Transitional Ankle Fractures: Juvenile Tillaux and Triplane Fractures
Jeanne M. Franzone
Joshua E. Hyman
The closure pattern of the distal tibial physis renders the distal tibia prone to unique fracture patterns during the adolescent growth phase. The distal tibial physis closes at approximately age 14 in girls and age 16 in boys. Physeal closure takes place gradually during the preceding 18 months in a specific order. The central region is the first area to close, then the anteromedial aspect, then the posteromedial aspect, and lastly the lateral aspect. Specifically, the anterolateral region of the physis is the last area to close. The combination of unfused areas of relative weakness being prone to fracture and the relative strength of the stabilizing ankle ligaments being greater than that of the physis sets the stage for transitional fractures of the distal tibia including juvenile Tillaux and triplane fractures. Such fractures do not fall neatly within the Dias-Tachdjian classification system.
The juvenile Tillaux fracture is a Salter-Harris III fracture of the anterolateral part of the distal tibial epiphysis. An external rotation force to a supinated foot causes avulsion of the anterolateral distal tibial epiphysis with anterolateral displacement due to the pull of the anteroinferior tibiofibular ligament. The juvenile Tillaux fracture was originally described by Kleiger and Mankin in 1964 with reference to the Tillaux fragment identified in the setting of lateral tibial avulsion fractures in cadavers by the French surgeon Paul Jules Tillaux in 1892. Juvenile Tillaux fractures constitute approximately 3% to 5% of pediatric ankle fractures.
Triplane fractures were initially described by Johnson in 1957 and by Marmor in 1970 and account for 5% to 15% of pediatric ankle fractures. They are also external rotation injuries, but they are constituted of multiple fracture lines. In the sagittal plane, there is a fracture line through the joint surface and the epiphysis (akin to the Salter-Harris III fracture of the juvenile Tillaux pattern); there is also an axial plane fracture through the distal tibial physis, and in the coronal plane, the fracture line exits through the metaphysis. Many variants have been described including two-part, three-part, and four-part triplane fractures. The two-part fracture pattern is the most common in which a large posterolateral epiphyseal and posterior metaphyseal fragment remains one fragment. In a three-part lateral triplane fracture, the smaller anterolateral epiphyseal fragment is fully detached, and in a four-part triplane fracture, the anterior epiphysis splits into two fragments (Fig. 12-1).
INDICATIONS FOR OPERATIVE MANAGEMENT
As with all traumatic evaluations, the history and physical exam of adolescents with ankle injuries are of paramount importance. Patients will typically describe a twisting force to the lower leg or foot during athletic or recreational activities. Some patients will present a few days after
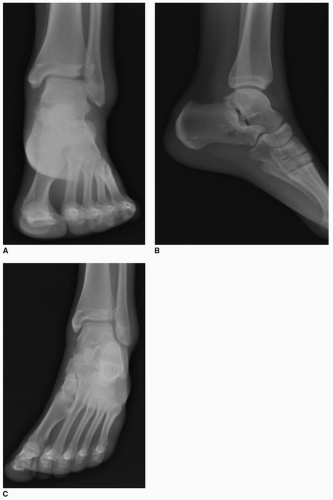
the injury initially underestimating the injury as an ankle sprain. Both severe ankle sprains and ankle fractures will present with pain, swelling, ecchymosis, and a reluctance to bear weight on the injured ankle. Examination of the skin integrity and swelling, as well as the presence of neurologic defects or vascular injuries, will help determine both the energy of the initial injury and its surgical acuity. It is important to fully palpate the lower extremity including the length of the fibula to evaluate for a Maisonneuve fracture of the proximal fibula as well as down through the foot to evaluate for injuries such as fractures of the base of the fifth metatarsal. A full radiographic evaluation will include tibia-fibula films and three views of the ankle—anteroposterior (AP), mortise, and lateral views. Particularly with juvenile Tillaux fractures, the tibiofibular overlap on a standard AP view can obscure a fracture of the lateral aspect of the distal tibial epiphysis (Fig. 12-2).
the injury initially underestimating the injury as an ankle sprain. Both severe ankle sprains and ankle fractures will present with pain, swelling, ecchymosis, and a reluctance to bear weight on the injured ankle. Examination of the skin integrity and swelling, as well as the presence of neurologic defects or vascular injuries, will help determine both the energy of the initial injury and its surgical acuity. It is important to fully palpate the lower extremity including the length of the fibula to evaluate for a Maisonneuve fracture of the proximal fibula as well as down through the foot to evaluate for injuries such as fractures of the base of the fifth metatarsal. A full radiographic evaluation will include tibia-fibula films and three views of the ankle—anteroposterior (AP), mortise, and lateral views. Particularly with juvenile Tillaux fractures, the tibiofibular overlap on a standard AP view can obscure a fracture of the lateral aspect of the distal tibial epiphysis (Fig. 12-2).
A computed tomography (CT) scan is important for determining both operative indications and operative planning. It is difficult to assess intra-articular displacement and to plan screw placement for fixation of three-dimensional fracture patterns based on plain radiographs. Magnetic resonance imaging (MRI) does not play a large role in the preoperative workup of transitional ankle fractures. It is more useful in the follow-up period for assessing reasons for ongoing ankle pain such as ligamentous damage or osteochondral injuries. It can additionally help identify premature physical closure or bony bar formation.
Transitional ankle fractures involve both the distal tibial physis and the articular surface of the ankle. Although physeal malalignment can cause growth disturbance, there is typically not sufficient growth remaining at the distal tibial physis in adolescents with transitional ankle fractures to cause significant growth-related problems. Open reduction is indicated to reduce the articular surface as articular malalignment leads to arthritis of the ankle joint. Fractures with a residual diastasis at the articular surface of greater than 2 mm should be treated operatively. It is questionable whether there is even a role for closed reduction in an emergency room setting where the adolescent patient must be relaxed with IV sedation or general anesthesia for closed reduction. Articular surface gaps of less than 2 mm may be accepted, and those fractures may be treated with a long leg non-weight-bearing cast to address the rotational nature of the injury. Fractures with malreduction of the articular surface of greater than 2 mm have been correlated with poor long-term outcomes and should be managed operatively.
PREOPERATIVE PREPARATION/SURGICAL PROCEDURE
In between the time of presentation and the time of surgery, strict elevation is to be enforced to help reduce swelling. If severe soft-tissue swelling is present, it may be necessary to delay surgery while allowing soft-tissue swelling to decrease with elevation in order to help avoid wound healing complications. In the operating room, general anesthesia is indicated for complete relaxation. The patient should be prepared for open reduction on a radiolucent table with a nonsterile tourniquet in place and a bump
under the ipsilateral hindquarter. The image intensifier is prepped and draped to enter from the nonoperative side. It is critical that the image intensifier is carefully manipulated in order to obtain images exactly parallel to each fracture line in order to accurately assess displacement and confirm precise reduction.
under the ipsilateral hindquarter. The image intensifier is prepped and draped to enter from the nonoperative side. It is critical that the image intensifier is carefully manipulated in order to obtain images exactly parallel to each fracture line in order to accurately assess displacement and confirm precise reduction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree