Metal on Metal: The Whole Story
John V. Tiberi
Eric Schiffman
Martin Kosztowski
Young-Min Kwon
Case Presentation
A 70-year-old male with a history of a right and left metal-on-metal (MoM) total hip arthroplasty (THA) presented with bilateral diffuse hip pain radiating into the thigh. His right and left THAs were performed at separate settings approximately 7 years prior to presentation. He initially did very well and was asymptomatic after recovering from surgery until 3 years prior to presentation. Since that time, he has had persistent and slowly worsening pain. On physical examination, he had 4/5 abductor strength with a bilateral Trendelenburg gait. The remainder of the examination was negative. Radiographs (Figs. 92.1 and 92.2) showed bilateral MoM THAs with modular acetabular components. All implants appeared well fixed. The acetabular components were in approximately 5 degrees of retroversion. The femoral components appeared well positioned and sized. His serum cobalt and chromium levels were 7.5 ng/mL and 5.1 ng/mL, respectively. Magnetic resonance imaging (Fig. 92.3) of bilateral hips employing metal suppression parameters demonstrated extensive adverse local tissue reactions (ALTRs) including capsular thickening, large juxta-articular complex collection, and low-signal regions most consistent with metal debris.
Introduction
MoM bearings in hip arthroplasty have a long clinical history, having been used as early as 1938 by Phillip Wiles and 1953 by George McKee (1,2). The bearing used by Wiles was stainless steel and failed because of poor wear characteristics and imprecise design tolerances. Other early designs include the Ring and McKee–Farrar, composed of a cobalt-chromium alloy, and the first (stainless steel) and second (cobalt-chromium femoral head and acetabular liner with titanium alloy femoral stem and acetabular shell) generation Sivash (2). Although all experienced failures from similar mechanisms related to imprecise femoral head—acetabular component tolerances leading to high-frictional forces—excellent long-term results have been reported (3,4). In addition, in those patients without early failures, low rates of wear and osteolysis were observed. The combination of a relatively large number of early failures combined with the rising popularity of Sir John Charnley’s MoPE and cemented low-friction arthroplasty led to the decline in popularity of MoM by the 1970s.
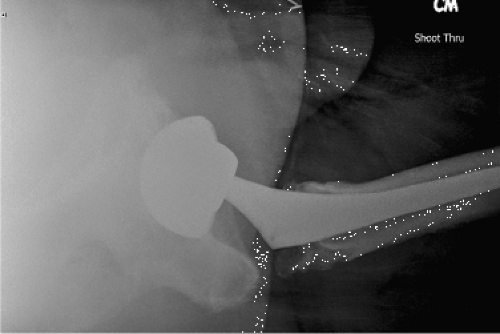 Figure 92.2. Shoot-through lateral view of the right MoM THA showing approximately 5 degrees of acetabular component retroversion. |
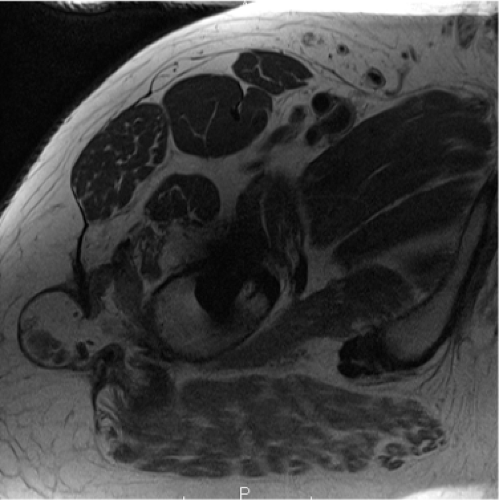 Figure 92.3. Metal suppression magnetic resonance imaging of the right hip showing capsular thickening, a large fluid collection, and low-signal regions most consistent with metal debris. |
Advances in materials, manufacturing, and implant design in MoM-bearing arthroplasty begot several highly desirable characteristics. High material strength minimizes the risk of gross material failure of the bearing surface and permits manufacturing of acetabular components that accommodate large-diameter femoral heads in both hip resurfacing and THA. Large-diameter bearings have greater range of motion (5) and a lower risk of instability (5,6), which is the leading cause of revision for THA in the United States (7). In addition, well-functioning MoM bearings have the potential for very low wear rates (8,9,10,11).
Because of these properties, there has been a rapid increase in the number of MoM hip resurfacing and large-diameter MoM total hip arthroplasty procedures performed. In 2009 it was estimated that 35% of all articulations used in the United States were MoM (12). Despite this surge in popularity, there are a number of concerns regarding MoM articulations. Effects from the systemic spread and accumulation of metal ions are poorly understood. Recent reports of early failure have put the utility of MoM articulations into question. The national registries of England and Wales and Australia have reported that the failure rate of THA with MoM bearings to be two- to threefold higher than contemporary THA with non-MoM bearings (13,14). The reported reasons for revision surgery include adverse periprosthetic soft tissue reactions and failure of osseointegration of the acetabular component.
Mechanisms of Failure
Systemic Considerations
MoM wear leads to the release of metal particles and metal ions. The particles are insoluble, whereas the ions are soluble and can enter the systemic circulation (15). Progressive systemic accumulation of metal ions is prevented by an effective renal clearance mechanism (16). Daniel et al. found that both the daily urinary excretion of metal ions and whole blood levels showed an early increase after MoM hip resurfacing, followed by a progressively decreasing trend (17). There has been concern about the effects of long-term exposure to elevated metal ion levels, especially since MoM hip resurfacing has been performed in younger patients who want to maintain active lifestyles. In animal models, cobalt and chromium wear particles have been shown to have carcinogenic potential (18), though currently available data does not support a causal link between risk of cancer and total joint arthroplasty (19). There have also been concerns regarding chromosomal damage and transplacental passage of metal ions (20,21). Recently there have been case reports of patients with MoM arthroplasty developing neurologic and cardiac complications (22,23).
Failure of Fixation
One mode of failure in modern MoM arthroplasty has been loose components. Often, failure of this type has been termed “aseptic loosening” by convention. This term implies loosening of a once well-fixed component. The early nature and appearance at revision suggests failure of osseous integration as a more accurate description of the mechanism in the majority of these cases. The preponderance of these failures involves the acetabular component with relative sparing of the femoral component. Some monoblock, cementless designs are at an especially high risk; however, similar failures have been observed in modular designs as well (24,25,26).
Adverse Tissue Reactions
Terminology
The understanding of periprosthetic soft tissue lesions in MoM arthroplasty is in constant evolution. The terminology in this area can be confusing. Metallosis refers to a visual description of macroscopic soft tissue staining and appears to be related to wear occurring via mode one (intended bearing surfaces) in MoM arthroplasty or modes two (nonintended bearing surfaces) and four (articulating nonbearing secondary surfaces) regardless of the bearing type (27,28). Aseptic lymphocytic vasculitis-associated lesions (ALVAL) is a histologic appearance of periprosthetic soft tissue observed in MoM bearings described by Willert et al. (29). The term pseudotumor has been used to describe a cystic or solid mass observed macroscopically or on imaging studies. Adverse reaction to metal debris (ARMD) and ALTR are both comprehensive terms that have been used to encompass all types of lesions; however, ARMD implies a relationship to wear while ALTR does not (27,30).
Etiology
The exact cause of adverse tissue reactions remains unknown. Available evidence suggests a complex interplay between
implant factors, surgical factors and patient factors: combination of wear-prone bearings and component malpositioning along with either a hypersensitivity to metal debris or a failure of the expected body’s response to debris (31). The implant debris leads to a synovial-like biomembrane with the capacity to produce collagenase, IL-1, TNF which are likely to be the mediators in bone resorption (32). These masses are heterogeneous in their appearance and have also been described as cysts (33,34), bursae, abnormal soft tissue reactions, and adverse reactions to metal debris (29,33,34,35,36,37,38). On histologic examination of periprosthetic tissue samples taken at the time of revision an ALVAL pattern is frequently but not always observed (37



implant factors, surgical factors and patient factors: combination of wear-prone bearings and component malpositioning along with either a hypersensitivity to metal debris or a failure of the expected body’s response to debris (31). The implant debris leads to a synovial-like biomembrane with the capacity to produce collagenase, IL-1, TNF which are likely to be the mediators in bone resorption (32). These masses are heterogeneous in their appearance and have also been described as cysts (33,34), bursae, abnormal soft tissue reactions, and adverse reactions to metal debris (29,33,34,35,36,37,38). On histologic examination of periprosthetic tissue samples taken at the time of revision an ALVAL pattern is frequently but not always observed (37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









