Tibiotalocalcaneal Arthrodesis Using a Medullary Nail
George E. Quill Jr.
Stuart D. Miller
DEFINITION
Tibiotalocalcaneal arthrodesis is the surgical procedure to simultaneously fuse the ankle and the subtalar joints.
In cases of posttraumatic, neuropathic, or avascular talar body bone loss, tibiocalcaneal arthrodesis may be indicated. The term pantalar arthrodesis refers to the surgical procedure to fuse all bones that articulate with the talus: the distal tibia, calcaneus, navicular, and cuboid. In essence, this is a combined ankle and triple arthrodesis.
In our opinion, the term medullary refers to the inner marrow cavity of a long bone and the word intramedullary is a redundant, less useful term.
The goal of tibiotalocalcaneal arthrodesis is to create a painfree ankle and hindfoot that are biomechanically stable and fused in functional position.
In our hands, tibiotalocalcaneal arthrodesis is a salvage operation performed for severe ankle and hindfoot deformity, bone loss, and pain.
ANATOMY
Tibiotalocalcaneal arthrodesis aims to recreate physiologic ankle and hindfoot alignment with a plantigrade foot position (the foot is at a 90-degree angle to the long axis of the tibia) and about 5 to 7 degrees of hindfoot valgus.3, 10
In general, rotation of the foot relative to the longitudinal axis of the tibia in the coronal plane is congruent with the anterior tibia—that is, the second ray of the foot is usually in line with the anteromedial crest of the tibia.
Hindfoot position influences forefoot position. With longstanding ankle and hindfoot deformity, forefoot pronation, supination, adduction, and abduction may be affected. Proper positioning of a tibiotalocalcaneal arthrodesis must take forefoot position into account. Ideally, in stance phase, the foot has near-equal pressure distribution under the heel and first and fifth metatarsal heads.11
NATURAL HISTORY
Severe ankle and hindfoot deformities and pathologic processes result in disabling pathomechanics and, when left untreated, often confine patients to cumbersome brace use, limited ambulation with assistive devices, or a wheelchair.7
Tibiotalocalcaneal arthrodesis is a major reconstructive process usually applied to otherwise disabling conditions.5, 6
Gellman et al2 noted that the dorsiflexion and plantarflexion deficits after ankle fusion compared to the nonfused contralateral ankle were 51% and 70%, respectively. Surprisingly, for tibiotalocalcaneal arthrodesis, dorsiflexion and plantarflexion deficits were 53% and 71%, respectively.
This same study concluded, however, that inversion and eversion were 40% less after tibiotalocalcaneal fusion than after tibiotalar fusion alone.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient being considered for tibiotalocalcaneal arthrodesis with a medullary nail presents with a myriad of orthopaedic pathology affecting gait, weight bearing, and ability to earn a living.
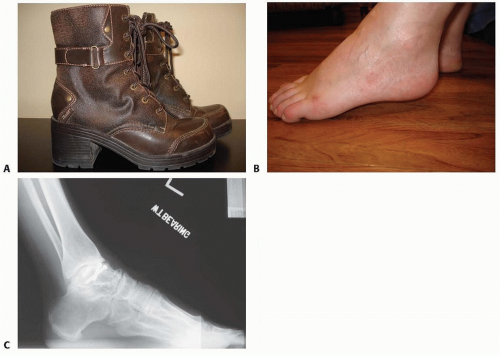
This patient may present with limited mobility, an equinus posture associated with genu recurvatum, and transverse plane deformity ranging from severe varus and instability of the hindfoot through profound valgus and ulceration over the medial structures (FIG 1).6, 9
The neuromuscular or neuropathic patient may present with ulceration, intrinsic muscle loss, and multiple fractures in various stages of healing.6
The posttraumatic patient often has a compromised soft tissue envelope, previously placed hardware, and already medullary canal sclerosis that must be considered in preoperative planning (FIG 2).7 Evaluation must include gait and weight-bearing posture, assessment of the soft tissue envelope, and a thorough neuromuscular examination.
IMAGING AND OTHER DIAGNOSTIC STUDIES
We routinely obtain three weight-bearing radiographs of the ankle and foot. As many of these patients have deformity, we often obtain additional long-cassette radiographs of the ankle or even mechanical axis views of the lower leg from the hip to the foot.
Posttraumatic and osteoarthritis
Radiographs may reveal joint space narrowing, osteophyte formation, and subchondral sclerosis and cysts, all characteristic of osteoarthritis. Posttraumatic deformity and retained hardware may be identified and must be considered in preoperative planning (FIG 3).7, 8, 9
Rheumatoid arthritis and other inflammatory arthritides
Radiographs typically identify periarticular erosions and osteopenia.4
Neuropathic arthrosis or Charcot neuroarthropathy
In our experience, this presentation is radiographically characterized by numerous fractures or microfractures in various stages of healing, hypertrophic new bone formation, and loss of normal weight-bearing architecture.
