Total Hip Arthroplasty for Developmental Hip Dysplasia
Thomas L. Bernasek
Steven T. Lyons
Brian T. Palumbo
Introduction
Developmental dysplasia (DDH) in the adult hip is a common etiology of painful arthritis and can present with a wide variation of degenerative changes and anatomic deformity. The incidence of osteoarthritis (OA) secondary to DDH appears to have geographic and ethnic variation. For example, a comparison of Japanese Asians and Caucasian Americans found that, for adults who underwent total hip arthroplasty (THA), the etiology for arthritis was DDH in 78% and 6% of cases, respectively (1). Hip replacement in these patients requires an understanding of DDH deformity to guide implant selection and technique.
The degree of hip dysplasia, subluxation or dislocation and femoral anteversion creates a significant variation in deformity which requires knowledge of adult DDH anatomy and surgical reconstructive techniques. The mild cases present with a dysplastic or shallow acetabulum and can be similar in technique to a regular primary THA, while the extreme cases of subluxation or complete dislocation can be very difficult and challenging for even the seasoned reconstructive surgeon requiring extensive soft tissue releases, special implants, osteotomy and acetabular grafting or augmentation. A key to successful DDH THA is understanding the anatomic variations which create different presentations and reconstruction requirements.
The DDH hip can be described as (a) reduced, (b) subluxed, and (c) dislocated. Multiple classification systems have been described for DDH and include those by Crowe et al. (2), Hartofilakidis et al. (3,4), Eftekhar (5,6), and Kerboul (6,7,8). The widely referenced Crowe classification is a description based on the degree of subluxation of the femur in relation to the true acetabulum (2). Crowe type I represents less than 50% migration of the femoral head from the true acetabulum whereas type II has migration 50% to 75% proximal to the true acetabulum, type III, 75% to 100%, and type IV, a complete dislocation of the femoral head from the true acetabulum and frequently residing in a pseudoacetabulum. Since Crowe type II and III represent femoral head subluxation, another useful classification described by Hartofilakidis et al. notes three types of dysplastic hips: type 1 to type 3. In type 1 the femoral head remains in the true acetabulum, type 2 represents a low subluxation or dislocation of the femoral head from the true acetabulum, and type 3 a high dislocation from the true acetabulum with the head creating a pseudoacetabulum with the iliac wing. In this chapter we present DDH patient case studies that represent the full spectrum of DDH OA, then discuss the surgical options, common treatment complications and pitfalls, and literature results.
Case Presentations
The Reduced Dysplastic Hip
Case 1: A 49-year-old female with 5 years of left hip pain was referred to the Orthopedic office. She has been managed medically for years with nonsteroidal anti-inflammatory drugs (NSAIDs), pain medications, physical therapy (PT), and a cane with diminishing pain relief. Although healthy she reported a history of hip problems at birth that required her to wear a hip brace when very young. No prior surgeries. She had done well most of her life until progressive pain over the last 5 years.
Office examination demonstrated an antalgic gait requiring a cane for ambulation. Her range of motion (ROM) was 0- to 100-degree flexion with pain, adduction 5 degrees, abduction 5 degrees, internal rotation (IR) 0 degrees and external rotation (ER) 10 degrees with a positive Stinchfield test. Her opposite hip showed 120-degree flexion, 10-degree adduction, 50-degree abduction, 40-degree IR, and 45-degree ER with a negative Stinchfield test. Trendelenburg test was mildly positive on the left.
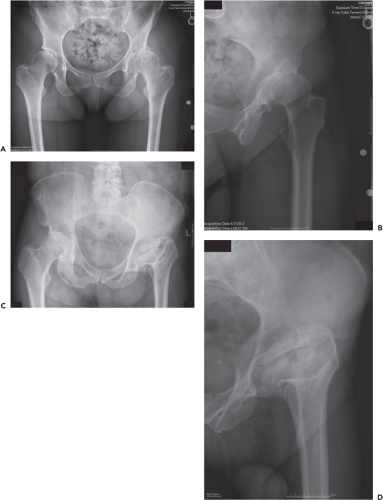
X-rays (Fig. 71.1A,B) showed bilateral dysplastic hips, worse on the left with arthritis and loss of superolateral joint space. Bone on bone contact is associated with large femoral head and acetabular cysts. Her center edge (CE) angles approached 0 degrees on each side. Having failed conservative measures for pain control, hip replacement was indicated.
