Transposition of the Great Arteries
William H. Neches
Sang C. Park
Jose A. Ettedgui
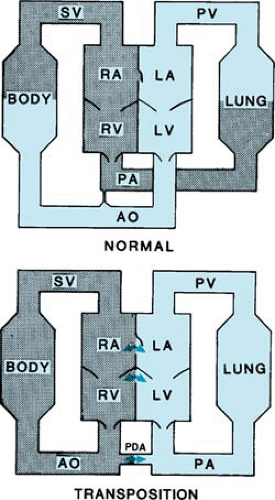
Transposition of the great arteries, or complete transposition, is a common form of cardiac abnormality found in approximately 5% of all patients with congenital heart disease. The distinguishing anatomic feature of transposition is the discordant ventriculoarterial connection of the great arteries whereby the aorta originates from the morphologic right ventricle and the pulmonary artery from the morphologic left ventricle. The consequence of this anatomic arrangement is that unoxygenated systemic venous blood returning to the heart passes through the right atrium and right ventricle and is ejected into the aorta. Similarly, oxygenated pulmonary venous blood reaches the left side of the heart and is returned to the pulmonary artery. The clinical situation that results from this cardiac anomaly is characterized by severe, life-threatening hypoxemia early in life. The presence or absence of associated cardiac abnormalities dictates the presentation, clinical course, and surgical approach to the management of the three main categories of patients with transposition:
Transposition with an intact interventricular septum (complete transposition). These patients may or may not have left ventricular outflow tract obstruction (subpulmonary stenosis).
Transposition with ventricular septal defect. This is complete transposition and an interventricular communication but without narrowing in the left ventricular outflow tract.
Complex transposition, which is complete transposition, ventricular septal defect, and varying degrees of left ventricular outflow tract obstruction. These patients usually have significant subpulmonic stenosis and equal right and left ventricular pressures. This category includes patients with pulmonary atresia.
Other major associated cardiac lesions include patent ductus arteriosus and coarctation of the aorta.
Before the modern era of cardiac catheterization and cardiac surgery, more than 90% of patients with transposition died in infancy. This lesion was one of the most common causes of death from congenital heart disease in the first year of life. In recent years, advancements in cardiac catheterization and cardiac surgery have transformed the devastating natural history of this anomaly so that today more than 90% of patients with this lesion are expected to survive into adulthood.
PHYSIOLOGY AND HEMODYNAMICS
In the normal heart, the circulation is connected in series. Systemic venous return passes into the pulmonary artery, while pulmonary venous return passes into systemic arterial circulation. In the heart with transposition of the great arteries, the result of the abnormal arterial connection is that the individual has two parallel circulations (Fig. 262.1). Systemic venous return passes through the right heart and is ejected into the aorta, whereas pulmonary venous return passes through the left heart and is again ejected into the pulmonary artery. This physiologic arrangement is incompatible with life unless blood can be mixed between the two circulations. In the neonate with transposition of the great arteries and an intact interventricular septum, a foramen ovale or atrial septal defect usually is present and facilitates exchange of blood at atrial level. A patent ductus arteriosus enhances this exchange. The ductus arteriosus is usually a transient neonatal structure, however, and tends to close physiologically within a few days after birth. Closure of the duct precipitates a dramatic change in the clinical appearance of an apparently healthy newborn to one with intense cyanosis.
The patient with transposition of the great arteries and a significantly sized ventricular septal defect presents an entirely different clinical picture. These patients often have adequate exchange of blood, with a combination of mixing at atrial and ventricular levels. As a result, only mild cyanosis is present in the early neonatal period, and, therefore, a significant cardiovascular anomaly often is not suspected until a few weeks later. As a result of this large ventricular septal defect, patients
present with congestive heart failure toward the end of the first month of life and are at risk for subsequent development of pulmonary vascular disease.
present with congestive heart failure toward the end of the first month of life and are at risk for subsequent development of pulmonary vascular disease.
The physiologic features in patients with complex transposition (transposition with ventricular septal defect and pulmonary stenosis) differ from those of either of the other two clinical forms. Patients with complex transposition have a large ventricular septal defect, and the balance between pulmonary and systemic blood flow depends on the degree of pulmonary stenosis. When severe pulmonary stenosis or pulmonary atresia is present, the patient presents with cyanosis and reduced pulmonary blood flow early in life. If pulmonary stenosis is less severe, then clinical presentation results from the presence of cyanosis or detection of a heart murmur and may occur even later in infancy.