Tibial Shaft Fractures: Intramedullary Nailing
Daniel S. Horwitz
Erik Noble Kubiak
INTRODUCTION
Tibial shaft fractures encompass a spectrum of injuries ranging from low-energy closed fractures to limb-threatening open fractures. Intramedullary nailing is the treatment of choice for most displaced fractures in the middle three-fifths of the tibia. Contemporary tibial nailing is performed with minimal medullary reaming using cannulated locking nails for both closed and open fractures. Recent prospective studies have shown that reaming is not associated with a statistically significant increase in infection rates for most open fractures (1, 2 and 3). Solid nails have largely been abandoned due to their inability to reduce the infection rate and difficulty with insertion and removal.
The favorable mechanical and biologic characteristics of intramedullary nails as well as advances in nail design have expanded the indications for nailing to include more proximal and distal tibial fractures. However, nailing of proximal tibial fractures with conventional entry portals often leads to angular deformities. To minimize malalignment following nailing, both a change in the approach (infrapatellar vs. suprapatellar) and the position of the leg (flexed or extended) is required. Another recent technical advance in nailing is the introduction of angular stable locking bolts or screws. This may improve stability following nailing in very proximal or distal fractures, particularly in osteoporotic bone.
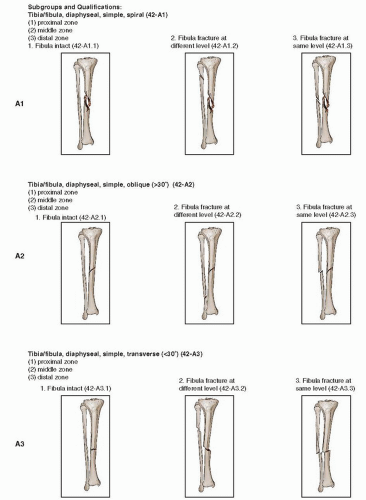
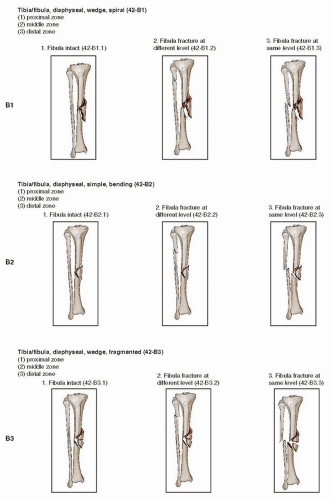
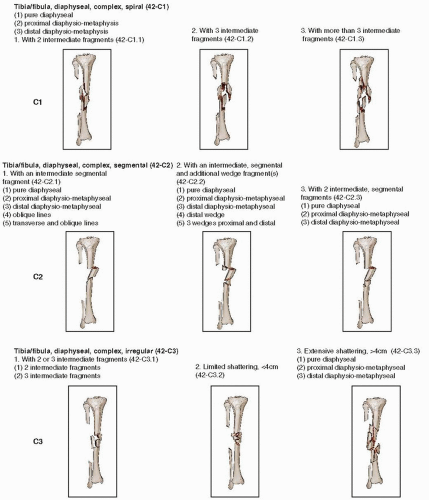
There are several widely used classifications for tibial fractures. The Gustillo and Andersen, as well as the Tscherne classifications, are used to describe soft-tissue injury patterns associated with both closed and open tibial fractures. The AO/OTA fracture classification of tibia fractures is a morphologic or geometric tool to describe the location and pattern of bony injury (Fig. 29.1).
INDICATIONS AND CONTRAINDICATIONS
Numerous studies have shown satisfactory rates of healing and earlier weight bearing compared to other fixation techniques when using an intramedullary nail. However, the advantages with this method of treatment must be carefully weighed against the risks unique to tibial nailing such as chronic knee pain and infection. Contraindications to nailing include patients who have isolated low-energy fractures with minimal shortening, displacement, or angulation that can be treated in a cast. Sarmiento and others have shown that shortening up to 12 mm and angulation up to 5 degrees in the frontal plane and 7 degrees in the sagittal plane are associated with good outcomes following functional bracing (4,5). Nonoperative treatment of high-energy fractures with substantial shortening, displacement, and angulation, particularly when there is associated soft-tissue injury, makes cast or brace treatment inadvisable. Nailing is also contraindicated in young adolescents with open epiphysis and in adults with very small medullary canals (<7 mm). The use of intramedullary nails in patients with infected fractures and nonunions is controversial, and alternative fixation techniques are often more appropriate in these patients.
Strong indications for intramedullary nailing include closed or open, displaced, and/or unstable fractures in the middle three-fifths of the tibia that are not amenable to cast or brace treatment. Some tibial fractures with an intact fibula can be difficult to reduce and hold in a cast and are better treated with an intramedullary nail. Other strong indications for nailing are tibial fractures with complex ipsilateral injuries to the foot, ankle, knee, or femur. Multiply injured patients with contralateral limb injuries and selected patients with pelvic, spine, and upper extremity fractures usually benefit from surgical stabilization to improve mobilization of the patient and rehabilitation of their limb. Relative indications for nailing include tibial fractures associated with compartment syndromes or vascular injuries. In these cases, damage control orthopedics with initial external fixation followed by delayed nailing may be preferable.
The safety and efficacy of acute nailing of open tibial fractures has been evaluated in multiple prospective studies (1, 2 and 3,6). Randomized controlled trials have not shown a statistically increased risk of infection following acute primary nailing in these fractures. However, external fixation may be preferred in patients with gross contamination, massive soft-tissue injury, extensive bone loss, or critically ill patients. In these challenging cases, delayed nailing or conversion to circular ring external fixation may be preferable.
While there have been several reports of intramedullary nailing of proximal tibia fractures (i.e., 4 to 6 cm from the joint), this remains a controversial topic (7,8). Specific reduction and nailing techniques are necessary in these cases to avoid malalignment or fracture instability. Unless a surgeon is familiar with the use of blocking screws, unicortical plating, and semiextended nailing methods, the use of a lateral locked plate should be considered. In some comminuted fracture patterns, nailing and supplemental medial plating may be indicated.
A similar thought process can be applied to very distal tibial shaft fractures when there is room for only a single distal interlocking screw. Unless the fracture is a simple pattern, and the fibula is either intact or can be axially stabilized, strong consideration should be given to the use of distal tibial anatomic plating.
PREOPERATIVE PLANNING
History and Physical Examination
Preoperative planning begins with a careful evaluation of the patient. A complete evaluation should include the Advanced Trauma Life Support protocols, obtaining a careful patient history and performing a detailed physical exam. The physical exam must evaluate and document the neurovascular status of the affected limb, the status of the compartments, and evaluation of active and passive toe motion. The soft-tissue envelope should be inspected for contusions, blisters, or open wounds. It is important to remember that a compartment syndrome is a clinical diagnosis, and pressure measurements are used primarily in borderline or questionable cases, and/or in patients with head injuries or cognitive impairment secondary to drugs or alcohol. Following a detailed assessment of the patient and his injury, the leg should be placed into a well-padded long leg splint prior to definitive management.
Imaging Studies
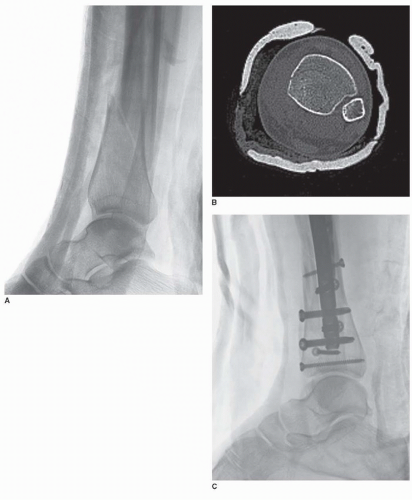
Radiographs must include full-length anteroposterior (AP) and lateral views of the affected tibia, and AP and lateral x-rays of the ipsilateral knee and ankle. Computed tomography (CT) scans of the knee or the ankle should be obtained when there is an intra-articular fracture extension or high index of suspicion of joint involvement based on the mechanism of injury or physical examination (Fig. 29.2).
TIMING OF SURGERY
Open Fracture Management
With open tibial fractures, high-dose intravenous antibiotics should be administered early. In Grade I, II, and IIIA open fractures, a cephalosporin antibiotic is given for 24 to 48 hours, and an aminoglycoside is added in Grade IIIB injuries. With farm injuries, penicillin is also administered. Tetanus toxoid should be given to all patients with an open tibial fracture.
The timing of operative treatment for open tibia fractures remains controversial. Whenever possible, surgical débridement should be done within 6 to 8 hours from the time of injury to lessen the risk of infection (9,10). Grossly contaminated wounds are irrigated in the emergency department if delays in treatment are anticipated.
Patients with open fractures that are physiologically stable and have no other contraindications to surgery can be safely nailed immediately following irrigation and débridement. Small clean wounds (<5 cm) are closed primarily, if this can be done without tension. Larger wounds are packed open, closed over a bead pouch, or covered with a wound vac. When there is deficient soft tissues, exposed hardware, or bone, microvascular surgery consultation is obtained. Rotational flaps or a free tissue transfer may be necessary.
Closed Fracture Management
Isolated closed unstable tibial shaft fractures should be splinted and have their tibia nailed within 24 to 48 hours whenever possible. In multiply injured patients, surgery is performed when the patient’s overall condition permits.
Surgical Tactics
The surgical setup includes a complete set of tibial nails and insertion equipment, medium and large-pointed reduction clamps, a large femoral distractor or external fixation tray, and small fragment screws. The small fragment set is useful to stabilize intra-articular extensions or when a unicortical plate or blocking screws are needed. Radiolucent triangles of different sizes are very helpful when performing classic medial or lateral patellar nailing with the knee flexed. The triangles also help reduce axial load and deforming forces on the tibial shaft itself, making reduction easier to maintain.
SURGERY
Anesthesia
We strongly recommend general anesthesia when treating patients with acute tibial fractures. It allows full-muscle paralysis for fracture reduction and allows careful postoperative monitoring for compartment syndrome. While spinal and regional anesthetic techniques are attractive for postoperative pain control, the small but real risk of masking a compartment syndrome makes this less appealing.
Positioning
Patients are placed supine on a radiolucent table that provides wide access for an image intensifier that is typically brought in from the opposite side. Fracture tables are rarely used when performing tibial nailing. A “bump” is placed beneath the ipsilateral flank and hip to maintain the leg in a neutral position. The arm on the affected side can be abducted on an arm board or placed and secured across the chest. A tourniquet is placed proximally on the thigh if there is concern for intraoperative bleeding—usually related to vascular or soft-tissue injuries.
Prep/Drape
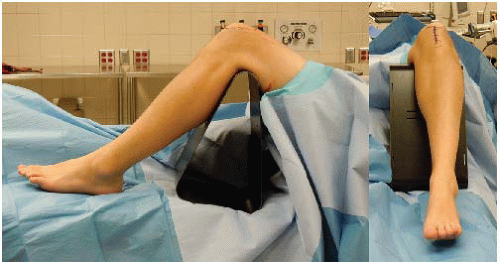
Although a thigh tourniquet is routinely applied, it is not frequently inflated. It is useful in patients with a vascular injury or significant bleeding associated with extensive soft-tissue injuries. We occasionally inflate the tourniquet during the irrigation and débridement, but NEVER during intramedullary reaming or nailing. We use an initial scrub with alcohol or chlorhexidine followed by an alcohol-based polymer product (Chloraprep/Duraprep). The entire leg is prepped, and the toes are wrapped with an impervious sticky plastic drape and left visible in the surgical field. Full access to the ankle and foot is essential to judge length, rotation, and alignment of the extremity. When using an extended nailing technique, the calf is supported with sterile bath blankets or a foam support beneath the drapes (Fig. 29.3).
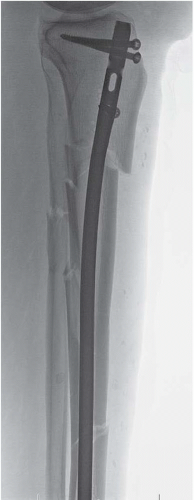
Nail Selection
We strongly recommend cannulated tibial nails designed to be placed over a guide wire. The bend in the nail should be very proximal rather than a long gradual curve, which can produce translational and angular deformities especially in proximal fractures (Fig. 29.4). The nail should accommodate proximal and distal locking screws that are at least 4 mm in diameter and are multiplanar. The ability to place locking screws in oblique planes is especially helpful when stabilizing metadiaphyseal fractures. Newer nail designs allow placement of angular stable (locked) screws, which may be desirable when treating metaphyseal fractures or fractures in osteoporotic patients.
Approach
There are several surgical approaches utilized when performing intramedullary tibial nailing, each with distinct advantages and disadvantages.
Medial tendon parapatellar. This is the most common starting point and is used for the majority of fractures in the middle and distal thirds of the tibia. However, it can lead to valgus malalignment when used to treat proximal tibial fractures.
Lateral tendon parapatellar. This approach aids in maintaining fracture reduction when nailing proximal one-third of fractures but requires mobilization of the patellar tendon.