Plain tomography or computed tomography (CT) may further define deformity, arthritis, bone loss, and prior malunion or nonunion (FIG 4).
We have not found three-dimensional CT reconstructions helpful in the routine setting.
CT is also useful in assessing progression toward union following tibiotalocalcaneal arthrodesis.
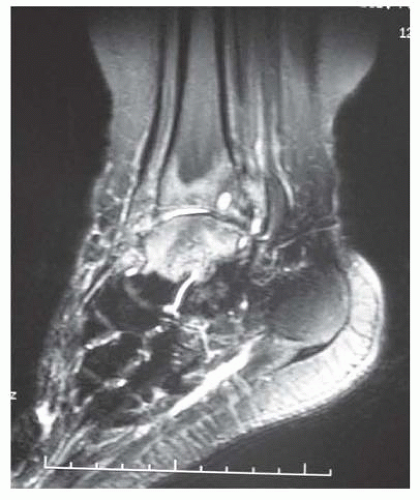
Magnetic resonance imaging (MRI) may complement CT by evaluating for fluid in and around the joints, bone marrow
edema, talar vascularity, infection, and periarticular tendon and ligament pathology (FIG 5).

FIG 3 • (continued) lateral radiograph (C) of an obese 69-year-old man after valgus nonunion of attempted tibiotalar arthrodesis.
Technetium 99 bone scans may be useful in the evaluation of osteonecrosis after talus fracture, arthritic involvement of one or several joints, stress fracture, or neoplasm.
Indium-labeled white blood cell scans can be helpful in the diagnosis of osteomyelitis or septic arthritis.
DIFFERENTIAL DIAGNOSIS
Primary and secondary osteoarthrosis, including posttraumatic osteoarthritis
Rheumatoid arthritis and other inflammatory arthritides (gout, pseudogout, pigmented villonodular synovitis, septic arthritis, psoriatic arthritis, spondyloarthropathy, Reiter syndrome)
Neuropathic arthropathy (diabetes mellitus, spinal cord injury, hereditary sensory and motor neuropathy, syringomyelia, congenital indifference to pain, alcoholism, peripheral nerve disease, tabes dorsalis, and leprosy)
Infectious arthritis (sepsis, open trauma, or previous surgical procedure for fixation of fractures)
Arthritis and joint subluxation resulting from generalized ligamentous laxity, mixed connective disease, posterior tibial tendinopathy, spring ligament insufficiency
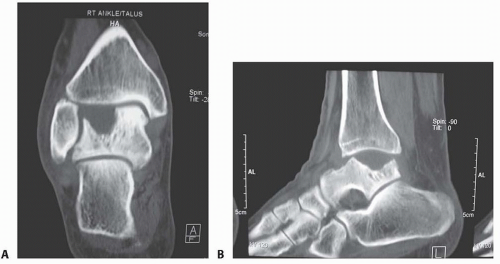 FIG 4 • Coronal (A) and lateral (B) CT images of a 48-year-old man with massive osteochondral talar insufficiency. |
NONOPERATIVE MANAGEMENT
Selective (diagnostic) injection of local anesthetic may help locate the exact anatomic source of the patient’s pain.
Tibiotalar arthritis may be associated with a stiff, painful subtalar joint that has a relatively normal radiographic appearance.
The injection of 5 to 10 mL of 1% lidocaine into the subtalar joint can clarify whether the pain may not be isolated to the ankle but in fact be generated in both the ankle and subtalar joints.
This has important implications when considering isolated tibiotalar versus tibiotalocalcaneal arthrodesis. We do not routinely incorporate the subtalar joint into the arthrodesis when performing an ankle arthrodesis. In select cases of endstage ankle arthritis associated with severe deformity and talar bone loss, we consider including an otherwise normal asymptomatic subtalar joint in the fusion mass achieved for tibiotalocalcaneal fusion. Alternatively, an injection carefully placed in the peroneal tenosynovial sheath may prove that pain may be related to the tendons rather than the joint.
Although often challenging for the patient with deformity, we recommend bracing for the patient with prohibitive medical illness or a dysvascular extremity, particularly for
the patient with a nonfixed, passively correctible deformity. A custom-molded polypropylene ankle-foot orthosis (AFO) or a supramalleolar AFO with Velcro closures may be considered as an alternative to tibiotalocalcaneal arthrodesis in poor surgical candidates (FIG 6).6
For the neuropathic patient in whom bracing can achieve a relatively plantigrade posture for the hindfoot and ankle, we prescribe a double metal upright AFO attached to an Oxford shoe that includes Plastazote liners (total contact inserts).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree