Total Hip Arthroplasty for Post Traumatic Arthritis
Adam J. Schwartz
Mark J. Spangehl
Introduction
Hip fractures are estimated to increase from 1.6 million to 6.3 million worldwide by 2050, due in large part to an aging patient population (1). Indeed by the age of 80, nearly one-fifth of women have sustained a hip fracture, and by the age of 90 this number increases to approximately 50%. As the incidence of traumatic injuries involving the proximal femur continues to rise, one would expect a concomitant rise in the number of cases of posttraumatic arthritis, resulting from articular cartilage injury, hardware failure, secondary osteonecrosis of the femoral head, and nonunion or malunion of the fracture fragments leading to poor joint biomechanics.
Posttraumatic arthritis following fracture of the proximal femur occurs either as a direct result of articular cartilage damage at the time of fracture, or due to pathologic alterations in the biomechanical forces about the hip joint. The latter is more likely after proximal femoral fractures, as high-energy fractures of the proximal femur that directly damage the articular cartilage are less common than low-energy periarticular fractures. Posttraumatic osteoarthritis is the most common long-term complication of simple hip dislocation, occurring in roughly 24% of patients (2). This number increases to over 80% in the setting of combined dislocation and acetabular fracture (3).
Posttraumatic Arthritis: Femoral Side
General
Proximal femur fractures may be broadly classified as intracapsular or extracapsular (4). Intracapsular fractures may be further subclassified into femoral head and femoral neck fractures. The former are typically seen as a result of high-energy trauma, frequently in conjunction with an acute hip dislocation. These injuries are less common than femoral neck fractures which are largely seen in the elderly population following a low-energy injury mechanism. Epidemiologic studies indicate that extracapsular fractures are increasing with relative frequency, as a result of the increasing prevalence of this type of fracture pattern in the expanding elderly population.
Avascular necrosis of the femoral head following simple hip dislocation is estimated to occur in roughly 1% to 17% of cases (5,6). Debate exists as to whether the time between acute dislocation and concentric reduction increases the likelihood of osteonecrosis (2,7,8,9). Most authors would advocate for reduction within 24 hours of injury to avoid late effects of reduced blood supply to the femoral head. As noted previously, however, there is a considerable incidence of posttraumatic arthritis following simple hip dislocation, even in the absence of osteonecrosis.
Femoral head fractures result in a similarly high rate of posttraumatic arthritis, regardless of fracture classification or fixation method (10,11). In one recent long-term review of 20 patients with femoral head fractures of varying severity, virtually all (95.2%) patients demonstrated some degree of radiographic posttraumatic osteoarthritis, although function was considered excellent in eight (10). Care is taken at the time of femoral head fixation to counter-sink screws in an effort to maintain femoral head sphericity. As noted previously, however, development of radiographic degenerative changes is a virtual certainty following these articular injuries regardless of fragment displacement or hardware chosen.
The incidence of osteonecrosis following intracapsular femoral neck fracture is variable, and largely depends on the angulation and displacement of the initial fracture (12,13,14). The use of bone scan within 1 to 2 weeks following fixation was accurate in predicting the development of posttraumatic osteonecrosis at an uptake ratio of 90% or less compared to the intact side (15). In addition, at the time of open reduction, bleeding of the femoral head was found to be an accurate predictor of late-onset osteonecrosis in patients with femoral neck fractures treated with open reduction and cannulated screw fixation (16,17). Studies have implicated a tamponade effect and recommend decompression of the hip capsule at the time of fixation, particularly for younger patients (18,19,20,21). Comminution of the femoral neck, high degree of initial fracture displacement, and poor surgical technique have all been implicated as reasons for hardware failure following femoral neck fracture (22,23,24). Although a single episode of perforation into the joint with a guidewire has not been associated
with the development of posttraumatic arthritis, screws that perforate the femoral head may protrude into the joint with fracture settling over time, even if the screw is exchanged for a shorter one at the time of initial fixation (25).
with the development of posttraumatic arthritis, screws that perforate the femoral head may protrude into the joint with fracture settling over time, even if the screw is exchanged for a shorter one at the time of initial fixation (25).
Posttraumatic arthritis ensuing from osteonecrosis is less common in the setting of extracapsular peritrochanteric fracture, occurring in roughly 0.5% to 1% of fractures within the first 4 years following fixation (26). Debate exists as to whether this complication is the result of injury to the deep medial circumflex artery at the time of the initial fracture, or at the time of surgical fixation. Hardware failure following fixation of peritrochanteric femur fractures may result in abnormal joint biomechanics, or perhaps direct injury to the articular cartilage. Implant penetration by the femoral head screw into the joint may be seen in the setting of peritrochanteric fractures, either with screw and side-plate implants, or nails. Femoral head screw cutout is estimated to occur in up to 20% of intertrochanteric fractures, and is associated with poor bone quality, advanced patient age, poor reduction, blocking of the gliding mechanism, and poor implant placement (27,28). Increased distance from the tip of the screw to the apex of the femoral head on AP and lateral intraoperative images has been associated with higher rates of cutout (29).
Preoperative Planning
Preoperative planning begins with a thorough history and physical examination, as well as a comprehensive review of the patient’s prior surgical treatment record. Failed hardware and associated fracture nonunion may implicate an infectious etiology. All patients with pre-existing hardware should be screened for infection with inflammatory markers, including an erythrocyte sedimentation rate and a C-reactive protein, particularly those with pre-existing hardware. When these markers are elevated, consideration should be given to joint aspiration and/or core tissue biopsy and culture. Implant records should be obtained to determine whether special instrumentation might be necessary for hardware removal. The planning, principles, and techniques of hardware removal in the setting of revision hip arthroplasty, discussed elsewhere in this text, should be followed (30).
Surgical approach is largely determined by previous fracture pattern, existing hardware, and prior incisions (31). Multiple incisions may be present in the case of prior femoral nail placement. An effort should be made to incorporate prior skin incisions when possible, and to excise the pre-existing scar. The presence of heterotopic bone should be noted, and perhaps incorporated into the approach. The classification system described by Brooker et al. is useful to define the extent of the problem. Brooker III and IV lesions may require extensile tri-radiate exposure to adequately visualize both the femoral and acetabular sides. Consideration should be given to prophylaxis for prevention of heterotopic bone formation, preferably with preoperative radiation (32,33,34,35).
Surgical Considerations
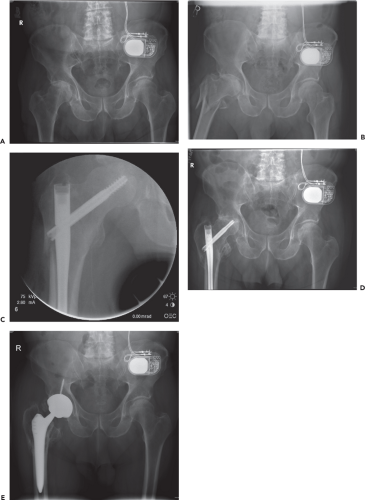
Dislocation of the hip prior to hardware removal may reduce the incidence of intraoperative fracture through stress risers at the sites of screw removal (Fig. 72.1) (36). If the degree of posttraumatic arthritis is severe, or in cases of associated protrusio, it may be difficult or impossible to dislocate the hip. Options in this situation include use of a trochanteric osteotomy or performing an in situ femoral neck osteotomy. The latter option will typically require initial removal of hardware, followed by manual extraction of the femoral head with the assistance of a corkscrew device or femoral elevator. If a cemented stem is chosen, a custom-mold using a rubber glove filled with cement may be used to prevent cement extrusion through the opening left by the femoral head screw during pressurization (37). Cement extrusion through previous drill holes has been associated with late postoperative femoral fracture, and in the setting of trochanteric osteotomy, may result in delayed healing or nonunion (38).
Osteotomy is frequently necessary to address proximal femoral deformity in the setting of underlying posttraumatic arthritis. Osteotomy may be performed prior to total hip arthroplasty (THA) as a staged procedure, or simultaneously (39,40,41). A staged approach offers the advantages of allowing for complete healing without threatening implant fixation or longevity and allowing for later reconstruction with more conventional implants. Consideration should be given to this approach in cases where the osteotomy would perhaps delay the need for arthroplasty (particularly in younger patients), or when hip arthroplasty is made technically too difficult without prior correction of the deformity. Occasionally, a corrective osteotomy prior to hip arthroplasty would allow for use of more conventional implants that utilize shorter segments of bone, which may be advantageous particularly in younger patients (40). The disadvantages of a staged approach include the necessity of two separate surgical procedures with separate recovery times, and the potential need for hardware removal at the time of eventual hip arthroplasty.
Simultaneous hip arthroplasty with corrective osteotomy is a reliable technique for complex femoral deformity (39,42,43,44). If femoral anteversion is expected to be 45 degrees or greater, consideration should be given to derotational femoral osteotomy or use of a modular implant (44). Contemporary implant designs are typically able to achieve adequate initial fixation even with multiple femoral fragments. Planning for femoral osteotomy is facilitated by the use of good-quality preoperative radiographs, and manual or digital overlay template techniques. The osteotomy should provide adequate correction and exposure, while simultaneously avoiding compromise of initial implant fixation. The use of cement should be avoided, and an effort made to preserve soft tissues and periosteum overlying osteotomy fragments to optimize healing (45). Various methods are available to achieve stable fixation of bone fragments, but most employ the use of various cerclage wiring techniques (46,47).
Implant selection is based upon severity of femoral deformity, residual bone quality, need for corrective osteotomy, and presence of existing hardware (40). Although cementless femoral components are associated with excellent long-term clinical results, the surgical technique and implant geometry are less forgiving than with cemented components particularly in the setting of pre-existing femoral deformity. Bony integration of the implant relies upon immediate rotational and axial stability (48,49). To achieve such stability, press-fit techniques and implant modifications (including tapered, tapered flat wedge, square tapered, and anatomic designs, among others) place significant stresses on the host bone
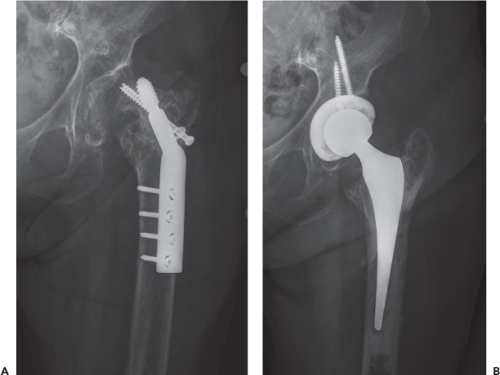
during implantation. The press-fit technique attempts to reduce micromotion by oversizing the femoral component relative to the native femur. The disadvantage of this technique is an increased risk of periprosthetic fracture, and subsequent loosening of the femoral component. In a series of over 20,000 primary THAs, Berry reported an incidence of periprosthetic fracture in 0.3% of cemented and 5.4% of uncemented primary THAs. If bone quality does not permit use of a cementless implant, consideration should be given to using cement (Fig. 72.2), although this technique carries the long-term risk of aseptic loosening, and extrusion of cement through prior drill holes and osteotomy lines as noted previously.
during implantation. The press-fit technique attempts to reduce micromotion by oversizing the femoral component relative to the native femur. The disadvantage of this technique is an increased risk of periprosthetic fracture, and subsequent loosening of the femoral component. In a series of over 20,000 primary THAs, Berry reported an incidence of periprosthetic fracture in 0.3% of cemented and 5.4% of uncemented primary THAs. If bone quality does not permit use of a cementless implant, consideration should be given to using cement (Fig. 72.2), although this technique carries the long-term risk of aseptic loosening, and extrusion of cement through prior drill holes and osteotomy lines as noted previously.
Modular implants that employ use of a proximal sleeve offer enhanced ability to achieve stability in the metaphyseal bone independent of diaphyseal diameter or geometry (Fig. 72.3) (50,51). Separation of the portion of the implant that achieves fixation distally from the proximal segment may improve intraoperative control of leg length, offset, neck length, and anteversion. Other studies have expressed long-term concerns regarding use of mixed metals, fretting corrosion, and taper fracture. Custom implants are another option to deal with severe proximal femoral deformity in the setting of posttraumatic arthritis (50




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree