Tibiotalocalcaneal Fusion Using an Intramedullary Nail
James K. DeOrio
DEFINITION
A surgical procedure in which the ankle and the subtalar joint are arthrodesed simultaneously
ANATOMY
The tibiotalar joint is bound by the medial malleolus, the fibula (lateral malleolus), anterior retinaculum and tendinous structures with the neurovascular bundle, and posteriorly by the flexor hallucis longus (FHL) and Achilles tendon.
The posterior tibial nerve lies immediately adjacent to the FHL tendon on the medial side.
PATHOGENESIS
Any trauma or inflammatory process which affect the ankle and subtalar joint simultaneously can cause pain in both of these joints. So too can the ankle be irreparably damage with a failed total ankle with so much fibrosis in the subtalar joint that it is not feasible to preserve it.
Because the rod stabiles both the ankle and subtalar joint, it may be used in paralytic conditions and when the talus is avascular and both the ankle and subtalar joints have been affected.
NATURAL HISTORY
The natural history is for the pain to increase because of increasing damage and loss of motion in these two joints. The prognosis is poor without surgery.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient complains of generalized pain across the anterior aspect of the ankle (ankle joint) and in the sinus tarsi (subtalar joint).
They have a limited range of motion in these joints and they are often painful on attempted manipulation and deep palpation.
IMAGING AND OTHER DIAGNOSTIC STUDIES
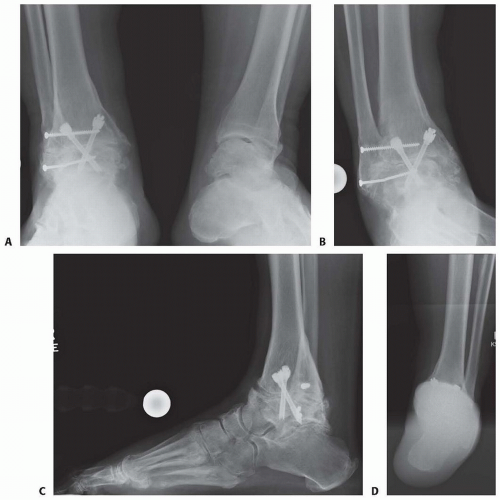
Diagnostic imaging consists of standard standing anteroposterior (AP), lateral, and mortise views of the ankle.
Additional standing full foot films are necessary, including a calcaneal view to ensure that the patient does indeed have a problem in the ankle and subtalar joints.
Frequently, a computed tomography (CT) scan of the ankle is necessary to confirm this fact.
DIFFERENTIAL DIAGNOSIS
Inflammatory arthropathy (rheumatoid arthritis, gout, hemosiderosis, etc.), trauma, failed ankle replacement, avascular necrosis of the talus and/or tibia, spastic paralysis, Charcot arthropathy, failed ankle fusion with subtalar arthritis, and resectable tumor with bone loss
NONOPERATIVE MANAGEMENT
Nonoperative treatment included bracing, orthotics, nonsteroidal anti-inflammatory drugs (NSAIDs), and injections of steroid and narcotic medication.
SURGICAL MANAGEMENT
The indications for surgery are coexisting painful inflammation in the ankle and subtalar joints simultaneously. This procedure is indicated when it is believed that neither ankle fusion nor subtalar fusion alone would suffice in producing a relatively painless functional limb.
It must be discussed with the patient that for whatever reason, they are not a good candidate for ankle replacement and subtalar fusion to deal with this problem (FIG 1).
Preoperative physical examination is mandatory to ensure that the approach is appropriate when considering previous incisions, trauma, free flaps, wound healing problems, and deformity.
Positioning
Although a tibiotalocalcaneal (TTC) arthrodesis may be accomplished in a supine and even lateral position, because insertion of the calcaneal screws is best done posterior to anterior, the prone position of the patient is desired. This position allows the leg to be shifted off the table for easy AP and by rotating the leg, a lateral x-ray with fluoroscopy. The tibial screws are inserted with the knee flexed 90 degrees.
Be careful to avoid the side paddle on the table near the thigh because this will prevent the leg from being shifted off the table.
Approach
Approach can be anterior, lateral, and posterior.
The disadvantage of the anterior approach is the need to make a separate incision for preparation of the subtalar joint.
The lateral approach is discouraged because of the need to resect the fibula, a technique that is believed to be outmoded and contributes to some subsequent valgus deformities if the ankle or subtalar joint do not heal.1
The posterior approach allows preparation of the ankle and subtalar joint simultaneously and has an angiosomic pattern that is ideal for healing.
TECHNIQUES
Exposure
Superficial Incision
The incision can be made just lateral to the Achilles but I prefer a midline, longitudinal Achilles tendon approach4 (TECH FIG 1).
It begins 8 cm above the posterosuperior aspect of the calcaneus and extends to the inferior surface of the calcaneus.
The tendon is split down the middle and the attachment on the calcaneus is relieved both medially and laterally. Remember, this is where the posterior to anterior screws are inserted anyway, and this increased release facilitates exposure of the ankle and subtalar joint simultaneously.
In extreme cases of equinus, one can do a Z-lengthening of the Achilles or completely remove the attachment onto the calcaneus.
Deep Incision
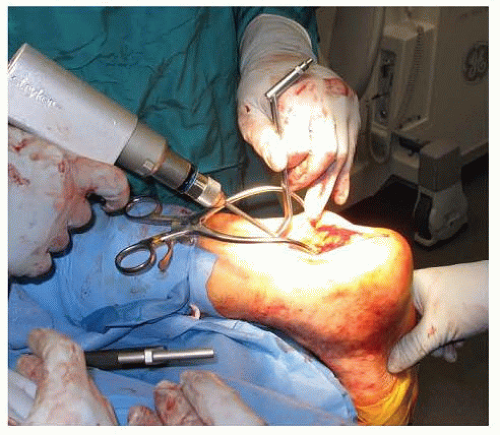
Once through the Achilles tendon, the deep retinaculum is cut and the flexor hallucis muscle bellies are visualized.
