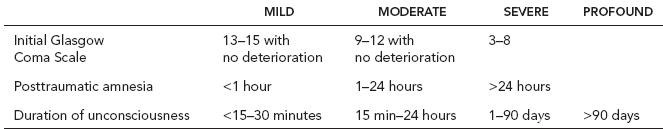
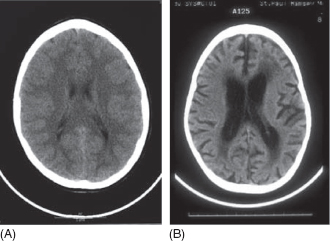
17 TRAUMATIC BRAIN INJURY Linda E. Krach, Mark E. Gormley, Jr., and Marcie Ward EPIDEMIOLOGY Traumatic brain injury (TBI) is a major cause of death and disability in children. It is the leading cause of death in children over 1 year of age. In 2009 to 2010, the Centers for Disease Control (CDC) reported that TBI resulted in a rate of 2,193.8/100,000 emergency department (ED) visits, 57/100,000 hospitalizations, and 4.3/100,000 deaths in the 0 to 4 age group and a rate of 888.7/100,000 ED visits, 23.1/100,000 hospitalizations, and 1.9/10,000 deaths for those between the ages of 5 and 14 years of age (1). The incidence of pediatric TBI peaks at two separate periods: below age 5 and in mid-to-late adolescence. The incidence of hospitalization for TBI has been reported to be 125 per 100,000 children per year in the 15- to 17-year age group (2,3). Males are more likely to sustain TBI than females, at a ratio of approximately 60% to 40% (4). Falls are the leading cause of injury in all those aged 0 to 14, but motor-vehicle-related causes increase over age 4 (5). From 2001 to 2009, the rate of reported concussion among those under 19 years of age rose 5% and in 2009, an estimated 248,418 children (age 19 or younger) were treated in U.S. EDs for sports- and recreation-related injuries that included a diagnosis of concussion or TBI (5). The leading cause of TBI-related death for children under age 4 was nonaccidental trauma (5). Children with a history of attention deficit hyper-activity disorder (ADHD) are at a greater risk to sustain TBI than those without it. ADHD affects approximately 6% of children, has a male predominance, and a hereditary tendency. Of children who sustain TBI, prevalence of preinjury ADHD is noted to be between 10% and 20% (6). Some authors have also evaluated the incidence of TBI in the United States by race. Langlois and colleagues (7) evaluated information from the National Center for Health Statistics. They reported a significantly higher rate of both hospitalization and death due to traffic/motor-vehicle-related causes in children aged 0 to 9 in Blacks compared to Whites. Another group reported their experience in a regional trauma center and concurred that traffic/motor-vehicle-related accidents were more frequently seen in minority children; however, there was no difference in death rates or the severity of brain injury (7). A recent report of the prevalence of TBI from a birth cohort of individuals between the ages of birth and 25 years in New Zealand indicated that the average incidence was from 1.10 to 2.36 per 100 per year with an overall prevalence of approximately 30% with 10% meeting criteria for moderate to severe injury (8). COSTS OF INJURY The costs associated with pediatric TBI are significant. In a study of hospital resource utilization for pediatric TBI in the year 2000, Schneier and colleagues (3) reported that more than $1 billion in hospital charges was generated for TBI patients less than 17 years of age. A survey study of needs after hospitalization reported that at 3 months after injury, 62% of children hospitalized for at least one night after TBI received at least one outpatient health care service during the interval since injury and 26% had unmet needs. At 12 months, 31% were reported to have unmet needs (9). The cost of TBI to families is something that is difficult to quantitate. However, Hawley and colleagues (10) published a report concerning parental stress after TBI in children and adolescents. The Parenting Stress Index and General Health Questionnaire results of parents of children with hospitalization of greater than 24 hours for TBI were compared to the same measures administered to a control group of parents that was identified by the subject parents. Loss of income due to the TBI was reported by 44.3% of families. For those with a child with a severe TBI, it was 69%. Also, parents of children with TBI were found to have significantly greater stress and poorer psychological health than the comparison parents. Parents of children with TBI were noted to have clinically significant levels of stress in 41% of the cases (10). The cause of injury differs by age. Nonaccidental trauma is responsible for 17% of brain injuries in infants and 5% in those aged 1 to 4. It causes a disproportionate percentage of severe TBI, resulting in 56% and 90% of severe injury in these two age groups (11). Motor-vehicle-related injuries are more common in adolescents than young children, accounting for 66% and 20% of TBIs in the respective age ranges (2). Falls cause 39% of TBI in those under age 14, and are especially common in those under age 5 (4). Falls are the leading cause of injury in children under age 4 (5). ASSOCIATION WITH OTHER INJURIES It is common for TBI to occur in association with other injuries. Children with more severe injury are more likely to have been injured in a traffic-related accident and to have associated injuries (9). It has been reported that about 50% of children with TBI have other injuries as well (12). The presence of chest and abdominal injuries has been associated with decreased survival (13,14). In one study, undetected fractures during the acute care stay were found in 16 of 60 children with TBI, some having more than one fracture (13,14). PATHOPHYSIOLOGY PRIMARY INJURY AND SECONDARY INJURY It is likely that the mechanism and consequences of TBI in children differ from those in adults for both primary and secondary injuries. Children have a relatively large head and weak neck musculature, higher brain water content, and lack of myelination (15). Primary injuries related to impact and deceleration and rotational forces can be influenced by these factors. It has been suggested that forces could be more easily transmitted to deeper brain structures as a result of lack of myelination and higher brain water content (15). Primary injury related to mechanical forces includes contusions on the surface of the brain, where the brain can impact against the inner surfaces of the skull (usually focal gray matter injury) and the shearing-type injury that is associated with deceleration and rotational forces (usually diffuse white matter injury or at gray–white interfaces). Primary injury results from mechanical disruption of membranes and axons (16,17). Secondary injuries occur due to complications or other events after the initial trauma. Potential causes of secondary injury include hypotension, hypoxia, vasospasm, infarction, prolonged seizure activity, and diffuse edema, resulting in increased intracranial pressure and a decrease in cerebral perfusion pressure (16,18). Early management of TBI has a goal of preventing secondary injury. Unfortunately, there are no guidelines concerning cerebral perfusion pressure and intracranial pressure targets for children with TBI. Values are thought to be age-dependent (19). Contributing to both primary and secondary injury in TBI are cascades of biochemical events. Injury evolves as the cascade is initiated and progresses. Mechanisms initiating these cascades include cellular power failure, acidosis, overstimulation of excitatory neurotransmitter receptors, lipid membrane peroxidation, increase in intracellular calcium, and cellular damage by free radicals (2,16). With increasing knowledge about the biochemical processes involved, researchers are attempting to identify biomarkers in serum and cerebrospinal fluid (CSF) that will assist in diagnosis and prognostication regarding the outcome of TBI (19–22). Likewise, additional information is being sought utilizing magnetic resonance spectroscopy (MRS). In Suskauer and Huisman’s review of MRS evidence, H-MRS data obtained shortly after TBI has predictive value for long-term behavioral and cognitive outcomes. Several studies have shown decreases in N-acetyl aspartate (NAA) after TBI and neurometabolite abnormalities also are predictive of overall outcome in pediatric TBI (23). Babikian and colleagues (24) found that NAA on MRS scans acquired 2 to 10 days after TBI correlated moderately to strongly with cognitive testing at 1 to 4 years postinjury. Also, mean NAA/creatinine ratio explained more than 40% of the variance in cognitive scores. They hypothesize that these values might be of assistance in predicting long-term outcome soon after injury when length of unconsciousness is not as yet known. DIFFUSE SWELLING AND SECOND IMPACT SYNDROME It is more common for children to experience diffuse cerebral swelling than adults (19,24,25). This could be due to increased diffusion of excitotoxic neurotransmitters through the immature brain, an increased inflammatory response in the developing brain, or increased blood–brain barrier permeability after injury in the immature brain (25). When a lucid interval is noted in children prior to deterioration in neurologic functioning post-TBI, it is likely due to the development of cerebral edema, in contrast to this phenomenon in adults being most commonly related to a focal mass lesion (2,26). This diffuse cerebral swelling is associated with a poor outcome (27). Children may experience impaired cerebral autoregulation after severe TBI (28,29). Cerebral blood flow varies with age, being approximately 24 cm/s in healthy newborns, 97 cm/s in children aged 6 to 9 years, and then decreasing to the adult value of approximately 50 cm/s (28). Some studies have suggested that children with TBI have a lower middle cerebral artery flow rate and therefore hypoperfusion is common (28). Another phenomenon associated with cerebral swelling is called second impact syndrome, and is said to occur after repeated concussion in children and adolescents. Brain swelling can be severe, even fatal, and develops after seemingly minor head trauma in an athlete who is still symptomatic (though at times subclinically) from a previous concussion (30). Second impact syndrome is a theoretical condition with only a few case reports available. The theory describes an initial injury (the first concussion), which deranges the brain’s autoregulatory and metabolic systems enough to produce vascular engorgement and poor brain compliance. This allows marked changes in intracranial pressure with small changes in intracranial volume (30). Second impact syndrome presumes that the brain cells are in a vulnerable state after the initial concussion. Minor changes in cerebral blood flow during the second concussion result in an increase in intracranial pressure and ultimately apnea due to herniation, cerebral ischemia, and brain death (31,32). Also, there have been reports of diffuse cerebral swelling after mild TBI in sports, usually occurring in male adolescents (32). NONACCIDENTAL TRAUMA Nonaccidental TBI is a special subset of TBI in children. It has been described as having a clinical triad of subdural hemorrhage, retinal hemorrhage, and encephalopathy, and is commonly associated with the history given, being incompatible with the severity of the injuries, and the injuries being unwitnessed and inflicted by a solitary care provider (33). Classically, this so-called shaken baby syndrome has been described as being due to shaking alone causing tearing of bridging veins and rotational forces causing diffuse brain injury. More recent studies have indicated that there is most likely an impact in addition to the shaking episode(s). Often, nonaccidental brain injury in young children is also accompanied by a delay in seeking medical attention, potentially resulting in a hypoxic component to the mechanism of injury (18,21,33). IMPLICATIONS OF PLASTICITY One must consider the effect of normal developmental activities of the immature brain on the mechanisms of developing damage after TBI. Apoptotic death of neurons is a part of plasticity and normal brain development. Does this result in the developing brain being more susceptible to activating the apoptotic cascade than the adult brain (15,25,34)? If so, this could help to explain the poorer prognosis for functional outcome for those injured at a very young age (34). In one animal study of post-trauma apoptosis, for a specific developmental age, the areas that had the highest density of programmed cell death were also noted to have high numbers of apoptotic cells in general (15). It may also be possible that excitatory neurotransmitter release could result in excessive stimulation of some pathways and stimulate the development of abnormal connections or that decreased excitatory activity could decrease connections (34). This implies that the relatively high plasticity of the developing brain could actually have a negative impact on the overall outcome after diffuse TBI and be at least partially responsible for the poorer outcomes seen in those injured at a very young age. In a discussion of plasticity after early brain insult, Anderson and colleagues (35) conclude that neither plasticity nor vulnerability theories explain the range of functional outcomes seen and that multiple factors including the extent and severity of injury, age, and environmental influences such as family, sociodemographic factors, and interventions influence outcome as well. Evaluation at too young an age will prevent the identification of problems such as executive dysfunction as those skills do not emerge until later in life, supporting the need for long-term follow-up in children with TBI. GROWING SKULL FRACTURE A rare complication of skull fracture in children is a growing skull fracture. It is reported to occur when a linear skull fracture in a child under age 3 is accompanied by a dural tear and a leptomeningeal cyst develops. Fluid pulsations result in bone erosion and a palpable skull defect that requires surgical repair (36–38). A series of eight children with growing skull fractures had MRI evidence of a zone of signal intensity similar to brain contusion or CSF through the margins of the fracture, leading to the conclusion that MRI can be useful in diagnosing growing skull fracture early after injury (38). NEUROIMAGING Computerized tomography (CT) scans are typically obtained early after significant TBI. This relatively rapid imaging study is helpful in evaluating whether there is a condition that requires prompt neurosurgical evaluation and intervention (39–42). Specifically, it is helpful in detecting extra-axial hemorrhage, fractures, acute hydrocephalus, or parenchymal hemorrhages that are relatively large. However, the presence of a skull fracture is not indicative of intracranial pathology (40). MRI is more sensitive for the detection of intraparenchymal lesions than CT scan, but takes longer than CT and often cannot be done early postinjury due to the child’s medical instability and need for supportive interventions. It is advisable, however, to obtain MRI when the child’s condition allows it. Different MRI techniques can be used to evaluate for specific abnormalities (42). Susceptibility-weighted imaging was shown to identify a greater number of lesions than other techniques in one study comparing outcomes from pediatric TBI and imaging findings (39). Others have also reported association between the volume of lesion and severity of injury (43). The total amount of diffuse axonal injury (DAI) is better demonstrated using fluid attenuated inversion recovery (FLAIR) sequences and may be more important than localized injury for outcome prediction. Diffusion weighted imaging (DWI) is also helpful in detecting DAI in children. Galloway and colleagues (44) reported that the contrast between uninjured immature brain and injured tissue is improved with this technique. Other authors have compared neuropsychological outcomes and imaging findings longer term after injury. One study of 14 children aged 10 to 18 years, 6 to 12 months after mild to moderate TBI and a matched comparison group used diffusion tensor imaging (DTI) to evaluate white matter. Authors reported that the groups had no difference in overall intelligence, but did demonstrate differences in processing speed, working memory, executive function, and behavioral problems. Also, the TBI group had lower fractional anisotropy (FA) in three white matter regions: inferior frontal, superior frontal, and supracallosal. FA in the frontal and supracallosal regions correlated with executive function. Supracallosal FA also correlated with motor speed and behavior problems (45). Another group reported DTI findings in an acutely injured child with normal CT imaging. DTI demonstrated temporary marked increase in anisotropy in large areas of the cortical and subcortical right hemisphere at 18 hours after injury. At 135 hours postinjury, subtle changes in anisotropy were present (46). Others have also noted that FA is related to injury severity including Glasgow Coma Scale (GCS) and Glasgow Outcome Scale (GOS) at 3 months postinjury (47); other investigators have found that increasing FA over time after TBI may be indicative of functional recovery (23). Late after injury, several different imaging findings can be used to assess global change in the brain. These include cerebral diffusivity, corpus callosum volume, and volumes of brain and ventricles. Increased diffusivity is thought to be related to an increase in the extracellular space. In young children who experience TBI, late cerebral atrophy or decreased total brain volume could be related to tissue loss due to the injury itself or impaired brain growth. In typically developing individuals, white matter is reported to increase by 12.4% from age 4 to 22 (17). One study of children and adolescents at least 6 years after TBI found a correlation between corpus callosum volume and processing speed and visuospatial abilities. Ventricular volume did not correlate as well with results of neuropsychological testing. Corpus callosum is reported to continue to increase in size in typically developing individuals into early adulthood (48). It is imperative to evaluate scans over time to see the full extent of damage (41). Functional magnetic resonance imaging (fMRI) has been reported to be useful in adults in the assessment of individuals with disorders of consciousness. There has been a recent case report indicating that this might also be of use in children in minimally conscious states. Nicholas and colleagues (2014) noted fMRI activation in a child in response to stimuli that were personally relevant, including the child’s name and a familiar voice, suggesting that this demonstrated preserved cognitive function (49). ELECTROENCEPHALOGRAPHY EEGs are commonly obtained for children who have sustained TBI. In the practice parameter developed by the American Academy of Neurology concerning antiepileptic drug (AED) prophylaxis in severe TBI, the authors note that in their review of studies, they did not find sufficient data to be able to make a recommendation concerning the use of EEG (50). In one report of 22 children between the ages of 1 week to 14 years at the time of TBI, the degree of EEG abnormality (mild, moderate, or severe) combined with admission GCS were predictive of outcome in the young children. This was not the case for older children. The degree of EEG abnormality was statistically significantly correlated with full-scale IQ, attention and executive function, and memory (51). Additional evaluation of the usefulness of EEG in predicting outcome is needed. INJURY SEVERITY The main tools used for classification of brain injury severity are the GCS, length of posttraumatic amnesia (PTA), and duration of unconsciousness. Each has its merits and drawbacks. GLASGOW COMA SCALE The GCS has found wide clinical application since it was first published in 1974 (52). It rates a person’s verbal, motor, and eye-opening responses on a scale of 3 to 15. It has the advantages of being simple, having a relatively high degree of interobserver reliability, and having the ability to be determined shortly after injury (53). A score of 8 or less is considered to be coma and classified as severe injury, 9 to 11 as moderate injury, and 12 to 15 as mild injury. There have been studies that indicate that a GCS score of 5 or lower instead of 8 or lower should be considered as severe injury in children, as scores lower than 5 have been associated with a good outcome (13,54–56). Although the GCS was initially formulated to aid in acute triage and in neurosurgical management, many studies have correlated outcome with initial scores. There is, however, wide patient-to-patient variability. Some have noted that the GCS in the field is more predictive of survival (14,56), and GCS later in the postinjury course (particularly the motor component at 72 hours after injury) is a better predictor of disability (14,56). Adaptations of the GCS have been made to facilitate evaluation of children (57,58). Other refinements of the scale include the number of days until a patient returns to a GCS of 6 or 15. POSTTRAUMATIC AMNESIA AND CHILDREN’S ORIENTATION AND AMNESIA TEST The duration of PTA is another commonly used indicator of injury severity. There is general agreement that the duration of PTA is directly correlated with the severity of injury (59–61). Compared with GCS, PTA has the merit of a longer period of observation. However, there is no generally accepted and easily applied method for determining the duration of PTA, especially in children. Assessments must be adapted, as appropriate, according to an individual’s age (61). The Children’s Orientation and Amnesia Test (COAT) has been helpful in evaluating the length of PTA. It was designed to assess cognition serially during the early stage of recovery from TBI in children. The COAT is composed of 16 items evaluating general orientation, temporal orientation, and memory. The duration of PTA is indicated by the number of days COAT scores are in the impaired range (62). Although this test should be useful in prospective outcome studies of children without profound injury, it has a major disadvantage because it takes 5 to 10 minutes to administer and, therefore, has not become a routine assessment on most clinical services. It has also been shown to be sensitive to nontraumatic impairment. For example, children receiving special education services fall within the impaired range, and the COAT, therefore, should be interpreted with caution (63). DURATION OF UNCONSCIOUSNESS Duration of unconsciousness is another measure of severity and has the advantage of longer observation than GCS. It is also easier to recognize than the duration of amnesia in children and is more easily determined in retrospective chart reviews. Unconsciousness has been defined as the inability to respond to the environment in any adaptive, meaningful way. Children can have sleep–wake cycles and still be considered unconscious (64). This is the most appropriate measure in series of more severely injured children who are unconscious for many weeks, many of whom never regain recent memory. A study conducted by Massagli and colleagues (56) concluded that there was a strong correlation between the length of time to reach GCS of 15 and early and late outcomes. Although most outcome studies have correlated outcome with only one index of brain injury severity (65,66), McDonald and colleagues (60) compared 10 measures. In their report, the number of days to reach age-adjusted 75% performance on the COAT, the number of days to GCS 15, and the initial GCS scores were most predictive of outcome across all neurobehavioral and functional measures when measured early and at 1 year postinjury. The intercorrelations of these brain injury indexes were also quite high. In general, these indexes could be used interchangeably and a single measure of severity predicted most outcomes almost as well as multiple measures. Severity ratings as determined by these alternative criteria are summarized in Table 17.1. In summary, it is important to use these tools and correlate them with clinical findings to make an assessment of the severity of injury and therefore possible long-term outcome. Although useful, these assessment tools do have limitations in determining outcome, and a clinician’s clinical impression is also important. COMMON MOTOR DEFICITS A wide spectrum of motor deficits is seen after TBI. This spectrum results from the variable nature of the injury and the combination of focal and diffuse damage. TABLE 17.1 RATING OF BRAIN INJURY SEVERITY Isolated focal brain injuries can occur from a variety of causes, including brain tumor resections, gunshot wounds, and other foreign-body penetrations. The cognitive and motor deficits may vary because of differences in brain injury loci. Obviously, if there is a unilateral penetrating or focal injury involving the motor area, a hemiparesis may result. Depending on the precise location of the damage, hemiparesis may be more pronounced in the upper or lower extremity. The long-term outcomes in motor, cognitive, and behavioral functioning may be better in focal injuries versus diffuse injuries given the isolated nature of the brain damage (67). DIFFUSE DAMAGE The diffuse nature of TBI has resulted in a constellation of motor impairments that is familiar to clinicians who work with these problems. These include difficulties with balance, coordination, and speed of response. Despite these impairments, however, a significant number of children achieve functional mobility. In a study by Boyer and Edwards (68), at 1 year after injury, 46% of the patients walked independently without assistive devices and 27% walked with an orthosis or an assistive device. Overall, 79% had independent mobility. Swaine and Sullivan (69) have examined early motor recovery after TBI in 16 adolescents and adults who had a GCS score of 8 or lower for at least 6 hours. Assessments included evaluation of muscle tone, range of motion, abnormal and voluntary movement, primitive reflexes, equilibrium and protective responses, and specific motor skills. There were differential patterns of recovery and differential rates of recovery among the subjects, which is to be expected considering the heterogeneous nature of TBI. Chaplin and colleagues (70) evaluated motor performance in children after TBI. Fourteen children with TBI who were unconscious for 24 hours or longer were compared with 14 age- and sex-matched children. The Bruininks–Oseretsky Test of Motor Proficiency was administered at least 16 months after injury. Children with TBI scored significantly poorer on the Gross Motor Composite, including all subsets: running speed, balance, bilateral coordination, and strength. Also, they scored lower on the fine motor subsets for upper limb speed and dexterity. Most of these subtests involve timed tasks. Chaplin and colleagues also found a correlation between the Gross Motor Composite score and the time since injury. They concluded that this correlation supports continuing long-term improvement in skills after TBI. Kuhtz-Buschbeck and colleagues (71) looked at gait, gross motor proficiency, and hand function in 23 children after a TBI, severe in 17 and moderate in 6, during their 5 months of inpatient stay. They were compared with age- and sex-matched healthy controls. Children with TBI showed marked reduction in gait velocity, stride length, cadence, and balance. Deficits in fine motor skills, speed, and coordination were noted on hand function tests. Hand function skills improved less than gait; degree of impairment was noted to increase with severity of injury. Younger age at injury was not associated with better recovery. It has also been noted that the absence of spasticity is a good predictor of ambulation recovery by discharge (72,73). Others have also noted impaired fine motor skills after TBI. Again, the speed component of the assessment on these tasks may account for some of the impairments that were observed. Long-term impairment of finger tapping has been described (74). Practice of activities requiring fine motor coordination improves skills, even long after injury (75). BALANCE Balance is frequently found to be abnormal after TBI, as it involves effective integration of the sensory, motor-programming, and musculoskeletal system (76). Cochlear and vestibular function may be impaired. True vertigo may be present. The clinical exam could be normal, despite children being symptomatic (76). Blocking visual input during quiet standing is a simple and sensitive test for postural instability (77). Gait analysis and vestibular testing may be necessary to evaluate subtle changes leading to imbalance (76). When postural instability is assessed quantitatively, long-term impairment of static and dynamic control of posture is often found after TBI (78,79). It may be related to latency of response and asymmetric stance (80). Treatment options include oral medications, visual therapy, vestibular balance rehabilitation therapy (VBRT), and surgery (81). Oral medications, including meclizine and scopolamine, should be used sparingly, as they could slow the natural compensatory process (81). Specific training with VBRT exercises that promote habituation and/or adaptation and/or substitution can be used (81). TREMOR Another motor impairment that is seen is tremor, which frequently is more pronounced proximally and increases with effort and movement. Lesions have been noted in varying areas. Treatment with medications typically used for tremor may be of benefit (82,83). Andrew and colleagues (84) report stereotactic surgery to be effective in management of tremors. Muscle tone abnormalities, including spasticity, dystonia, and rigidity, are common after TBI. The types of problems noted vary, depending on the time since injury as well as the severity of injury. The cause of acquired brain injury also influences the type of problem that is most commonly noted. Spasticity has been noted in 38% and combined spasticity and ataxia in 39% of children and adolescents 1 year after injury (66). Rigidity or dystonia is especially common when there has been secondary injury due to hypoxia or ischemia (85). SPASTICITY Spasticity results from an upper motor neuron injury and is manifested by increased deep tendon reflexes and velocity-dependent resistance to movement (86,87). Several different scales are available to evaluate spasticity, but they are all subjective (81), and available quantitative tests are time-consuming (88). Physical Management It is important to begin treating spasticity in the acute care setting to prevent contracture development (89). Treatment approaches include range of motion, stretching, casting and splinting, medications, and surgical interventions used alone or in combination to manage spasticity. Range of motion itself may be helpful to reduce tone temporarily (90). Also, one may begin with positioning options, including but not limited to, splinting and weight-bearing, if tolerated, as well as the use of neutral warmth, gentle shaking, and reflex inhibition (91). If a child has a tendency to assume a total extension posture, positioning in side-lying with hips flexed beyond 90 degrees and neck flexion may assist in interrupting the extension pattern. If active posturing is present, one must be careful in the use of splints and casts because constant pressure against the splint or cast may result in the development of an ischemic ulcer (91). Stretching should always be included in any treatment protocol for spasticity (81). Pharmacologic Management Medications for treatment of spasticity can be oral, intrathecal, or injectable. Enterally administered pharmacologic agents may be beneficial in decreasing abnormal muscle tone and posturing. Their potential side effects may limit their effectiveness in this population. This is especially true of the sedating effects of baclofen and benzodiazepines. Dantrolene sodium causes sedation, despite its action at the sarcolemma. Alpha-adrenergic agonists, such as clonidine and tizanidine, have also been reported to decrease tone (81). The effectiveness of all of these medications is variable. Early after injury, when posturing may be a problem, chlorpromazine has been of assistance. It has significant potential to cause sedation (86). Bromocriptine has also been effective in reducing posturing early postinjury. Injectable medications include botulinum toxin and phenol motor point blocks. They can be used in combination with positioning, splinting, and casting. Early after injury, with severe posturing and intolerance of splinting, botulinum toxin may be a helpful adjunct in attempting to maintain range of motion. It is reversible, so if there is significant motor recovery, there is no permanent effect of the injection. Functional gains have been noted with the use of botulinum toxin (92–95). Phenol blocks tend to be used later after injury when there is residual difficulty with increased tone. Phenol and botulinum toxin injections can be used concurrently to treat severe spasticity and to increase the number of muscles treated at one time. If severe deformity develops, surgical tendon or muscle lengthening may need to be considered (85). Intrathecal baclofen (ITB) infusion using a programmable pump has been shown to be effective in the treatment of spasticity of cerebral origin, particularly cerebral palsy (96,97). Studies have also shown functional improvement in gait (94–96) with the use of ITB infusion in patients with acquired brain injury. Francisco (98) and colleagues also noted improvement in activities of daily living (ADLs) and decrease in pain. Two studies have shown caregiver and patient satisfaction in individuals treated with continuous infusion of ITB by an implanted programmable pump (99,100). ITB by an implanted programmable pump should be considered if severe systemic spasticity persists (101,102). Doses can be changed, depending on the patient’s progress. DYSTONIA Dystonia is defined as a disorder in which involuntary sustained or intermittent muscle contractions cause twitching and repetitive movements, abnormal postures, or both (87). It has been reported as a rare motor impairment and is more commonly seen in those injured as children rather than as adults (103,104). The interval between injury and onset of dystonia varies. No consistent picture is seen on neuroimaging study. Medications such as trihexiphenidyl hydrochloride, carbidopa/levodopa, and bromocriptine are used in treating dystonia. ITB infusion has also been used effectively to treat dystonia (102,105). RIGIDITY Rigidity is the resistance to an externally imposed joint movement, with an immediate resistance to reversal of the direction of the movement, and the limb therefore does not tend to return to a particularly fixed posture (87). Management of rigidity is similar to the management of spasticity and dystonia; however, it is often more refractory to intervention. COMMON SENSORY DEFICITS OLFACTORY DYSFUNCTION (ANOSMIA) Olfactory dysfunction is a common consequence of TBI, most frequently associated with severe injury, and has also been seen with PTA of more than 5 minutes (106). Bakker and colleagues (107) report an association between severity of anosmia and executive function in children. The incidence of anosmia varies from 5% to 65%, depending on the type and severity of the brain injury (108). Olfactory dysfunction can be a partial loss of the sense of smell (microsomia) or a complete loss of sense of smell (anosmia) (109). In a study carried out by Yousem and colleagues (110) to locate and quantify the deficits using radiographic studies, most patients with impaired olfaction showed damage to the olfactory bulbs and tracts, followed by the inferior frontal lobes and volume loss in the olfactory bulbs and tracts. Both patients and their parents are seldom aware of their deficits (111) and therefore formal testing should be done in children with TBI. The three-screen test can be used for quick, gross identification, but the University of Pennsylvania Smell Identification Test (UPSIT) is more reliable in identifying all patients with deficits (112). There is usually poor recovery from anosmia in comparison to parosmia (108). Impairment in the sense of smell may have social and safety implications (109). Those with anosmia must be cautioned to use other senses to look for dangers, such as a gas burner left on, fire hazard, or similar problems. Teenagers and young adults may need to be advised about the use of fragrance when they cannot receive any feedback about its strength. HEARING IMPAIRMENT Hearing impairments and impairments of vestibular function are also commonly noted. Hearing impairment may occur secondary to several causes: central processing deficit, peripheral nerve damage, cochlear injury, or disruption of the middle ear structures. Cognitive impairments that are common after TBI often interfere with the child recognizing this difficulty. It is important for clinicians to have a high index of suspicion in children and initiate screening for hearing impairment. Vestibular impairments have already been mentioned in the discussion on balance. Vertigo secondary to vestibular impairment commonly resolves within 6 months of injury (113,114), but electronystagmogram abnormalities can persist for years (115). Central auditory processing impairment occurs with damage to tracts or cortical tissue. In such individuals, pure tone audiometry is normal, but other studies, such as speech discrimination, or late waveforms of brainstem auditory evoked potentials are abnormal (116). Central auditory impairment is difficult for most families to understand. Their intuitive conclusion is that hearing is related to the ear, so they frequently anticipate that interventions such as a hearing aid may be helpful. Hearing loss may be conductive in nature because of disruption of the ossicles or CSF or blood in the middle ear. Both of these types of injuries are frequently associated with fractures of the temporal bone (117). Conductive hearing loss usually recovers spontaneously in about 3 weeks. If it persists for more than 3 weeks (particularly for >30 db), a repeat audiogram and exploration of the middle ear are recommended (118). Problems related to fluid in the middle ear usually resolve spontaneously. Sensorineural hearing loss may also be seen, but less often than conductive hearing loss (117,118). Sensorineural hearing loss is commonly noted at higher frequencies (117) and is associated with inner ear pathology (113,118). Marked variation is seen in the recovery of sensorineural hearing loss (118). There may be trauma to the eighth cranial nerve, or injury to the labyrinthine capsule, or labyrinthine concussion, which may result in hearing loss because of the transmission of high-energy vibrations and a pattern similar to the hearing loss