Case 2: A 60-year-old male with left hip pain and a short leg which has been present as long as he can remember. He
reports that he was born with a “congenital defect” of the hip. He had closed treatment as an infant but no prior hip surgery. In recent years routine conservative measures such as NSAIDs and a cane had become ineffective. At times the patient cannot walk due to severe groin pain that radiates to the knee. He has worn a shoe lift for years.
reports that he was born with a “congenital defect” of the hip. He had closed treatment as an infant but no prior hip surgery. In recent years routine conservative measures such as NSAIDs and a cane had become ineffective. At times the patient cannot walk due to severe groin pain that radiates to the knee. He has worn a shoe lift for years.
Office examination showed a 6-ft 1-in, 200-lb male. A left antalgic gait is noted with an associated 1-in short leg. ROM is painful with 60-degrees flexion, 5-degree adduction, 5-degree abduction, 0-degree IR, and 10-degree ER. The limb is approximately 1 inch shorter than the right. The right hip showed full ROM without irritability.
X-rays (Fig. 71.1C,D) demonstrate a dysplastic, shallow acetabulum with a superolaterally oriented sourcil. The obvious deformation of the proximal femur includes coxa breva, coxa plana, coxa magna, and overgrown greater trochanter. The findings are consistent with DDH OA associated with long standing avascular necrosis of the femoral head. Having failed all conservative measures for pain control, hip replacement was indicated.
The subluxated Dysplastic Hip
Case 3: A 68-year-old female presented to the office with a multiyear history of left hip dysplasia which was diagnosed as a child. She reported leg length discrepancy and a left shoe lift. She has developed increasingly severe groin and lateral hip area pain. Prior treatments had exhausted the ladder of therapy and she was ready for total hip replacement. No prior hip surgeries. She is generally healthy.
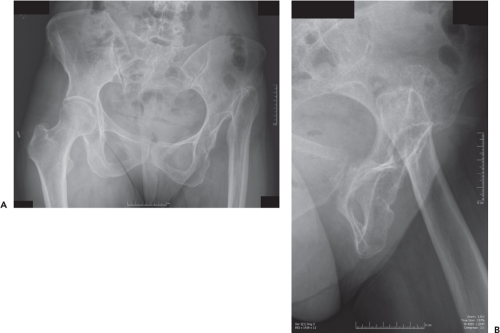
Examination revealed painful left hip ROM flexion of 85 degrees, adduction 5 degrees, abduction 15 degrees, ER is 5 degrees, IR is 10 degrees and extension of 10 degrees. Her popliteal angle with the hip flexed at 90 degrees is −10 degrees extension. The right hip ROM was flexion 90 degrees, adduction 10 degrees, abduction 35 degrees, ER 30 degrees, IR 10 degrees, and extension is 10 degrees. She has a 1.5 inch leg length discrepancy, short on the left. She was neurovascularly intact. X-rays (Fig. 71.2) demonstrated a normal right hip and advanced degenerative arthritis of the left hip secondary to DDH with proximal and lateral femoral head subluxation, a large central acetabular osteophyte, coxa magna, and coxa plana.
The Dislocated Dysplastic Hip
Case 4: This 50-year-old female presented to the office for evaluation of left hip pain which has been severe and worsening for about 2 years. She reports a history of left hip dislocation as an infant and that it was not treated. She stated that she grew up with no pain or complaints and had a very physically active childhood with sports. She reported a pain increase over the recent few years with activities such as walking, standing, and prolonged sitting. Pain decreased with rest, Tramadol, Vicodan, Ibuprofen, and Tylenol. She was otherwise healthy and denied prior surgery.
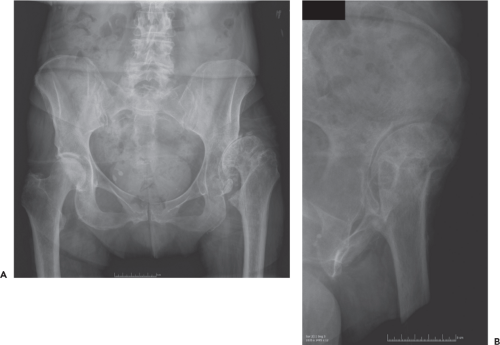 Figure 71.2. A, B: Sixty-eight-year-old female with many years of left hip pain due to OA secondary to DDH with hip subluxation. Classification is Crowe Type III, Hartofilakidis Type 2 hip dysplasia. |
Physical examination reveals a left Trendelenburg gait, 8 cm left leg shortening. Left hip ROM is flexion 85 degrees, abduction 25 degrees, adduction 40 degrees, ER 60 degrees, IR 40 degrees with a positive Stinchfield and Patrick’s test. Right hip ROM is flexion 110 degrees, abduction 45 degrees, adduction 30 degrees, ER 50 degrees, IR 30 degrees, and extension 10 degrees.
X-rays (Fig. 71.3) showed a high dislocation of the left hip with pseudoacetabulum articulation. She had pelvic tilt with marked left coxa breva, femoral head cyst formation, and femoral hypoplasia compared to the right side.
Preoperative Evaluation of the Dysplastic Hip
Dysplastic hip anatomy presents with a predictable dysmorphism that varies with increased degree of dysplasia. (Crowe I to IV) Careful evaluation and knowledge of the dysplastic patient is critical to surgical planning and a favorable outcome. Incomplete information and preparation can result in unanticipated operating room events that can usually be easily avoided to maximize surgical success.
History
The patient’s history can provide important insights into the DDH hip. An assessment of pain is important and dictates the therapeutic measures. For example, a dislocated DDH patient (Crowe IV) can present with no pain and minimal activity limitations despite leg length discrepancy, a Trendelenburg gait, and a markedly abnormal x-ray. Such a patient is not a surgical candidate despite an alarming x-ray. Modern guidelines require documentation of conservative treatment which is appropriate for OA secondary to DDH and includes NSAIDs, exercise for stretching and strengthening, ambulatory aids, shoe lifts, and weight loss as appropriate. Severe pain and compromised quality of life unresponsive to conservative measures indicates surgery.
When surgery is indicated, important information includes the recent and distant treatment history (if possible obtain reports). Also the need for a shoe lift or history of prior surgery will be relevant to any surgical plan.
Physical Examination
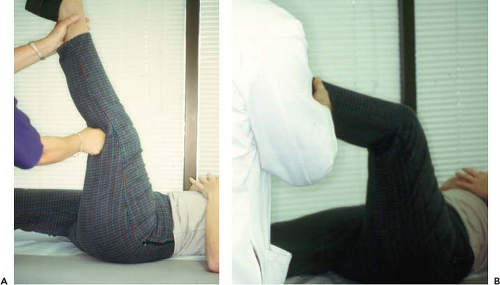
ROM, gait, leg length, neurologic status, and prior scars are all important to note. Observing the patient walk gives a lot of helpful data on the efficiency of their gait and whether it is antalgic. A Trendelenburg gait is usually seen with high degrees of dysplasia especially Crowe III and IV although not necessarily antalgic. The dislocated Crowe IV can have painless hips for many years until they start to become symptomatic. Leg length discrepancy is defined by direct measurement supine and by standing and measuring the leg length with blocks to level the pelvis to define a functional discrepancy. While supine, flexing the hips and comparing the sides reveals LLD (Fig. 71.4). Supine the legs can be measured from the anterior superior iliac spines (ASIS) to the medial malleoli.
 Figure 71.4. A, B: Leg length discrepancy due to hip subluxation in a DDH patient. The clinician must determine the source of shortening as femoral, tibial, or both for accurate diagnosis. |
ROM is an important predictor of potential problems with the surgical exposure if the hip is stiff. Generally the high dysplastic or dislocated hip can require a shortening derotational osteotomy (SDO) whereas in lower degrees it may not be as clear. Measuring the popliteal angle can indicate hamstring and soft tissue contracture and is a proxy for neurovascular structure elasticity. The popliteal angle is measured while supine, with the hip flexed to 90 degrees and the knee extended maximally. The residual flexion angle of the knee is measured (Fig. 71.5).
Comparison of hip IR suggests the degree of femoral anteversion to expect (Authors’ preference—evaluate patient seated with knees bent over the side of the table). It is not uncommon to see much greater IR of the dysplastic hip compared to the nonaffected side. If both hips are dysplastic then similarly the surgeon would see excessive IR bilaterally. This implies increased femoral anteversion which can affect surgical decision making and predict deformity, such as anterior acetabular wear due to excessive femoral head contact force. Such findings can suggest the need for a modular femoral component to dial out anteversion, or the need for an osteotomy to derotate the anteversion.
The need for a neurovascular examination to ensure that the preoperative state is known and the postoperative condition is unchanged is obvious. With the large number of soft tissue releases and mobilization needed in difficult cases, the sciatic, obturator and femoral nerves, and associated vascular structures are at risk. Evaluate lower extremity motor function
in all muscle groups of the thigh and leg to rule out existing neurologic deficit and to document function. Electromyogram and nerve conduction (EMG/NCV) may be warranted for supplemental documentation if positive or ambiguous findings are present. Vascular evaluation including the dorsalis pedis and posterior tibial pulses should be documented.
in all muscle groups of the thigh and leg to rule out existing neurologic deficit and to document function. Electromyogram and nerve conduction (EMG/NCV) may be warranted for supplemental documentation if positive or ambiguous findings are present. Vascular evaluation including the dorsalis pedis and posterior tibial pulses should be documented.
Radiographic Examination
Defect analysis by x-ray imaging should include AP hips and pelvis (pelvis included for comparison to contralateral hip), Lauenstein (frog leg) lateral, a cross-table or true lateral view of the hip and an AP and lateral of the affected femur. In addition to dysplastic changes, look for evidence of prior surgery or deformity such as pelvic osteotomy, iliac crest deficiency from being used as donor bone graft site or femoral shaft angular deformity, retained hardware or defects. CT scan can be useful for complex deformity and should include the pelvis, the hip joints, and a slice through the distal femoral condyles which allows accurate measurement of proximal femoral anteversion. Acetabular bone stock, anteversion, and bone defects are readily analyzed with this study. In general, there is no use for MRI, bone scans, or other radiographic modalities, as they do not add much helpful information.
Contraindications
Contraindications include active infection or medical comorbidity that threatens life or surgical outcome, severe neuromuscular deficit or patients who are noncompliant or are unable to cooperate with postoperative restrictions and rehabilitation (severe mental retardation, Alzheimer disease, etc.).
Surgical Planning
Implant Selection
The ultimate success of DDH reconstruction can be dependent in large part on the choice of implant. Intraoperative findings can change implant requirements, therefore the surgeon should prepare by having the most likely implants and implants for the “bail out” circumstance. The acetabular component workhorse is the hemispherical porous shell with holes for screw fixation. As backup a revision acetabular shell that allows for more screws, offset adjustment, and augmentation should be available. Small stature patients, hypoplastic acetabula, and distorted anatomy are common in DDH and often require very small press-fit components. The smallest sizes are special order devices which should be ordered routinely as back up. Also order the corresponding small head sizes routinely. For example, the authors’ preference is the DePuy Bantam series of cups which offers sizing down to a 38-mm shell. Sizes 38, 40, and 42 mm require a 22-mm head. Since 22-mm sized heads are not typically kept “on the shelf” they need to be ordered ahead of time. Additional preparation includes metal wedge augments, reconstruction rings and shells, bulk and particulate graft with the associated burrs for preparation and screws and washers for fixation.
Femoral components should be available to address the routine and complex case. Since increased anteversion is a common finding in even mild DDH, modular implants which allow rotational adjustment are useful and are the authors’ preference. Modular stems such as the SROM from DePuy or the Empirion from Smith and Nephew are well suited for this application because they achieve proximal fixation with a porous sleeve and distal fixation via splines on the stem. The metaphyseal sleeve has two shape variations in the SROM system which is a cylinder with and without a “spout.” The former is useful for cylindrical proximal femora (Fig. 71.3) and must be specially ordered. Long stems are recommended and should be available for osteotomy fixation or improved implant stability if needed. The authors have these available for all DDH cases. In addition cerclage cables, femoral plates, and screws should be routinely available.
Surgical Technique
The patient is secured rigidly into the lateral decubitus position; the authors prefer a post system (Montreal) which contacts both anterior superior iliac spine (ASIS), the ischium, and the sacrum thereby firmly controlling the pelvic position (Fig. 71.6). After sterile prep and drape a lateral skin incision is centered over the femur of the proximal thigh. The incision is curved slightly posteriorly proximally. The fascia lata is incised the length of the incision, anterior and posterior flaps are developed.
Arthrotomy: Minimal deformity such as the Crowe I with minimally increased femoral anteversion can be approached via the surgeon’s preference for THA. For advanced deformity, we recommend the posterior approach. The short external
rotators are exposed, detached, and posterior capsulotomy is performed. The hip is dislocated and the femoral head removed using an L-shaped osteotomy (this accommodates the SROM modular hip). The proximal femur is mobilized by partial or total capsulectomy, removing sufficient capsule to expose the true acetabulum. Difficulty with femoral mobilization is frequently due to contracted anterior capsule which is excised as necessary for exposure. A dislocation or high subluxation often has an elongated capsule which articulates medially with the femoral head. This should be excised.
rotators are exposed, detached, and posterior capsulotomy is performed. The hip is dislocated and the femoral head removed using an L-shaped osteotomy (this accommodates the SROM modular hip). The proximal femur is mobilized by partial or total capsulectomy, removing sufficient capsule to expose the true acetabulum. Difficulty with femoral mobilization is frequently due to contracted anterior capsule which is excised as necessary for exposure. A dislocation or high subluxation often has an elongated capsule which articulates medially with the femoral head. This should be excised.
 Figure 71.6. Pelvic position rigidly fixed by contact of posts on pelvis (ASIS, Ischial tuberosities, Sacrum). |
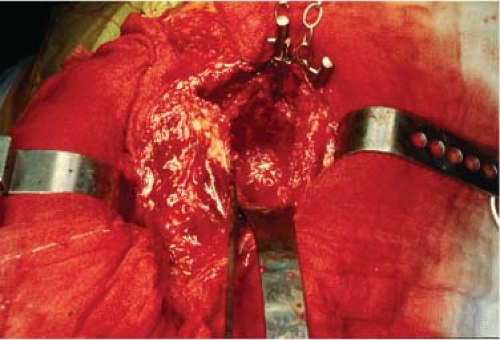
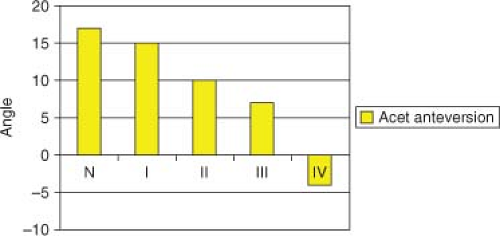
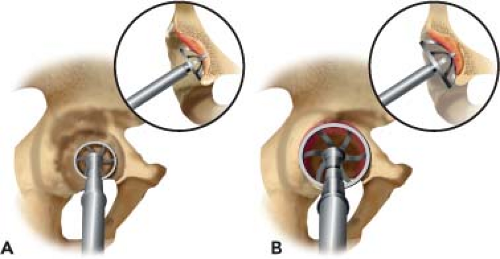
Acetabulum: A cobra retractor placed anterior-inferiorly to the acetabulum retracts the femur anteriorly and allows full acetabular exposure (Fig. 71.7). The acetabular anatomy varies depending on the severity of the DDH and is typically anteverted in mild deformity with decreasing anteversion in higher subluxations and dislocation (Fig. 71.8) (9).
The acetabulum is often deficient superolaterally with a very small diameter for which the surgeon should be prepared with small size components. Identification of the cotyloid fossa is an important guide to reaming the anatomic center for the acetabular component (Fig. 71.7). In the subluxed hip, a central acetabular osteophyte often obscures this structure requiring bone removal for exposure. Once the bone, labrum, pulvinar, and peripheral soft tissues are excised and the acetabular fossa identified, sequential reaming begins. The fossa is carefully enlarged while maintaining a central position until a concentric bony bed is developed. A reverse or “compaction reaming” technique is routinely employed in osteopenic bone. Medialization by reaming to the periosteum of the medial wall of the acetabulum increases coverage and can be required in peripherally deficient acetabula. The medial reaming depth is guided by the thickness of the medial wall which is routinely assessed by a 1/8-in drill hole through the fossa measured with a depth gauge. Do not overream the anterior and posterior walls by attempting to achieve reamer contact with deficient superolateral bone (Fig. 71.9).
Once reamed, trialing is performed to assess fit. The cup will often be uncovered superolaterally and will still achieve the mandatory stable fixation. The authors’ prefer a press-fit cup with screws. A decision regarding superolateral acetabular augmentation with metal augment, bulk autograft or allograft, or a reconstruction ring is made at this juncture. Structural bone grafting or augmentation is indicated when the cup is unstable due to bone deficiency. The acetabular component is placed using a 1- to 2-mm press fit with orientation in about 40-degree abduction and 15- to 30- degree anteversion. Supplemental fixation with screws is performed routinely.
Femur: Deformities typically include increased anteversion proximally and small femoral dimension. Femoral preparation is performed prior to osteotomy unless femoral deformity prevents straight axial reaming (e.g., congenital or acquired angular deformity of the femoral shaft). SROM preparation requires three basic steps: (1) straight reaming of the shaft to accommodate the minor diameter of the stem (0.75, 1.0, or 1.25 mm less than the major diameter for the SROM depending on stem diameter), (2) conical reaming of the metaphysis, (3) triangular reaming of the metaphysis. Steps 2 and 3 prepare for the metaphyseal cone. Trial components are placed with the femoral neck placed in proper anteversion (Fig. 71.10).
In high subluxations or dislocations the local soft tissue, contracted muscles and/or neurovascular bundle tension prevent femoral head reduction. SDO to decompress the soft tissues is indicated in this circumstance. The trial stem is removed and subtrochanteric osteotomy performed below the metaphyseal triangle (this usually correlates with the superior border of the gluteus maximus tendon (Fig. 71.11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree