Tibial Pilon Fractures: Tensioned Wire Circular Fixation
James J. Hutson Jr.
INTRODUCTION
Circular tensioned wire fixation of periarticular fractures of the distal tibia is a well-established method of treatment to manage selected pilon fractures as an alternative to internal fixation. Circular external fixation with tensioned wires aligns and stabilizes these difficult and high-risk fractures with minimal additional soft-tissue injury and few major complications. The chief advantage with this method of treatment is that it avoids the soft-tissue dissection in the zone of injury required to place plates. Furthermore, the extensive metallic surfaces inherent with internal fixation may increase the risk of bacterial colonization and subsequent infection. Despite the advent of locked plating and “minimally invasive” surgical techniques, internal fixation of high-energy pilon fractures is still associated with substantial risk. Increasing levels of soft-tissue damage, comminution of the distal tibia, and bone loss create a zone of injury, which makes external fixation an attractive treatment alternative. This chapter provides a comprehensive technique guide for application of circular fixation of pilon fractures ranging from fixation of extra-articular distal tibial fractures to complex articular injuries with bone loss. A bridging frame with limited internal fixation is a technique that surgeons with limited experience with circular ring frames can learn to apply. For surgeons who treat complex pilon fractures not amendable to plating, the technical drawings provided in this chapter may serve as a guide to address fractures with severe comminution, bone loss, and complex soft-tissue injuries.
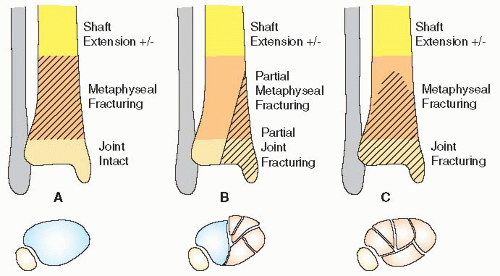
The Orthopedic Trauma Association’s Fracture Compendium that describes fractures in the distal tibia is seen in Figure 32.1. Type A injuries are extra-articular fractures that spare the joint. Type B fractures are partial articular injuries with an osteoarticular segment of the joint still intact and connected to the shaft. Type C fractures involve the joint surface and adjacent metaphysis. They are further divided into three subtypes based on the severity of articular and metaphyseal comminution. A C1 injury has a simple split, while C2 and C3 fractures have increasingly complex joint disruption.
INDICATIONS AND CONTRAINDICATIONS
For many lower-energy injuries and in patients with a good soft-tissue envelope, internal fixation with low-profile locking plates inserted using minimally invasive techniques is an attractive method of treatment. For example, partial articular injuries (Type B) with an intact column of bone that maintains length are ideal for buttress plating with low-profile plates. For many Type A and C1, fractures with mild to moderate soft-tissue injury can also be treated with internal fixation or half-pin bridging frames with limited internal fixation.
However, as soft-tissue damage and bone comminution worsen, the indications to use circular tensioned wires increase (1). Circular tensioned wire fixators are dynamic devices that allow the surgeon the ability to fabricate a customized external fixator to treat complex distal tibial periarticular fractures. The fixators are
constructed based on the position of the fracture fragments and the severity of injury to the soft tissues. Basic principles are applied in sequence, which results in alignment and fixation of the fracture.
constructed based on the position of the fracture fragments and the severity of injury to the soft tissues. Basic principles are applied in sequence, which results in alignment and fixation of the fracture.
Strong indications for circular tensioned wire external fixation of distal tibia periarticular fractures include
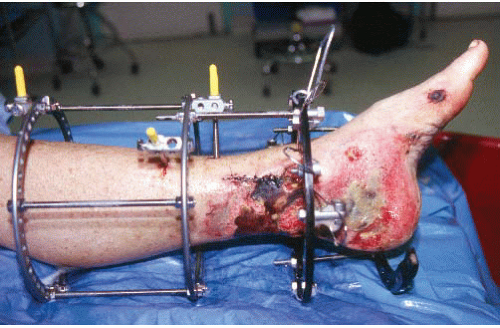
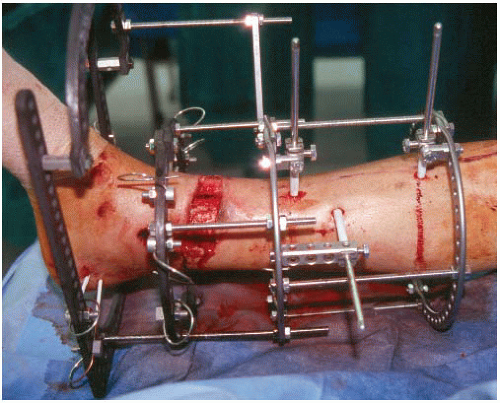
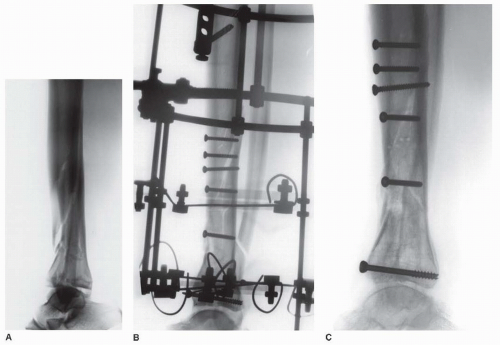
Grade II and III open fractures with soft-tissue injuries that would compromise an open approach for internal fixation (Fig. 32.2). The most common is a large medial wound with partial edge necrosis that could not be closed without a free flap (Fig. 32.3).
Closed fractures with soft-tissue injuries that would compromise an open approach for internal fixation
Complex fractures with severe comminution in which the fragments are too small to be fixed with locking screws
Pilon fractures with bone loss (Fig. 32.4)
Pilon fractures with late presentation (>3 to 4 weeks)
Relative Indications
Pilon fractures with diaphyseal extension (Fig. 32.5).
Segmental tibial fractures
Patients with other fractures in the lower or upper extremity fractures that would enable mobilization and earlier weight bearing
Obese patients who are unable to remain nonweight bearing for 3 months after plating
Pilon fractures associate with complex foot injuries
Psychiatric patients who will walk on their extremity against advice.
Patients with ischemic vascular disease/diabetes with tenuous skin that would not tolerate open incisions and skin distraction necessary to place large locking plates
PREOPERATIVE EVALUATION AND PLANNING
History and Examination
Distal tibial periarticular fractures often occur in patients with other injuries. Multiply injured patients must be evaluated for life and limb-threatening injuries using advanced trauma life support protocols. When the patient is stable, the patient and his or her extremity are evaluated in detail. In the conscious patient, the mechanism of
injury should be determined. This often gives important information about the amount of energy absorbed by the limb and its impact on the soft tissues. The patient’s medical history should review important comorbidities such as diabetes or peripheral vascular disease. Does the patient use alcohol or smoke tobacco? Is there a history of mental illness? Is the patient employed? Does the patient have family support and financial resources for a prolonged period of disability? These factors may influence the treatment recommendations.
injury should be determined. This often gives important information about the amount of energy absorbed by the limb and its impact on the soft tissues. The patient’s medical history should review important comorbidities such as diabetes or peripheral vascular disease. Does the patient use alcohol or smoke tobacco? Is there a history of mental illness? Is the patient employed? Does the patient have family support and financial resources for a prolonged period of disability? These factors may influence the treatment recommendations.
On physical exam, the entire limb from hip to toes should be exposed, inspected, and examined for signs of injury. The soft-tissue envelope of the distal one half of the tibia should be carefully evaluated for abrasions, blisters, or open wounds. In patients with skeletal deformity, gentle traction to grossly realign the limb should be performed and the extremity supported. The dorsalis pedis and posterior tibial pulse are palpated. If undetectable or asymmetric with the opposite side, a Doppler examination is performed. If there is compromise to the circulation of the leg, consultation with vascular surgery is indicated. The lower leg and foot are evaluated for compartment syndromes, which do occur but are seen less commonly than in patients with high-energy tibial shaft fractures. A detailed neurologic exam with specific testing of deep and superficial peroneal, medial, lateral and calcaneal plantar nerves, saphenous, and sural nerve function is recorded. It is essential to have an accurate neurologic and vascular exam before surgery. If the patient has a postoperative loss of sensory, motor, or vascular function, comparison with the preoperative evaluation is critical. Open wounds are observed for extent of injury and degree of contamination. In patients with open fractures, intravenous cephalosporin or vancomycin antibiotics are started immediately. Wounds with gross soil contamination receive additional antibiotics that cover gram-negative organisms. With sterile gloves, the wound is lavaged with normal saline, and a sterile dressing and splint are applied.
Imaging Studies
Essential radiographs include an anteroposterior (AP), lateral, and mortise view of the ankle, as well as full-length films of the entire tibia. Dedicated x-rays of the foot should also be obtained. For the vast majority of
pilon fractures, a computed tomography (CT) scan is obtained. It is an important adjunctive imaging study; however, the scan should be delayed until the fracture has been preliminarily reduced and stabilized. If the scan is acquired before the fracture is reduced, it is of little value. The scan defines the size and location of the fracture fragments available for fixation. The orientation of the fragments, displacement of the joint surface, and potential fixation pathways will be derived from the CT scan.
pilon fractures, a computed tomography (CT) scan is obtained. It is an important adjunctive imaging study; however, the scan should be delayed until the fracture has been preliminarily reduced and stabilized. If the scan is acquired before the fracture is reduced, it is of little value. The scan defines the size and location of the fracture fragments available for fixation. The orientation of the fragments, displacement of the joint surface, and potential fixation pathways will be derived from the CT scan.
Surgical Tactic
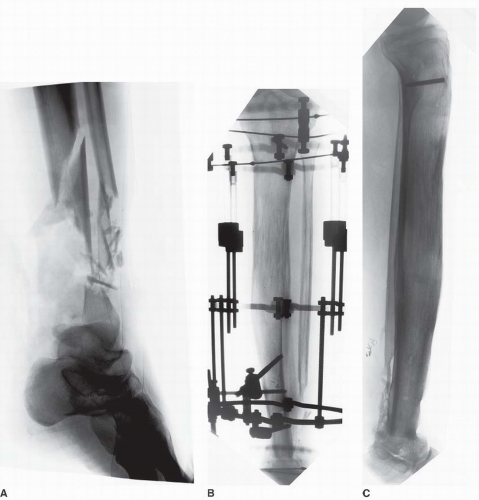
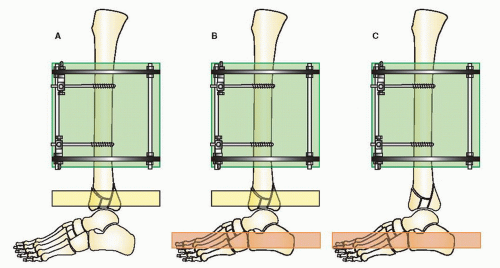
Lower-energy closed fractures are placed into a well-padded short leg or coaptation splint. Open fractures, fractures with vascular injuries, and patients with compartment syndrome require emergent surgery. Following irrigation and débridement or compartment release, the fracture is temporarily stabilized with half-pin bridging fixation using a transverse calcaneal pin and two half-pins in the tibia to create a delta frame (Fig. 32.6). Closed fractures with comminution and displacement also are stabilized with an early bridging halfpin external fixator. If these comminuted fractures are not reduced and stabilized early, massive edema and fracture blisters often occur. Calcaneal pin traction on a Bohler-Braun frame or traveling traction with a transfixation pin in the calcaneus and proximal tibia is an alternative if the patient cannot be taken to surgery (Fig. 32.7).
The goal of initial spanning fixation is to restore length and alignment of the fracture through distraction as well as to align the dome of the talus with the central axis of the tibia shaft on both the AP and lateral views. The second toe must be aligned with tibial tubercle to restore the correct rotational position of the extremity. The forefoot is controlled with a metatarsal pin, and the foot is aligned in a plantar neutral position. It is essential that excellent gross alignment be established with this initial bridging external fixation frame. However, it is important to remember that indirect reduction through ligamentotaxis cannot reduce impacted osteoarticular fragments. Failure to achieve these goals will compromise subsequent reconstruction. Repeat débridement, antibiotic bead pouches, or negative pressure dressings are frequently utilized in selected open fractures.
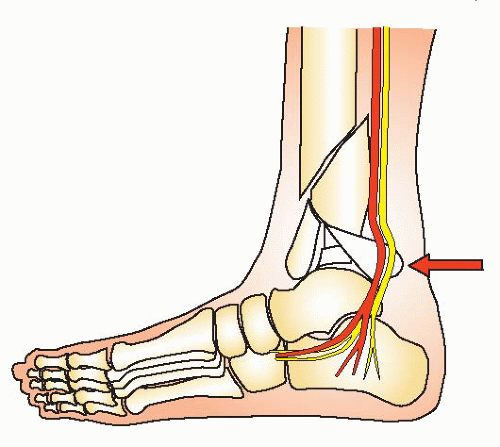
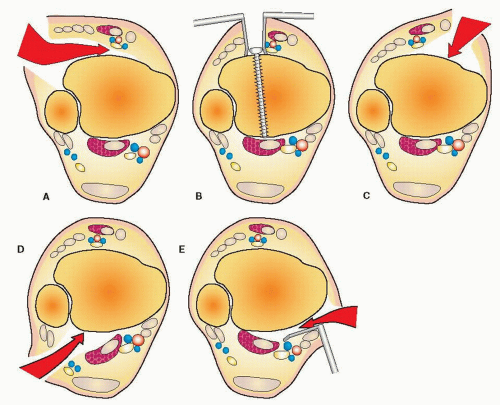
A number of fractures will have further soft-tissue compromise or wound problems requiring repeat operative débridement. Occasionally, a patient will have a fragment of the posterior tibia rotated and displaced against the tibial nerve resulting in parasthesia or anesthesia of the plantar surface of the foot (Fig. 32.8). Reduction of this fragment is urgently indicated to avoid permanent neurologic injury. A small number of Grade IIIB open fractures prove to have unreconstructable limbs necessitating amputation (2). I have found it helpful to engage the patient and family early in the course of treatment, particularly in severe cases involving limb salvage.
For the majority of closed and low-grade open fractures, improvement in the soft-tissue envelope occurs over 7 to 14 days. The status of the soft tissues determines the timing of definitive reconstruction of a pilon fracture. When the edema has improved, the fracture blisters begin to reepithelialize, and the skin wrinkles return, second-stage surgery can proceed.
Staged Reconstruction
Postreduction plain films and the CT scan are critically evaluated. The integrity of the lateral column is determined by the presence or absence of a fibular fracture. If the lateral malleolus is fractured, the level of fracture, amount of comminution, and separation of the fibula from the tibia are noted. The proximal extension of the tibia fracture and comminution of the joint surface is evaluated. Fracture comminution and bone loss are evaluated. The axial cuts on the CT scan help identify the ideal location for an incision if an open approach is needed. A pilon fracture can be approached through anterior-medial, anterior-lateral, posterior-lateral, or posteriormedial soft tissues based on the CT “windows” (Fig. 32.9). The condition of the soft tissues will be compared to the fracture pattern to avoid an incision and dissection through compromised soft tissues. A decision is made at this time as to the plan of treatment (a) open reduction and internal fixation, (b) bridging external fixation with limited internal fixation, or (c) circular tensioned wire fixation. This chapter describes the treatment strategies for tensioned wire fixation.
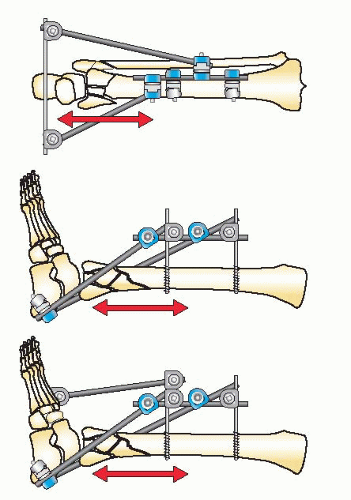
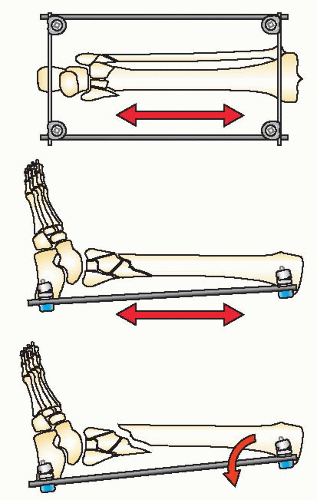
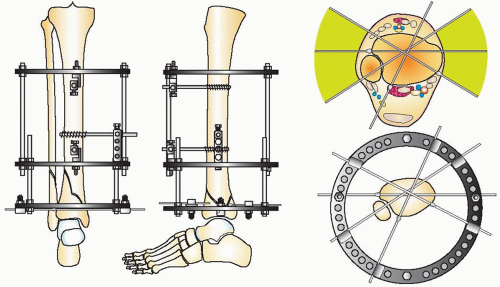
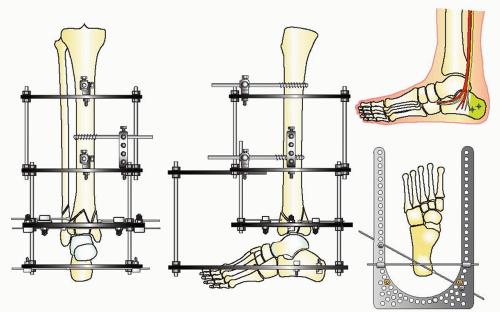
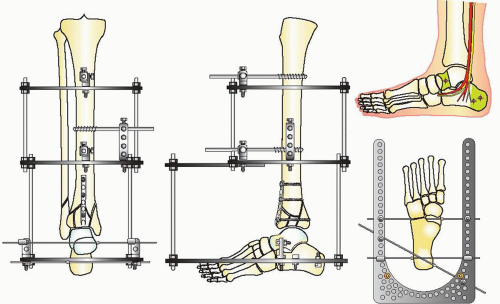
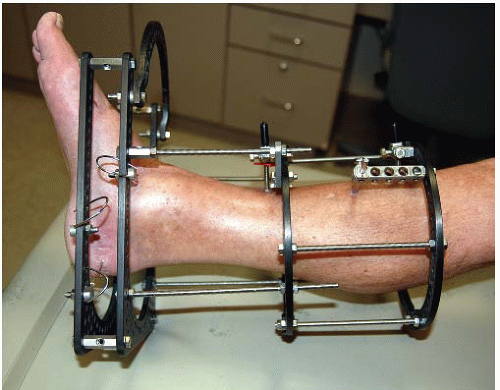
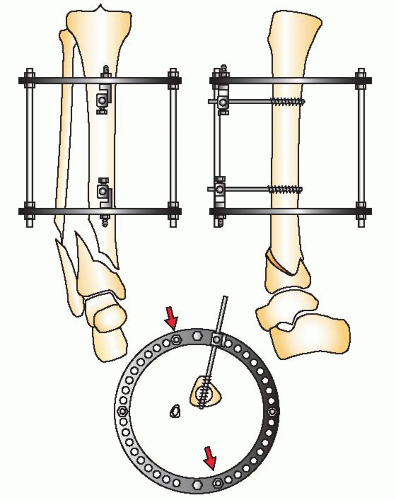
The goals of treatment in pilon fractures are to restore correct limb length, alignment, and rotation, reduce the joint surface to match the contour of the dome of the talus, and reconstruct the ankle mortise and metadiaphyseal bone. These goals are approached with cautious handling of the soft tissues. The strategy of reduction for this injury is based on distraction. Because of the terminal location of pilon fractures, the tibial shaft proximally is used as a fixation base to reduce the fracture. A fixation block is created with two half-pins in the AP plane in an orthogonal position when using circular fixators. This fixation block is used as a base to support the distal fixation rings, which are placed at the level of the plafond or calcaneus to distract and reduce the fracture. The reduction of the fracture is initiated with application of a double-ring fixation block on the tibial shaft (Fig. 32.10). Distal fixation is determined by the configuration of the fracture and the soft-tissue injury. Type A, C1, and C2 fractures with large fracture fragments are reconstructed with a fracture reduction ring at the level of the tibial plafond (Fig. 32.11). If there is comminution of the joint, the frame will combine a distraction foot plate (ring) and a plafond fracture reduction ring (Fig. 32.12). Pilon fractures amendable to limited internal fixation and bridging distraction will have a foot plate (ring) applied to the calcaneus and talar neck without a ring at the level of the plafond (Figs. 32.13 and 32.14).
Distraction is the key to reduction. If the plafond or calcaneus (hindfoot) is distracted axially with correct rotation, the distal tibial fracture will be spatially reduced with correct rotation, alignment, and length. This initial reduction will facilitate the local alignment of the joint surface and the metaphysis by percutaneous or open techniques. The better the alignment gained by accurate distraction, the easier the reduction of the joint and metaphysis. It is almost impossible in complex pilon fractures to reduce the plafond if the dome of the talus is malaligned, shortened, or rotated. This applies to any type of external fixator used to treat pilon fractures (monolateral, clamp and rods, and circular tensioned fixators). The dome of the talus must be aligned correctly in distraction before beginning the reduction of the fracture fragments.
Anesthesia, Positioning, Imaging
General anesthesia is preferred. Postoperative nerve evaluation and the small chance of compartment syndrome are relative contraindications to spinal anesthesia or regional nerve blocks. The patient is positioned on a fluoroscopic flat-top table that allows easy access for a C-arm image intensifier, which is positioned on the opposite side from the injured leg. A silicone bolster is placed under the buttock and flank to internally rotate the leg to neutral. A tourniquet is placed on the thigh. Intravenous cefazolin or vancomycin is administered at least 1 hour before surgery. A foley catheter is placed as surgery often takes 3 to 6 hours.
The original or resuscitation fixator is removed before prepping. The resuscitation pins are never used for the definitive fixator. Manual traction is maintained during the prep and drape to prevent angular displacement of the fracture. The leg is scrubbed with soap and sterile water, and the pin sites are cleaned to remove dried skin and debris. A formal prep and drape from tourniquet to toes is completed. It is essential to have the knee completely exposed in the field to assess rotation of the fracture and limb. The rotation of the knee that centers the patella image between the condyles is considered the AP alignment of the knee.
REDUCTION TECHNIQUE TYPE A AND TYPE C1 AND C2 FRACTURES
The level of the distal horizontal reference wire is determined by the fracture pattern. In Type A distal tibia fractures, the joint surface is intact, while in some C1 and C2 fracture patterns, the articular fracture contains large fragments. If a percutaneous or limited open reduction and fixation with subchondral lag screws will reduce the joint surface anatomically and create a solid epimetaphyseal bone block, it is strongly recommended. The reconstructed distal tibia can then be treated as a Type A fracture (Fig. 32.15).
The proximal ring block is aligned on the tibial shaft with two AP 5- or 6-mm half-pins (Fig. 32.16). Hydroxyapatite-coated pins are always used because they bond to the bone reducing the incidence of pin track infection. There should be at least 10 cm of spread between the half-pins to increase the fixator stiffness. Mounting these pins with a Rancho Cube (Smith Nephew) facilitates alignment of the frame (Fig. 32.17). The pins should be placed with their tips protruding just beyond the opposite cortex (Fig. 32.18). The distal halfpin is placed 3 cm above the proximal extent of the fracture. Placing the half-pins distant from the fracture increases the working length leading to frame instability. It is important to align the fixation block in an orthogonal position. The frame should be parallel to the tibia on the AP and lateral views. The ring over the plafond must clear the anterior soft tissues of the ankle, and the superior ring of the fixator block must not impinge on the posterior leg, where the gastronemius and soleus muscles bulge posteriorly (Fig. 32.19).
If the fixation block on the tibia is orthogonal, then the joint surface of the plafond will be in anatomic alignment when the joint forms a 90-degree (±2 degree) angle with the axis of the shaft. The joint line on the AP view forms an angle of 90 degrees to the axis of the tibia. This anatomic fact allows the surgeon to accurately align distal tibia fractures by placing a horizontal reference wire parallel to the epiphyseal scar and joint surface. The horizontal reference wire is placed 10 mm above the plafond centered on the metaphysis in the lateral view (Fig. 32.20). The centered lateral view is used to place the reference wire (Fig. 32.21). This places the pin outside of the joint capsule and prevents intra-articular pin placement (Figs. 32.22 and 32.23) (3,4). The plane of the carbon fiber fracture reduction ring, which is connected to the proximal tibial ring, is 90 degrees to the shaft. The horizontal reference wire in the distal tibia is attached to the distal side of a radiolucent carbon fiber fracture ring and then manipulated under fluoroscopy to align the plafond axially and with correct rotation (Fig. 32.24). The horizontal reference wire may need to be adjusted several times until an anatomic alignment is obtained (Fig. 32.25). Small angular corrections are done with washers on one side of the ring to improve alignment when needed (Fig. 32.26). Once the wire is tensioned, distraction is placed across the fracture to reduce the metaphysis.
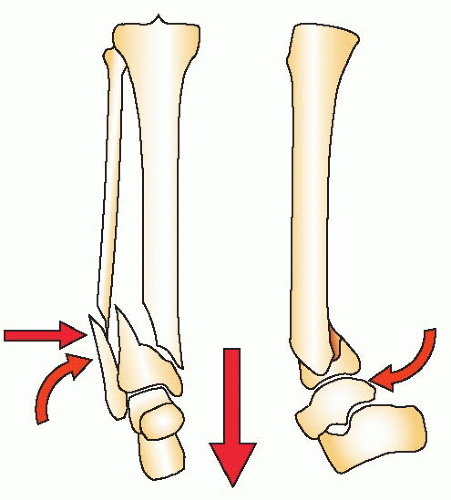 FIGURE 32.15 A Type A distal tibia fracture. Reduction is gained by distraction to length, correction of rotation, and axial alignment. |
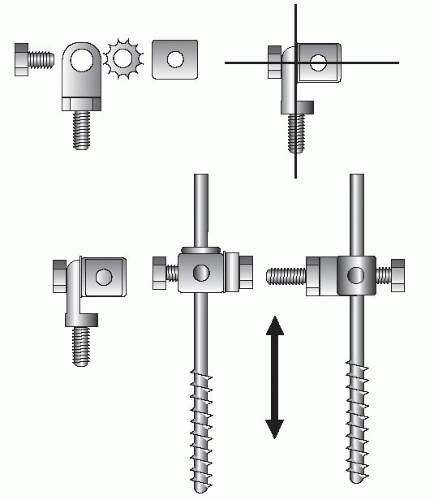 FIGURE 32.17 The half-pins are connected to the rings on the stable base with universal fixation cubes. An 8-mm bolt connects the Rancho Cube® (Smith Nephew) to a male hinge or post. These universal attachments allow fine-tuning of the stable base and small corrections of the tibial shaft alignment with the plafond.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|