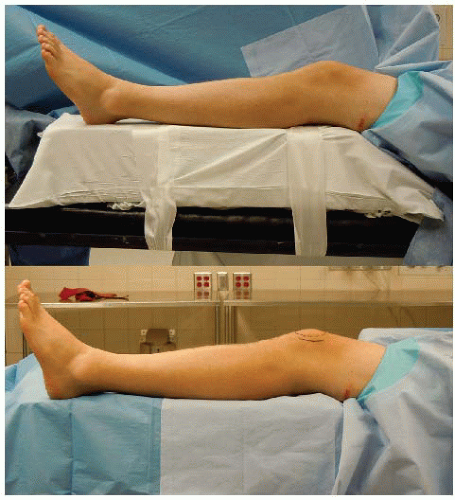
FIGURE 29.3 A foam support is used to facilitate the semiextended nailing technique. Note that the foam is secured to the table with surgical tape to avoid intraoperative motion or loss of support.
Patellar tendon splitting. This gives direct access to starting point, but can inadvertently damage the patellar tendon or lead to patella baja and is used less commonly.
Semiextended medial or lateral parapatellar. This approach is used to nail proximal tibial fractures. Advantages include ease of positioning, imaging, and aid to fracture reduction.
Suprapatellar (transquadriceps tendon). This is an alternative approach for proximal tibial nailing but requires special instruments. Inadvertent trochlear damage to the patella and femur is possible, and deposition of reaming debris in knee is a concern.
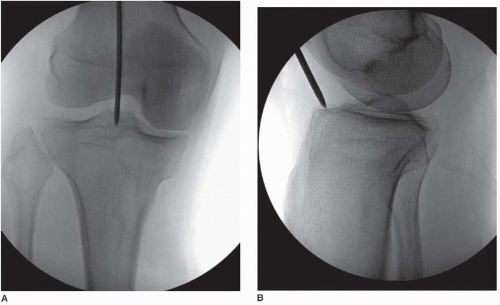
STARTING POINT
We describe the two most commonly used approaches when nailing a tibial fracture: the medial parapatellar tendon approach with the knee flexed (Fig. 29.5) and the lateral or medial parapatellar semiextended approach (Fig. 29.6). Both approaches utilize a similar starting point for nail insertion, which has been described as the “sweet spot,” referring to the flat extra-articular area just anterior to the joint and behind the patellar tendon (Fig. 29.7). This location has been well described in the literature (11) and is aligned with the lateral aspect of the medial tibial spine on the AP radiograph and just below the articular margin on the lateral view. When a parapatellar tendon approach is utilized, we prefer to remove soft tissues from the starting point using
electrocautery in order to clearly visualize the entry portal. Great care should be taken to avoid entering the joint or damaging the anterior aspects of the menisci. The starting point is localized and confirmed fluoroscopically with either an awl or with a guide pin that can be enlarged with a cannulated drill or awl. Care must be taken to avoid injury to the skin, meniscus, patella, and the cartilage of the femoral condyle during initial awl insertion and instrumentation of the tibia.
electrocautery in order to clearly visualize the entry portal. Great care should be taken to avoid entering the joint or damaging the anterior aspects of the menisci. The starting point is localized and confirmed fluoroscopically with either an awl or with a guide pin that can be enlarged with a cannulated drill or awl. Care must be taken to avoid injury to the skin, meniscus, patella, and the cartilage of the femoral condyle during initial awl insertion and instrumentation of the tibia.
For the medial parapatellar tendon approaches, a 3- to 4-cm skin incision is made between the inferior pole of the patellar and the tibial tubercle along the medial border of the patellar tendon. The extensor retinaculum is incised, and the sheath of the patellar tendon is identified, mobilized, and carefully preserved. The infrapatellar fat pad is freed from the posterior surface of the tendon, which leads to the bare area just below the knee joint.
The semiextended lateral or medial parapatellar approach utilizes a skin incision along the lateral or medial border of the patella, extending from the superior pole of the patella to the upper third of the patellar tendon, with the knee in relative extension (5 to 30-degree knee flexion). This approach can be made either medially or laterally, based on the patient’s anatomy and which direction allows better access to the proximal tibia. For example, if the patella naturally subluxes more easily to the medial side (more common), then the lateral parapatellar approach is chosen. Through a 3- to 4-cm skin incision, the retinaculum and joint capsule are opened to the level of the synovium, which should be kept intact. This allows the patella to be mobilized medially or laterally without difficulty. The synovium is a thin layer and can be easily torn by insertion instruments or reamers. If this occurs, it is carefully repaired with a 2-0 absorbable suture at the end of the case. The retropatellar fat pad is freed from the posterior surface of the patellar tendon revealing the bare area of the proximal tibia for nail entry. When using this approach, the bare area is palpated and visualized with fluoroscopy, but is not generally visualized by the surgeon. When using the semiextended approach, the surgeon must be vigilant to avoid anterior migration of the proximal starting point, intermeniscal ligament injury, and damage to the articular surface of the knee during the approach, reaming, and instrumentation of the tibia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree