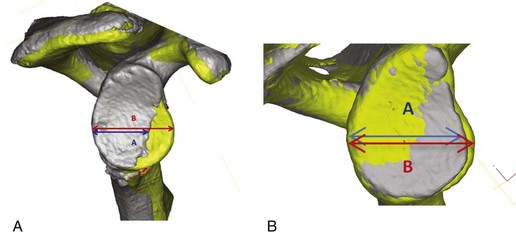
Chapter 15 Traumatic anterior dislocation of the glenohumeral joint is frequently associated with disruption of the anteroinferior capsulolabral structures, the so-called Bankart lesion.1,2 Surgical treatment of Bankart lesions has demonstrated long-term success in reducing the rate of recurrent instability after first-time anterior shoulder dislocation (10% vs. 58% for 3- to 10-year results) when compared with nonoperative treatment.3 However, glenohumeral dislocation is also associated with a high prevalence of osteoarticular injury, including glenoid bone loss (bony Bankart lesions) and compression fractures of the posterosuperior humeral head (Hill-Sachs lesion).2,4 Frequently, recurrent anterior glenohumeral instability is associated with bone loss. Hill-Sachs defects are present in up to 100% of first-time anterior dislocations, and anteroinferior glenoid bone deficiency has been reported in 22% of primary dislocations.1,2,4–6 Because the glenohumeral joint is minimally constrained, bony defects can significantly alter the balance of static and dynamic forces that contribute to shoulder stability. Therefore recognition of bony Bankart and Hill-Sachs lesions is critical for formulation of a thoughtful treatment plan and prevention of recurrent instability. Bankart repair with anterior glenoid bone loss can lead to unpredictable outcomes and a high failure rate. Burkhart and de Beer7 retrospectively reviewed 194 cases of arthroscopic Bankart repair, dividing patients into two groups—those with significant bone defects of the glenoid or humeral head, and those without such defects. If a soft-tissue repair was performed in patients with significant bone defects (inverted-pear glenoid or “engaging” Hill-Sachs lesion), there was a 67% recurrence rate compared with 4% in patients without significant bone defects. Several other authors have demonstrated similar results, suggesting that anterior glenoid bone loss as an important risk factor for recurrent shoulder instability.8–11 Hill-Sachs lesions also play a role in recurrent instability. Rowe and colleagues12 initially reported a 76% incidence of Hill-Sachs lesions in failed instability surgery, and Burkhart and de Beer7 reported engaging Hill-Sachs lesions to be associated with failed instability surgery in 100% of cases. Boileau and colleagues9 reported that 84% of patients with recurrent traumatic anterior shoulder instability had a Hill-Sachs lesion and that large lesions were significantly correlated with recurrent instability. Several cadaveric studies have also demonstrated a decrease in glenohumeral stability after the creation of posterosuperior humeral head bone defects.13,14 Balg and Boileau15 developed a preoperative assessment to determine which patients are at risk for recurrent instability after a Bankart repair, identifying the presence of a Hill-Sachs lesion and glenoid bone loss as important factors to consider in planning surgical reconstruction. Historically, the goal of treatment has been to create a stable glenohumeral joint and prevent recurrent instability. Numerous nonanatomic techniques have been described, including transfer of the coracoid process16 (Bristow and Latarjet procedures), open capsular shift17,18 (Putti-Platt and Magnusson-Stack procedures), infraspinatus transfer into the Hill-Sachs defect19 (Remplissage), and rotational humeral osteotomy.20 More recently, anatomic reconstruction techniques have also been described to address both glenoid and humeral head bone loss. The use of iliac crest autograft,21 distal tibia allograft,22 femoral head allograft,23 or glenoid allograft24,25 has been reported to restore normal glenoid contour and glenohumeral biomechanics. Similarly, humeral head convexity can be restored with a humeroplasty,26,27 arthroscopic mosaicplasty with fresh-frozen allograft plugs,28 osteoconductive graft plugs,29 and humeral head allograft reconstruction.30–32 These anatomic techniques theoretically allow for improved postoperative motion and decrease the risk of recurrent instability while avoiding the complications of nonanatomic techniques.33,34 The physical examination proceeds in a systematic fashion, beginning with inspection. Any previous surgical scars are noted. Active and passive range of motion and rotator cuff strength are tested and compared with the contralateral unaffected arm. Instability is assessed in the anterior, posterior, and inferior directions. Instability is graded on a three-point scale. Typically, patients with soft-tissue Bankart lesions will experience apprehension at 90 degrees of shoulder abduction and 90 degrees of external rotation; in those with bone defects the examiner may note apprehension at lower angles of abduction and external rotation (ABER), termed the bony apprehension test.35 Because pain may limit the in-office examination, all findings are verified later with a complete examination under anesthesia. The goal of osteoarticular allograft reconstruction is to restore normal shoulder biomechanics. Glenoid bone defects decrease the available articular arc length so that during positions of increasing ABER, the humeral head subluxes or dislocates anteriorly owing to a lessening of the glenoid fossa concavity, a loss of the anteroinferior labrum (“bumper”), and a loss of the concavity-compression mechanism for dynamic support.36–38 Similarly, large Hill-Sachs lesions decrease the available arc of motion and, if oriented properly, can “engage” on the anterior glenoid rim.7 In the case of concomitant glenoid and humeral head bone loss, the amount of articular arc length may be further compromised, exacerbating feelings of instability. Although imaging modalities such as CT and MRI can show the size and location of bony defects, diagnostic arthroscopy provides the most comprehensive and dynamic method of evaluation. There is no consensus regarding the amount of glenoid or humeral head bone loss required to cause recurrent instability and justify an anatomic reconstruction procedure. Rowe and colleagues1 originally described glenoid lesions as significant if they involve 30% of the articular surface. On the basis of a biomechanical study, Gerber and Nyffeler39 found that anteroinferior glenoid defects with a total length greater than half the maximum anterior-to-posterior diameter decreased the resistance to dislocation by 30%. Bigliani and co-workers8 reported a 12% recurrence rate in patients with glenoid rim fractures after Bankart repair and recommended a coracoid transfer for bone loss greater than 25% of the anteroposterior diameter of the glenoid. Burkhart and de Beer7,40 suggested that there is a high chance of recurrent instability if the anterior-to-posterior glenoid diameter is less than the diameter above the midglenoid notch, termed the inverted pear glenoid. The authors showed that when the glenoid bare spot is used as a reference for arthroscopic measurement, a 6-mm loss of anterior glenoid rim bone results in a 25% deficiency of the glenoid diameter. The consensus of these and other authors is that glenoid bone grafting is recommended for defects greater than 25% to 30% of the articular surface. Hill-Sachs lesions that engage on the anterior glenoid rim in functional positions should be addressed surgically. Several cadaver studies have evaluated the effect of lesion size on shoulder stability. Sekiya and colleagues14 reported that defects as small as 12.5% of the humeral head diameter can cause changes in glenohumeral biomechanics that may alter stability. Kaar and co-workers13 created humeral head defects of varying radii and showed a significant decrease in shoulder stability with defects of 5/8 radius. Furthermore, Yamamoto and colleagues41 described the concept of a “glenoid track,” in which Hill-Sachs lesions that lie medial to this zone can engage as the humeral head overrides the glenoid rim in the presence of humeral head or glenoid bone defects. The size and orientation of the humeral head or glenoid bone defect are determined preoperatively through CT or MRI. We have developed a technique for measuring glenoid bone loss we termed contralateral overlay. The patient’s normal contralateral glenoid is flipped and superimposed onto the affected glenoid. The anterior-posterior width of the affected glenoid is compared with the normal glenoid width. This technique has the advantage of detecting subtle glenoid bone loss and better quantifying larger bone loss (Fig. 15-1). Fresh-frozen allograft is selected from a tissue bank and is size- and side-matched based on preoperative measurements. A thorough discussion of the potential risks associated with the use of allograft tissue is undertaken with the patient. Informed consent is obtained.
Treatment of Combined Bone Defects of Humeral Head and Glenoid
Arthroscopic and Open Techniques
Preoperative Considerations
Physical Examination
Indications and Contraindications
Surgical Planning
Musculoskeletal Key
Fastest Musculoskeletal Insight Engine