The muscle belly is followed distally and the FHL tendon is dissected off the calcaneus for mobility. The muscle belly is free and retracted medially. Use of the Henley retractor can assist with the visualization.
Ankle Exposure and Subtalar Exposure
Now, the posteroinferior tibial lip is exposed and removed to facilitate entry into the ankle joint. Using a blunt periosteal elevator, the ankle joint and subtalar joint are free from any adhesions. Exposed cartilage is removed from both joint. It helps to use
a lamina spreader, both medium and extra large to be able to open these joints. A distraction pin separator is usually necessary.

TECH FIG 1 • After an anterior exposure to remove his previous hardware, patient is opened straight posteriorly through the Achilles tendon to expose his ankle and subtalar joint.
If there is a total ankle in place, the polyethylene is removed first. To remove the talar component first and then the tibial component, a small reciprocating and oscillating saw is used to cut free any bony attachment so as to preserve maximum bone continuity.
If there is an intramedullary (IM) tibial component, it may be necessary to window the posterior tibial for exposure. This way, the reciprocating saw can maneuver around the stem and free up most of the ingrowth bone.
For the INBONE prosthesis, the base plate can be removed with an impactor and the wrench can be inserted around the last stem piece and then impaction begins on the wrench. A large bone hook placed with in the INBONE stem can help to counteract the posterior impaction force to keep the tibia from breaking at the level of the ankle.
▪ Débriding the Ankle and Subtalar Joint
Removal of the cartilage and or soft tissue débride can be accomplished with curettes, rongeurs, sharp dissection with a knife, a burr, a saw to cut the talar surface slightly, or even a small acetabular reamer (38 mm) to speed up the process.2
The tool is taken in the wound, protecting the posterior tibial nerve and can be used to remove soft tissue and leave a concavity in the tibia into which a femoral head can be inserted if necessary.
If there is complete avascular necrosis of the talus, I like to remove the posterior half of the talus and replace that with a femoral head.
If there is eburnated bone present, drilling the bone extensively with a 4.5-mm drill will break down the bone to allow vascular ingress more easily (TECH FIG 2).
▪ Bone Grafting
Once the joint is cleaned and the surface prepared, bone graft is added. I routinely use bone morphogenetic protein (BMP) sheets laid anteriorly, medially, and laterally.3 Onto this is laid up to 40 mL of thawed frozen cancellous bone. This is followed by a trimmed femoral head to fit the space.
I usually trim the sides and the base of the head to make it fit and then impact it into position.
This may also be done after preparing the leg for the rod because the head will want to spit out posteriorly as you prepare leg for the rod.
If it is done now, you can put some posterior Steinmann pins into the head and surrounding bone to get it to stay in place.
▪ Preparation of the Leg for the Nail
Depending on the manufacture’s rod you are using, preparation of the leg for the nail may vary. For purposes of detailing the surgical procedure here, I will use the A3 nail.
Place a guide pin into the calcaneal fat pad using the pin placement guide (TECH FIG 3A-D) or place it free hand parallel to the calcaneal cuboid (CC) joint, about 20 mm posterior to the joint and in the middle of the calcaneal fat pad.
If you aim just slightly laterally and anteriorly, when the rod is placed, you will force the foot into dorsiflexion and valgus and help void plantarflexion and varus.
Note that in TECH FIG 3C, you see an osteotomy in the fibula. This was done to reduce the patient into a hindfoot valgus position. Failure to do so would have caused the patient to walk on the side of his foot. However, it has never been necessary to remove the fibula which adds to the support of the final construct.
The angulated drill sleeve is used to find the place laterally and posteriorly to place the incision for the reamers.
Once the guide pin is in place, ream the guide pin starting with fixed reamers to the tibiotalar joint (TECH FIG 4A-G) and then insert a longer ball-tipped guide rod up the tibia and ream ½ mm larger than the intended rod for the shorter rod 150 to 180 mm and 1 mm larger for the larger rods 210 mm (TECH FIG 4H-K).
Add a femoral head allograft and additional cancellous bone, insert the guide pin again, check its position with the fluoroscope (TECH FIG 5), and then reream a hole into the bone graft to accommodate the rod.
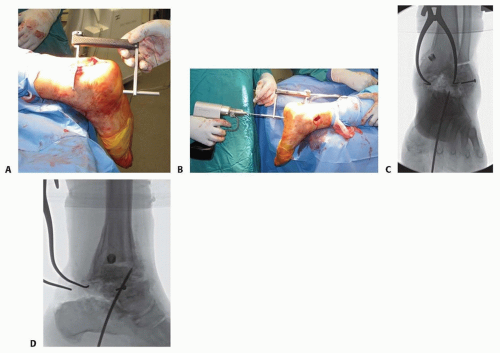 TECH FIG 3 • A. A pin placement guide is now inserted into the ankle joint with its distal tip just anterior and lateral to talar dome center. B. The guide pin is now placed through the guide until it reaches the tibial plafond. It is then sitting in the calcaneus and talus. C,D. Checking the guide pin placement on AP and lateral x-rays, respectively. Note how the guide pin is situated anterolateral to the talar dome. Then, when the foot is brought into dorsiflexion and valgus, the rod will go up the tibia and place the foot in the popper position.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|