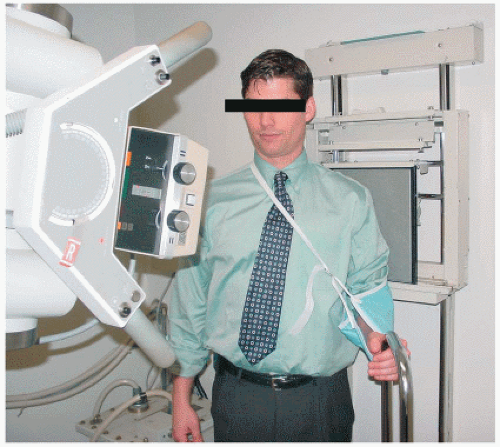
If the fracture is several weeks old and is relatively stable, the surgeon may choose to take the AP view of the scapula in slight external rotation: this gives a clear view of the greater tuberosity (Fig. 12-4). It is easily accomplished by loosening the sling, gently rotating the arm to about 20 degrees of external rotation while checking for bone crepitus, and letting the patient hold onto an intravenous pole or table edge (Fig. 12-5). Recently, the senior author’s work on the reliability and reproducibility of evaluating radiographs of the greater tuberosity was presented.81 It was found that the anteroposterior (AP) ER view as well as the AP 15-degree caudad projections best profiled the greater
tuberosity and were more accurate in their assessment of overall fracture displacement (average error of 5.1 mm). They were also the most accurate views at the level of displacement (5-10 mm), where surgery may be indicated (average error, 1.8 and 2.2 mm). Overall, multiplane radiographic imaging, which includes these views as well as the normal trauma series, will improve the diagnostic imaging accuracy and aid in determining the appropriate treatment.
tuberosity and were more accurate in their assessment of overall fracture displacement (average error of 5.1 mm). They were also the most accurate views at the level of displacement (5-10 mm), where surgery may be indicated (average error, 1.8 and 2.2 mm). Overall, multiplane radiographic imaging, which includes these views as well as the normal trauma series, will improve the diagnostic imaging accuracy and aid in determining the appropriate treatment.
Computed Tomography Scans
Although accurate radiographs allow the experienced surgeon to consistently identify displaced segments, CT is occasionally helpful to assess tuberosity displacement and articular surface involvement.94 The head may be split or have a significant impression defect, both of which may be well visualized on CT. Morris et al.70 have reported on a series of patients in which CT was helpful in judging the amount of displacement of tuberosity fractures. Posterior and medial retraction of the greater tuberosity is best seen on a transverse cut of a CT scan (or, of course, the axillary radiograph). Usually, the tuberosity fragment overlapping the articular surface is present. Computed tomography imaging has also been advocated in evaluating more complex fractures, which will be discussed in subsequent chapters.5,19,45,91,94 However, while CT has proven to be a useful adjunct, one must be aware that CT evaluation is certainly not meant to be a substitute for ideal radiographs.
Of note, CT scan evaluation of fracture patterns has been assessed in relation to interobserver and intraobserver reliability of the Neer classification system. The effect of CT on increasing reliability and reproducibility was assessed by Bernstein et al.4 The mean kappa coefficient for intraobserver reliability was 0.64 with only radiographic evaluation and 0.72 (substantial) with radiographs and CT scans. The intraobserver reliability increased while the interobserver reproducibility did not change with the addition of CT scans.
Thus, overall, a CT scan should be ordered only when good radiographs fail to show the fracture pattern clearly. Computed tomography scans are most helpful in checking for dislocations, in ruling out glenoid fractures, and in assessing posterior retraction of the greater tuberosity.
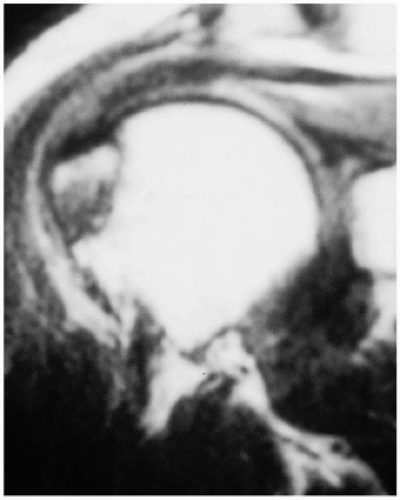
Magnetic Resonance Imaging
Although magnetic resonance imaging (MRI) scans are not often needed in the evaluation of two-part proximal humerus fractures, some nondisplaced greater tuberosity fractures may be impossible to see on radiographs. Magnetic resonance imaging, thus, may be helpful because the fracture line can be well visualized.105 These radiographically occult fractures often have associated marrow edema, which can be identified on the MRI (Fig. 12-6).62,64 Occult fractures that
are imaged acutely can have a linear or curvilinear signal that is seen within diffuse edema. Images taken within a later time frame may allow resolution of the fracture line with the persistence of edema.64 These findings have then led some to conclude that MRI can prevent unnecessary arthroscopy in patients with a clinically suspected traumatic rotator cuff tear, which is actually a subtle greater tuberosity fracture that is not visable on plain radiographs.84
are imaged acutely can have a linear or curvilinear signal that is seen within diffuse edema. Images taken within a later time frame may allow resolution of the fracture line with the persistence of edema.64 These findings have then led some to conclude that MRI can prevent unnecessary arthroscopy in patients with a clinically suspected traumatic rotator cuff tear, which is actually a subtle greater tuberosity fracture that is not visable on plain radiographs.84
SURGICAL NECK FRACTURES
The principle involved in treating minimally displaced fractures is early protection combined with gradual mobilization. Although, in theory, more than 1 cm of displacement makes the surgical neck “displaced,” in practice, in most elderly patients, surgeons accept almost any degree of displacement as long as there remains some solid bone contact. Angulation is well compensated for by shoulder motion or can be adjusted by small manipulations after a week or so, after the fracture becomes sticky. Elderly patients with reduced demands (i.e., more likely to accept a stiff shoulder), with poor health, and who are poor rehabilitation candidates are more likely to receive nonoperative treatment. In young patients, less than 50% shaft diameter displacement and less than 45-degree angulation in the dominant arm are acceptable indications for nonoperative treatment, although, in some individual cases, surgery may be considered for less displacement or angulation.
Most patients are placed in a sling for the first week to 10 days and are instructed to pull a shirt over it at night. Swathes rarely stay on and are uncomfortable. Hand, wrist, and elbow motion begins immediately. On the next visit, the physician holds the patient’s elbow and flexed forearm in one hand and palpates the tuberosities and biceps groove with the other while the patient leans over. If the proximal and distal humerus “move as a unit,” the patient is started on gentle pendulum range of motion. If, on the other hand, a slip or give is felt in association with some bone crepitus or catching, the patient is left immobilized for another week and is then reassessed. At 3 or 4 weeks, if radiographs are unchanged and the bone again feels solid, gentle assistive exercises (pulley elevation, external rotation with a stick, extension with a stick) are begun, along with formal physical therapy. At 6 weeks, there is rapid progression to terminal stretches and light resistive exercises.
Koval et al. followed 104 patients with minimally displaced proximal humerus fractures for at least 1 year after treatment in this fashion.51 Ninety percent of these patients had no pain, and most patients achieved 90% of their contralateral shoulder motion. Motion was better when formal physical therapy had been started early.
There are only a few, rare indications for surgical treatment of a minimally displaced proximal humerus fracture: ipsilateral neurovascular injury requiring exploration, repair, or protection; an open fracture; or multiple trauma requiring mobilization as fast as possible.
Closed Reduction
If a two-part surgical neck fracture is displaced at initial presentation, closed reduction may often be attempted. This can usually be performed if there is an unimpacted fracture without bone contact. A hematoma block can often be helpful, or this maneuver can be performed in the operating room, with the option of operative intervention, if a stable reduction cannot be attained. It is imperative, when using the C-arm image intensifier in the operating room, to drape the patient so that the arm is entirely free to move. The image intensifier must be able to easily project a true anteroposterior and axillary view of the fracture site. The arm is then adducted and flexed 90 degrees, thus relaxing the pectoralis. A translation force (usually posteriorly and laterally, because the typical fracture is anteriorly angulated and is anteromedially displaced) is applied to reduce the deformity, while longitudinal traction is applied. After a reduction is felt, a gentle attempt to reimpact the bones is made. If the fracture is reducible and stable, treatment as outlined for minimal displacement is continued for 4 weeks rather than 7 to 10 days (Fig. 12-7). If the fracture is reducible but unstable, percutaneous pins should be considered. If a reduction cannot be achieved, open reduction and internal fixation are considered. Interpositioning the biceps tendon, capsule, or subscapularis may prevent closed reduction. Significant comminution at the surgical neck fracture site may preclude a stable closed reduction.
Closed Reduction and Percutaneous Pinning
Technique
Closed reduction and percutaneous pinning of unstable two-part proximal humerus fractures is a well-known technique for treating these kinds of fractures and, typically, should be reserved for patients with good bone quality and a fracture that can be reduced closed but is unstable and cannot maintain the reduction.3,41 It does offer some theoretical advantages over open techniques because it limits soft-tissue trauma and any associated morbidity. It does not add an additional risk to the vascular supply of the humeral head articular segment; however, there is an inherent risk to the surrounding neurovascular structures during the pinning process.87 Lateral pins should be distal enough to avoid injuring the anterior branch of the axillary nerve; however, the pin must be placed above the deltoid insertion to avoid injuring the radial nerve. Anterior pins may risk injuring the musculocutaneous nerve, cephalic vein, and the biceps tendon. Also, multiple images should be taken to avoid penetrating the humeral head cartilage. Finally, this technique demands a compliant patient who will agree to maintain the immobilization of his or her arm
and who is available for close follow-up of the pin positions and skin condition.
and who is available for close follow-up of the pin positions and skin condition.
 Figure 12-7 Displaced surgical neck fracture in a 76-year-old female. (A) Initial injury anteroposterior view. (B,C) Three months after closed reduction in the operating room. Fracture is healed on the anteroposterior and axillary views. (D,E) Patient has regained symmetrical motion in forward elevation and external rotation 3 months after closed reduction.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|