After reading this chapter and completing the exercises, the reader will be able to: 1. Identify and describe the key components of a treatment note. 2. Identify and describe the key components of a progress note. 3. Appropriately document components of treatment notes and progress notes using a modified SOAP format. Although there are no formal guidelines from either APTA or CMS regarding the structure of treatment or progress notes, such documentation can become unwieldy without some organization. The SOAP note is a commonly used format and is one with which most medical personnel are familiar (see Chapter 2 for the history and development of the SOAP note). The SOAP format is relatively easy to master and provides a quick format for writing a treatment note. This chapter presents a format for writing both treatment notes and progress notes using a modified SOAP format. The acronym SOAP stands for subjective, objective, assessment, and plan. This format was discussed briefly in Chapter 2 and is presented here as a framework for treatment and progress note documentation. However, the original design for use of the SOAP note is not how it is currently used by most medical professionals. The SOAP note was designed to promote a sequential rather than an integrative approach to clinical decision making and was linked to the problem-oriented medical record, which is no longer routinely used. However, with some modifications the SOAP note can provide the foundation for efficient, effective functional outcomes documentation in rehabilitation. The figures and tables in this chapter outline key components of these notes to meet criteria necessary for optimal clinical decision making, third-party payment, and legal purposes. Because treatment notes must serve such diverse purposes, there may be a tendency for therapists to write excessively long notes. Strategies for simplifying documentation are provided in Box 12-1. Furthermore, the case examples at the end of the chapter demonstrate how such notes are modified for different patients in different practice settings. Treatment notes are written for each encounter a PT or PTA has with a patient (Case Examples 12-1, 12-2, and 12-3). Although APTA documentation guidelines and most third-party payers require documentation for each physical therapy encounter, the format of treatment note documentation is at the discretion of each institution. Treatment notes are written for four distinct reasons: 1. Legal documentation. A treatment note importantly provides a legal record of what was done in a therapy session and why. For this reason, documentation of the specifics of the interventions performed and the patient’s reaction to those interventions is critical. 2. Third-party payment. Third-party payers typically request that treatment notes be provided as proof of service. Medicare, for example, requires documentation to create a record of all treatments and skilled interventions to justify the use of billing codes. 3. To facilitate functional outcomes and clinical decision making. Writing a treatment note that focuses on functional outcomes helps to maintain a therapist’s attention on patient-specific goals. Each treatment note allows the therapist the time to reevaluate the patient’s progress and goals and to consider changes to the plan of care. 4. As a record for other therapists in case of absence. In the event that a therapist is absent, it is important for any covering therapist to have a complete record of the specific interventions that were performed with a patient. The framework for treatment note documentation includes goals (G), subjective (S), objective (O), assessment (A), and plan (P) (Figure 12-1). In the Subjective section of the treatment note, the therapist documents the patient’s subjective respon-ses to interventions and any changes in participation or activity limitations. This section could include any relevant statements or reports made by the patient, patient’s family members, and/or caregivers. The purpose of this section is to detail the patient’s own perception of his or her condition, which can relate to impairments (e.g., pain), activities (e.g., ability to walk), or participation (e.g., ability to work). Box 12-2 provides more information on documenting pain in treatment notes. The focus of the Objective section is twofold: (1) to document the results of any tests and measures performed, specifically those that relate to achievement of the stated goal(s) (Status Update), and (2) to provide details of the interventions performed (Rx) (see Case Examples 12-1, 12-2, and 12-3). The Status Update should include any examination findings that were performed or observed (e.g., range of motion, walking speed). Documentation of the interventions (Rx) should include the procedural interventions that were performed, including location, frequency, intensity, duration, and/or repetitions, as appropriate. Some of this information can be recorded in table or flowchart form. However, the documentation must clearly show evidence of skilled intervention and the interaction between the patient and therapist (see Chapter 15).
Treatment Notes and Progress Notes Using a Modified SOAP Format
Modified SOAP Format
Treatment Notes
FRAMEWORK FOR TREATMENT NOTE DOCUMENTATION
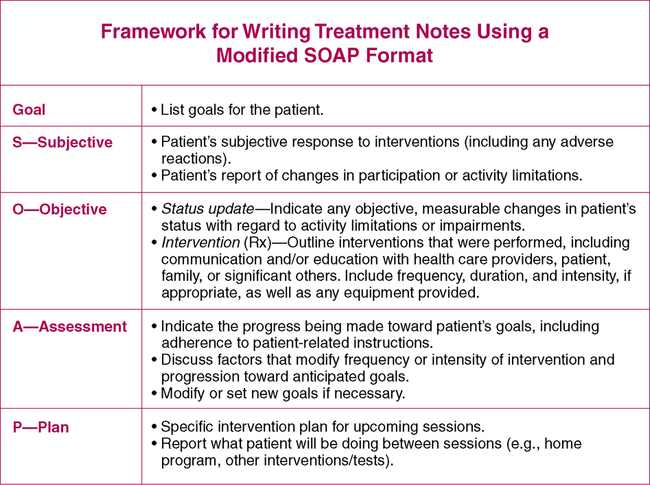
Subjective (S)
Objective (O)
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Treatment Notes and Progress Notes Using a Modified SOAP Format
Only gold members can continue reading. Log In or Register to continue