after prolonged noise exposure (119). Injuries to the labyrinthine capsule and the eighth cranial nerve are frequently associated with basilar skull fracture. VISUAL IMPAIRMENT Because of the complexity of the visual system, a variety of visual impairments can be seen. Impairments may result from injury to cranial nerves, eyes, optic chiasm, tracts, radiations, or cortical structures (120,121). Early after injury, a child may appear to be functionally blind. Although vision is often assessed by looking at response to visual threat and visual tracking, these responses do not differentiate between peripheral and central impairments. One must assess cranial nerve function to make that differentiation. Visual acuity reduction is the most frequently detected deficit in children, but the severity varies and is associated with the severity of injury (121). Visual acuity reduction is commonly associated with frontal lobe injuries (120,121). In children with greater visual acuity impairment, optic nerve atrophy, either complete or partial, is present (121). Usually, optic atrophy is seen within 1 month after injury (120), and is correlated with the site of impact and not necessarily with the overall severity of the brain injury. Chiasmatic injury results in bitemporal visual field impairment of varying degree and is found in 0.3% of TBI cases. It may be identified on MRI (122). Homonymous hemianopsia is seen with injuries to the optic tracts and is often associated with hemorrhage and hemiparesis. Prism lenses may be of assistance, as well as learning compensatory techniques to increase scanning of the full environment (123). The presence of visual field impairments may be associated with more severe neuropsychological impairments (124). Central visual dysfunction may be described as visual processing or visual-perceptual problems. Cortical injury is responsible for this type of impairment and may not be confined to the occipital lobes. For example, involvement of temporal lobes may produce visual memory impairment, and involvement of parietal lobes may produce impairment of spatial awareness (125). Injury of the third, fourth, and sixth cranial nerves may lead to a variety of visual problems (126). Diplopia may result from extraocular muscle imbalance most commonly due to trochlear palsy (126) and may be present at all times or just in particular gazes. Patching is commonly used to eliminate diplopia but results in monocular vision and related disadvantages (127). In children under 11 years old, it is important to patch eyes in an alternating manner to avoid difficulty with amblyopia. Visual motor impairments due to unilateral abducens nerve palsy in children usually resolve spontaneously within 6 months (128). Deficits that persist longer than 6 months are more likely to be associated with bilateral or complete abducens nerve palsy and are unlikely to resolve spontaneously (128). Difficulties with convergence may also result in diplopia, and are believed to be due to supranuclear impairment. Anatomic correlates of diplopia have not been well described (126). Accommodation may also be impaired (129). COMMON COGNITIVE DEFICITS Although TBI can result in both motor and cognitive impairments, it is generally the cognitive impairments that most profoundly affect the individual’s ability to function. As noted previously, the full extent of the child’s cognitive impairment may not be known until a significant time after injury, as deficits may not become apparent until the child is at a developmental stage when one would anticipate that he or she would have a particular cognitive ability, such as abstract thinking or metacognition. In general, when children have been followed long term after injury, those who were injured at a young age typically show more cognitive impairment than those injured later in childhood (130). ATTENTION AND AROUSAL Arousal is a precursor for attention. It has been defined as “the general state of readiness of an individual to process sensory information and/or organize a response” (131). Although there have not been systematic studies of pharmacologic interventions to improve arousal in children with TBI, a number of medications have been used and reported in case studies. One retrospective report of amantadine in children with TBI noted that compared to a group of children who had not been started on any neurostimulant medication, those on amantadine had a greater increase in their Rancho Los Amigos level during hospitalization. The amantadine group had lower initial Rancho scores and GCS (132). Dopaminergic medication use has also been reported, again in a retrospective review. In this report, the children’s Western Neuro Sensory Stimulation Profile scores prior to and during medication were compared. Also, the rates of change in these scores before and after medication were compared. Significant differences were noted, suggesting that the medication could be contributing to the accelerated rate of improvement (133). As noted previously, children with a prior history of ADHD are at an increased risk to sustain TBI. Likewise, attentional problems are common after TBI, affecting an additional approximately 20% (6). The severity of TBI is reported to be associated with the likelihood of developing attentional problems (134,135). The attentional problems seen after TBI in children are not the same as seen in developmental ADHD. It has been reported that skills that develop earlier in childhood are relatively spared compared to those that develop later. Therefore, sustained attention and divided attention are more significantly impaired than focused attention (136). Also, children with TBI tend to have slower response speeds than children with developmental ADHD (137). Both behavioral interventions and medications have been used as treatment for children with attentional problems after TBI. Case reports have noted improvements (138,139). MEMORY IMPAIRMENT Memory impairment is another common area of concern after pediatric TBI. Typically, the memory impairment that is seen is for the formation of new memories as opposed to long-term memory. This has significant implications for a child’s ability to learn new information. As observed in other areas, severity of memory impairment appears to be related to the overall severity of injury. Impairment is seen in both immediate and delayed recall in severe TBI (140–143). When evaluating preschool children who had experienced TBI, Anderson and colleagues (141) found that over time, children did show developmental progress in their memory skills; however, children with more severe TBI did less well over time. They saw this trend as well for both the learning and memory measures that they evaluated. It has been reported that verbal memory is more impaired than visual memory after TBI in children and that unstructured retrieval is the most impaired aspect of memory (144). Memory impairment is a challenging deficit to attempt to address during rehabilitation. Different approaches include trying to improve recall through memory practice, using organizational strategies or mnemonics, using teaching techniques to make learning more efficient (including backward chaining), and making use of compensatory techniques such as a memory notebook or electronic device (143,145,146). Avoiding purely verbal teaching, making use of structured activities in teaching, and increased repetition have been advocated as well (144). BEHAVIORAL PROBLEMS Behavioral sequelae are also common after TBI in children. These can include impulsivity, personality changes, depression, anxiety, becoming easily frustrated, aggression, and sleep problems (147). These problems persist long term and are reported in 10% to 50% of children with TBI (148,149). Some authors report an increase of emotional and behavioral symptoms over time (149). Also, a number of authors note that those who sustain TBI are more likely to have a preinjury history of behavioral or psychiatric concerns (148,150). Behavioral problems can be significantly disabling even in the absence of significant mobility or ADL impairment (148). Behavioral problems appear to be more significant and more common in those injured at a younger age (150). Approaches to address behavioral concerns include providing structured environments and daily routines but allowing the individual to make choices when possible, as well as assisting in breaking down tasks to their component parts, providing cues or aids for organization, creating situations in which the individual will be successful, and helping the individual to communicate the need to escape a task or situation. Positive reinforcement of desired behaviors has also been used. Involvement of family members in the process is important (150,151). Various medication interventions have been tried in the past, but none has been shown to be ultimately superior to others in addressing this variety of behavioral symptoms. It is imperative that those working with the individual understand that the behavioral problems are neurologically based. Behavioral symptoms are strong predictors of family burden over time (149). COMMUNICATION DEFICITS A variety of communication impairments can be seen after TBI in children. If there is focal injury in areas of the brain that control language, aphasia can be seen. Also, motoric impairment can contribute to dysarthria. In general, the communication impairments that are seen more commonly are due to other cognitive deficits, such as memory impairment and executive function concerns (150). Difficulties with response speed can contribute to a reduced rate of speech and, conversely, impulse control difficulties can result in a rapid rate of speech (152). Word finding and verbal learning deficits are common, potentially relating to memory impairment (150,153). Discourse, abstract language, and social interaction with language are all commonly impaired (150,154). Also, verbal working memory, which is commonly impaired, is important in acquiring language, reading, and arithmetic in children (155). Authors report that the ability to use language functionally is typically more impaired than one would expect from reported results of standardized intelligence testing (156). EXECUTIVE FUNCTION The area of executive function is one that is commonly affected, even in children who have experienced a mild TBI. It also is one in which the full effect of the injury may not be manifest until the child has matured to the point when one would expect him or her to demonstrate these particular skills. Executive function is defined as the ability to manage and direct more modular cognitive abilities in order to set, manage, and attain goals (6). This includes problem solving, organization, self-monitoring and self-regulation, self-appraisal, and self-management. It has been suggested that children are particularly susceptible to impairment in executive function if injured, as they are experiencing rapid development in this area (6). Impairments of executive function are noted to be more severe in children injured at a young age (157). Working memory is one of the first executive function areas to develop, emerging between 7 and 12 months of age. It involves being able to temporarily store some information while concurrently processing and retrieving other data (158). It has been shown to be impaired after TBI, and the degree of impairment relates to the severity of injury (6,155,158). Other areas commonly affected by TBI include the ability to inhibit, shifting set, planning, self-monitoring and control, decision making, social cognition, and behavioral self-regulation. The Behavior Rating Inventory of Executive Function (BRIEF) is a tool that uses parent and teacher ratings to evaluate the impact of executive dysfunction on everyday life (6). Interventions for executive dysfunction have not been rigorously studied. Some have suggested using an approach that breaks tasks into problem-solving steps. Also, the provision of a structured environment and expectations is important. Incentives for progress toward a goal can be helpful. It is imperative that parents develop an effective working relationship with their child’s school program providers to have open communication around the issues of executive dysfunction and its impact on school programming (6,157,159). It is not possible to totally separate social functioning from executive function; however, a separate comment on this important area will be undertaken here. A child’s ability to effectively function within his or her social milieu is often significantly affected by TBI. Emotional lability is common (160). Often, children have difficulty interpreting social cues from others or recognizing the emotions being expressed (161,162). Janusz and colleagues (160) reported on social problem-solving skills in children with TBI. They found that although the children were able to articulate the social dilemmas, they chose less developmentally mature strategies as the best means to solve them and also used low-level reasoning to evaluate whether the strategies were effective. Social participation is also reported to be decreased in children with TBI compared to their typically developing peers. Bedell and Dumas (163) reported that 30% to 73% of the children with acquired brain injuries that they studied were restricted in at least one of the participation domains they evaluated. Family-reported institutional, social, and attitudinal barriers were more often contributing to this restriction than physical environmental barriers (163). One recent study reported that two-thirds of children and adolescents with TBI continued to experience difficulty in a variety of social settings at 2 years after injury. These challenges were associated with their behavioral symptoms (164). MEDICAL CONDITIONS ASSOCIATED WITH TBI Medical conditions associated with TBI can vary greatly from individual to individual. Essentially, all organ systems can be affected when a child sustains a TBI. NEUROENDOCRINE DYSFUNCTION Head trauma places the pituitary gland at risk for injury due to its encasement in the sella turcica, its delicate infundibular structures, and its tenuous vascular supply. The gland may be subject to edema, ischemia, transection of the pituitary stalk, or watershed injury (165). Dysfunction of the hypothalamic–pituitary axis can be categorized as either involving the anterior or the posterior pituitary. Posterior pituitary dysfunction results in syndromes including diabetes insipidus (DI) and the syndrome of inappropriate antidiuretic hormone (SIADH) secretion. DI is commonly noted early after a moderate or severe TBI and can, therefore, be considered a potential marker for global hypothalamo-pituitary injury and dysfunction (166). SIADH also is a result of posterior pituitary dysfunction and needs to be distinguished from DI. The incidence of DI in children is poorly understood and poorly researched. One study (167) demonstrated incidence around 21.6% of DI in adults with moderate or severe brain injury. The study also found DI tended to be associated with a lower GCS and with the presence of cerebral edema. The fluid and sodium imbalance of DI results in a deficiency of antidiuretic hormone and excessive water loss. As antidiuretic hormone is produced in the hypothalamus, those patients who exhibit DI are felt to be predisposed to other hypothalamo-pituitary system dysfunctions. Patients with DI are hypernatremic and demonstrate polyuria and polydipsia. Although often DI is only a temporary problem for most people with TBI, it may persist. Treatment for DI is desmopressin acetate (DDAVP), which is a synthetic form of an antidiuretic hormone (168). SIADH is another common fluid and electrolyte imbalance encountered in those with TBI, and needs to be distinguished from DI in order to provide appropriate treatment. In contrast to DI, these individuals exhibit decreased urine output, hyponatremia, and decreased serum osmolarity. SIADH is typically managed with fluid restriction and carefully reestablishing the serum sodium to a normal level in a cautious fashion. Rapid correction of the hyponatremia can cause pontine myelinolysis and possibly death (168). CEREBRAL SALT WASTING Cerebral salt wasting is the third cause of serum sodium imbalance in individuals with TBI. Like SIADH, cerebral salt wasting results in hyponatremia. It is essential that cerebral salt wasting be distinguished from SIADH. Unlike DI and SIADH, cerebral salt wasting does not involve the hypothalamo-pituitary system, but is believed to occur due to direct neural effects on renal tubular function. The low sodium levels seen are a direct result of abnormal renal tubular function, resulting in lost sodium along with lost fluid volume. These patients are dehydrated and, therefore, fluid restriction would cause their condition to further decline. The treatment for cerebral salt wasting involves fluid and sodium replacement (169). ANTERIOR PITUITARY DYSFUNCTION Literature suggests that approximately one-third to one-half of adults who have sustained a moderate or severe TBI have some hypothalamo-pituitary dysfunction (166). Children with TBI are at risk for hypothalamo-hypophyseal dysfunction, with one study identifying a rate of about 60% (170). Another group of 48 pediatric patients were found to have a 10% incidence of hypothalamo-hypophyseal dysfunction 6 months after their brain injuries (171). The challenge in identifying which children to screen for anterior pituitary dysfunction is that many of the symptoms of anterior pituitary dysfunction mimic the effects of TBI. For instance, low levels of growth hormone are associated with symptoms such as fatigue, cognitive dysfunction, irritability, and DI (166). An individual who has sustained a TBI would commonly complain of these symptoms and have them dismissed as sequelae of the brain injury. In 2005, a consensus statement on screening for hypopituitarism after TBI recommended systematic screening for pituitary dysfunction for individuals with moderate to severe TBI who are at risk of developing pituitary dysfunction. They recommend screening for hypopituitarism if, while patients were hospitalized, they had DI or hyponatremia and hypotension. If they had SIADH or hypothyroidism identified, screening for anterior pituitary dysfunction would also be indicated. Reasons noted for foregoing anterior pituitary function screening include the individual being in a persistent vegetative state at a very low level of consciousness. Since little is known about the incidence of hypothalamo-pituitary dysfunction in children after TBI, the majority of the recommendations are extrapolated from adult literature. The treating physician should be knowledgeable, however, of the presenting features of hypothalamo-pituitary dysfunction in children, which may include growth failure, arrested or delayed puberty, amenorrhea, decreased libido, and short stature (172). PRECOCIOUS PUBERTY Precocious puberty is defined as the onset of puberty in girls before the age of 8 years and in boys before the age of 10 years. It can occur following TBI in children, with signs developing from 2 to 17 months after the initial injury. There is a positive correlation between increased ventricular size secondary to cerebral atrophy and the development of precocious puberty, and girls are affected much more frequently than boys (54.5% in girls to 4.5% in boys) (173). The signs of precocious puberty include onset of secondary sexual development prior to the predicted age and accelerated linear growth. These children demonstrate advanced bone age and premature closure of the epiphyseal plates. Because precocious puberty places a social and emotional burden on the patient and family, and because of the development of short stature secondary to premature epiphyseal plate closure, it is essential that the physician have a watchful eye for precocious puberty and be prepared to evaluate for it and treat it if indicated. RESPIRATORY DYSFUNCTION Recommendations for the treatment of children with TBI include transitioning from endotracheal intubation to tracheostomy for ventilatory support around the time the patient is 7 to 10 days postinjury. The tracheostomy allows for pulmonary support, easier secretion clearance, and better long-term airway management. The tracheostomy is not without complications, though, including, the potential for vocal cord paralysis, tracheal stenosis, subglottic and glottic stenosis, and tracheomalacia (174). The ultimate goal is to move toward decannulation once controlled ventilation is no longer needed and when the patient is able to manage his own secretions. Another reason to move toward decannulation is to avoid the increased nursing and respiratory care requirements when the tracheostomy tube is in place. These increased needs can complicate discharge, as some long-term care facilities are unwilling to provide care for patients with tracheostomies and family members may be anxious and apprehensive about caring for a child who has one (175). The stepwise fashion moving toward decannulation has been described by Klingbeil (176). The process begins with downsizing the tracheostomy tube sequentially until, ultimately, an uncuffed small tube is tolerated. Then capping of the tracheostomy tube is recommended as the clinician evaluates the patient’s tolerance. If the patient is able to maintain oxygen saturations with a comfortable breathing effort and demonstrate effective cough with good management of secretions, the tube is removed and an occlusive dressing is placed to allow the site to heal. If the patient is demonstrating difficulty during the process of decannulation with worsening respiratory function or distress, it is recommended that the patient undergo direct laryngoscopy prior to decannulation in order to evaluate for concerns such as tracheal granuloma. NUTRITIONAL MANAGEMENT Very early after severe TBI, it is important for the primary team to place emphasis on the child’s nutritional status. Guidelines have been established for achieving adequate nutritional management in this population (177). These guidelines are mostly from the adult TBI literature, as there is quite limited pediatric research regarding nutrition after TBI. Metabolism is reported to be increased after severe TBI in children, causing increased nutritional requirement. Phillips and colleagues (178) studied pediatric TBI survivors who had initial GCS between 3 and 8. Overall, the energy expenditure in those patients was 130% of their expected metabolism. Phillips also found that weight loss ranged between 2 and 26 pounds during their 2-week postinjury evaluation despite aggressive nutritional support. Moore and colleagues (179) identified metabolic profiles of pediatric TBI survivors who had initial GCS of less than 7. They found that the increased energy expenditure in that group averaged 180%. In adult literature, hypermetabolism in TBI survivors is well established. The guidelines for the adult population include the following recommendations: (a) full nutritional replacement should be initiated by day 7 postinjury; (b) enteral nutrition should be started no later than 72 hours postinjury; and (c) tight control of serum glucose is necessary to avoid hyperglycemia, which is associated with worsening ischemic injury and worse outcome. Parenteral nutrition should be started if enteral nutrition is not full and complete by day 7. TUBE FEEDINGS Typically, enteral support of nutrition begins with nasal jejunal or nasal gastric feedings. Jejunal tube feedings are often tolerated better due to delayed gastric emptying (174), but the goal is to move to gastric feeds with boluses of nutritional formula for more typical meal feedings to decrease the complexity of equipment needs and to more approximate the typical physiology of enteral feedings. Percutaneous gastronomy (PEG) tubes are often placed at the time tracheostomies are placed, with the presumption that the patient who requires the tracheostomy will require tube feedings for longer than an acceptable time to leave a nasal tube in place. Nasal gastric and nasal jejunal tubes are associated with an increased risk of sinusitis, and the presence of the tubes in the posterior pharynx may be a source of irritation for the restless and the agitated child with TBI. If the child’s cognitive status improves and he or she achieves full nutrition by mouth with no risk for aspiration, the PEG tube can be discontinued as early as 2 to 6 weeks after it was placed once the cutaneous-gastric fistula has matured (180). Janik and colleagues (181) found that gastrostomy tubes that remained in place in the pediatric patient for greater than 8 months required surgical closure of the fistula in 92% of the patients studied. GASTROESOPHAGEAL REFLUX DISEASE Prior to placing a gastrostomy tube, consideration should be given to the child’s likelihood of having gastroesophageal reflux disease. This can be evaluated with an upper gastrointestinal radiological study, a pH probe study, or a milk scan. Occasionally, a Nissen fundoplication will be done in conjunction with the placement of a gastrostomy tube to avoid reflux and the risk for aspiration and its associated morbidity. Children with gastrostomy tubes in place should usually be placed on an H2 receptor blocker or proton pump inhibitor to decrease risk for acid reflux as well as gastrointestinal bleeding (182). TRANSITION TO ORAL FEEDINGS Evaluation of the child with TBI at the bedside by speech and language pathologists and/or occupational therapists is usually the first step in determining whether to begin transitioning to oral feeding. Studies show that dysphagia, oral motor impairment, and cognitive impairment are all highly correlated in the child with TBI; therefore, evaluation at the bedside of oral motor control as well as cognitive impairment helps to determine the degree to which dysphagia is present (183). The incidence of dysphagia in this population varies with the severity of the brain injury. The overall incidence is reported to be 5.3%. Children with mild brain injuries have an incidence of dysphagia of 1%, moderate brain injuries demonstrate a 15% incidence, and severe brain injuries 68% (184). The strongest factor predicting whether dysphagia will be present in a pediatric patient is the GCS. If the GCS is less than 9 (representing a severe TBI), the child is more likely to have dysphagia. These children tend to exhibit both oral and pharyngeal deficits with reduced lingual control and a delayed swallow reflex in the majority (183). Most dysphagia in this population resolves about 12 weeks postinjury and a normal diet is resumed. Once a child is evaluated by modified barium swallow and no silent aspiration is identified, the rehabilitation team can begin oral feeding in a stepwise fashion. Typically, the team will begin with tastes of pureed foods and thickened liquids, with progression over time, as tolerated, to solid foods and thin liquids. BOWEL MANAGEMENT It is important to maintain regular bowl movements early on in the critical care course of a child with a TBI. A bowel management program may involve stool softeners, suppositories, and/or laxatives in order to cause regular and routine bowel movements. The patient’s bowel management program needs to be adjusted depending on his or her clinical response. Narcotic medications are constipating and antibiotic medications can cause loose stools, so close follow-up and regular adjustments are indicated. Once the child is medically stable and the routine for their bowel routine is better established, the team may choose to cause bowel movements at the same time of day with the use of a suppository. In this way, “functional continence” may be obtained, with the child’s bowel movements being more predictable. The agents commonly used include senna, docusate sodium, polyethylene glycol, or glycerin suppositories. BLADDER MANAGEMENT During acute care of the child with severe TBI, it is common for a Foley catheter to be in place for measuring urine output. After children have been transferred from the critical care unit to the rehabilitation unit, they typically are placed in diapers for management of their incontinence. In children with cognitive impairment, the majority of their incontinence is a result of a disinhibited bladder. In these children, the bladder is emptied completely and bladder volume is reduced. If their cognitive status allows, they may be able to participate in a timed voiding program to achieve functional continence or to learn continence. Children may also have a neurogenictype bladder with uninhibited bladder contractions, which can be treated with anticholinergic medication. This will allow for increasing bladder volume. If the clinician is faced with bladder emptying that resembles an upper motor neuron or lower motor neuron voiding pattern, it is imperative that spinal cord injury be ruled out. This possibility can usually be eliminated by demonstrating low postvoid residual volumes (185). CENTRAL AUTONOMIC DYSFUNCTION Central autonomic dysfunction (CAD) is a clinical entity that is manifest by a myriad of symptoms, including hyperthermia, hypertension, diaphoresis, generalized rigidity, tachypnea, decerebrate posturing, tachycardia, and pupillary changes. It has many names, including, diencephalic seizures (186), autonomic storming, autonomic dysfunction syndrome (187), hypothalamic midbrain dysregulation syndrome (188), central seizures, central storming, central fevers (189), and posttraumatic hyperthermia (190). CAD is a result of an injury to the brain that interrupts the diencephalic–brainstem connection, leading to what is called “brainstem release phenomenon (188).” Signs and symptoms will often disappear as neurologic improvement is noted, but medical management may be necessary for 6 months or more after injury in a select group of patients (191). Management of CAD is usually initiated due to concern about an elevated body temperature. It is imperative the clinician rule out an infectious etiology, as central temperature elevation is a diagnosis of exclusion. CAD responds poorly to antipyretic medication (187), such as nonsteroidal anti-inflammatory drugs. This may be helpful when ruling out infection. Initial management at the bedside usually consists of attempting to lower the temperature by providing cooling blankets and ice packs, turning down the temperature in the room, or providing a fan in the room to cool the patient. Often, the patient’s hypertension is marked enough to warrant treatment with a beta-blocker such as propranolol, which will also help reduce the heart rate and can be used on an as-needed basis (189). Bromocriptine is used by some clinicians to reduce the symptoms of CAD and has ultimately resulted in a decreased need for antipyretics (189). Morphine in combination with bromocriptine has been useful in one study. ITB has also been reported to effectively treat CAD associated with TBI (101,192). CAD is associated with a poor prognosis. In a retrospective review of a series of children with acquired brain injury, CAD correlated positively with more protracted periods of unconsciousness and overall worse cognitive and motor outcomes one or more years postinjury. Follow-up computed axial tomography (CAT) scans in these children revealed ventricular enlargement and marked brain atrophy (191). HETEROTOPIC OSSIFICATION Pediatric TBI survivors have about a 14% to 23% chance of developing heterotopic ossification (174). It is more common in children who are over 11 years of age and also more common in children who have two or more extremity fractures (193). Heterotopic ossification in children with TBI is most common at the hips and knees. Diagnosis is often made approximately 1 month after injury (193,194). Signs and symptoms of heterotopic ossification include pain, decreased range of motion, and occasionally swelling (194). Deep venous thrombosis may be present concomitantly with heterotopic ossification and warrants further evaluation (195). Treatment of heterotopic ossification begins with regular and aggressive passive range of motion for these patients. Occasionally, splinting is necessary to prevent worsening contracture. Nonsteroidal anti-inflammatory drugs such as indomethacin, ibuprofen, and aspirin are often employed in an effort to halt progression once it is identified (193,194). Although in adult rehabilitation patients heterotopic ossification is often treated with high-dose disodium etidronate, it is avoided in pediatric patients due to concerns for development of rickets or rachitic syndrome (196). Rarely does pediatric heterotopic ossification require surgery (174,193,194). POSTTRAUMATIC EPILEPSY In recent years, whether pediatric TBI survivors should be treated with AEDs prophylactically has been discussed frequently in the literature. Seizures after TBI are separated into immediate, early, and late posttraumatic seizures. Immediate seizures happen within the first 24 hours of injury, and early seizures happen within the first 7 days. Late seizures occur anytime after the first week following the brain injury and may begin many years after injury (197). In adults who have TBI, early seizures correlate with the development of late seizures. However, this correlation is not seen in the pediatric population after brain injury (198). The incidence of posttraumatic seizures is greater in children than in adults. Although the majority of posttraumatic seizures in children are immediate seizures, the incidence of early seizures ranges from 20% to 39% (57,198–200) and the incidence of late seizures ranges from 7% to 12% (198,201,202). It should also be noted that lower GCS and younger age are associated with a higher risk of early posttraumatic seizure (57,198–200,203). Children less than 2 years of age have a threefold greater risk of early posttraumatic seizures compared with children who are 2 to 12 years of age (200). In one study of children who were 3 years of age and younger at injury, the risk of late posttraumatic seizures was greatest for those under 1 year of age at the time of injury (58). The risk of epilepsy after TBI in children and young adults was studied based on a population study from Denmark (204). The relative risk of epilepsy was twice higher after mild brain injury and seven times higher after severe brain injury compared to no brain injury for all ages. Brain injury was associated with an increased risk of epilepsy in all age groups but was highest among those older than 15 at injury. Having a family history of epilepsy increased the risk of developing posttraumatic epilepsy. Consensus guidelines established in 2003 state that currently there is insufficient data to support a standard guideline for the prevention of pediatric posttraumatic seizures (177). The guidelines recommend that prophylactic AED not be used to prevent the development of late seizures. They did note, however, the bulk of the evidence does suggest considering AED as a treatment option to prevent early seizures in high-risk patients. The American Academy of Physical Medicine and Rehabilitation agrees that “[a]ntiepileptic drugs are not recommended after one week for seizure prophylaxis in nonpenetrating traumatic brain injuries.” Young and colleagues (202) conducted a randomized, double-blinded, placebo-controlled study to evaluate phenytoin in 41 children with TBI who were followed for 18 months postinjury for the development of seizures. No statistically significant difference was distinguished between the groups in the development of late posttraumatic seizures. Posttraumatic epilepsy is diagnosed when the patient has two or more seizures in the late period after TBI. For the child who transfers to the pediatric rehabilitation medicine unit on phenytoin or another AED, the process of weaning the medication is fairly simple. If serum levels of the AED are subtherapeutic, it is safe to discontinue the medication without weaning. Otherwise, the dose can be reduced by approximately 50% the first week and can be discontinued thereafter. Since early seizures in children are not correlated with the development of late seizures, one can obtain an EEG in children who had early seizures and if no epileptiform activity is identified, consideration can be given to weaning the AED (168). In children who develop posttraumatic epilepsy, AED therapy should use medications that have the least effect on cognitive function. This medication should then be used at the lowest clinically effective dose in order to maximize the cognitive recovery of these patients. The consulting pediatric neurologist considers which AED to use in a given child based on factors including the clinical seizure pattern, the EEG activity, and the side effect profile of the AED. POSTTRAUMATIC HYDROCEPHALUS AND CEREBRAL ATROPHY Ventriculomegaly is seen commonly after severe TBI in children (64). The enlargement of the ventricular system can be either from high-pressure hydrocephalus or from cerebral atrophy resulting in hydrocephalus ex vacuo. True hydrocephalus is a result of either an obstruction in the cerebral spinal fluid flow or impairment in the absorption of cerebral spinal fluid, ultimately resulting in an increase in cerebral spinal fluid volume and pressure. Hydrocephalus can be described, therefore, as either communicating (where there is abnormality in absorption) or noncommunicating (where there is an obstruction in the flow of the cerebral spinal fluid). The majority of hydrocephalus is caused by impaired cerebral spinal fluid absorption, secondary to inflammation or secondary to subarachnoid hemorrhage. Hydrocephalus ex vacuo describes enlargement of the ventricular system that results after cerebral atrophy and loss of brain volume (Figure 17.1). To distinguish between clinically significant hydrocephalus and the expected consequence of cerebral atrophy after severe TBI, one must consider the patient’s clinical status as well as the amount of time that has passed since the injury. Overall, if the patient is continuing to demonstrate ongoing and regular improvements in his or her clinical status, ventriculomegaly is more likely to be due to cerebral atrophy. The patient who has hydrocephalus typically continues with poor clinical improvement or clinical deterioration. The CT scan findings will yield clues as well, with cerebral atrophy demonstrating areas of encephalomalacia or enlargement of sulci, while hydrocephalus demonstrates more specific changes around the ventricular system outlined in Table 17.2 (205).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








