Tibial Pilon Fractures: Staged Internal Fixation
David P. Barei
Daphne M. Beingessner
INTRODUCTION
Pilon fractures continue to be challenging injuries due to their associated and often complex osseous and soft-tissue injury components. Pilon fracture is a mechanistic term that is commonly applied to injuries of the tibial plafond and describes an axial-loading injury similar to the interaction of a mortar and pestle. The energy absorbed in these injuries often causes significant osseous comminution, fracture displacement, and axial shortening. This, in turn, results in the significant swelling, abrading, and blistering of the surrounding soft-tissue envelope (Fig. 31.1).
These fractures are typically the result of higher-energy mechanisms such as falls from a height, motor vehicle collisions, motorcycle crashes, or industrial accidents in younger patients. They also may occur as the result of lower-energy torsional injuries. Both groups may have significant soft-tissue compromise. A spectrum of injury exists, but the combination of axial and rotational force is universal and results in a variety of fracture patterns depending on the direction of force and position of the foot and ankle at the time of load application.
A variety of associated injuries may accompany pilon fractures. Some series have reported up to 51% of patients with other fractures or major system injuries. The rate of open injuries has been reported to be as high as 56%. However, compartmental syndrome is relatively uncommon with reported rates of up to 5%. Vascular injury at a rate as high as 52% may occur but typically involves only one vessel and the patients are not clinically ischemic.
The AO/OTA classification system incorporates all fractures of the distal tibia including extra-articular fractures of the distal tibial metaphysis. Tibial plafond fractures are categorized as extra-articular (43 Type A), partial articular (43 Type B), or total articular (43 Type C). Each type is then further divided into one of three groups depending on the amount of fracture comminution. Subgroups are identified by other characteristics of the fracture, such as the direction, description, or location of a fracture line, the presence of metaphyseal impaction, and the location and amount of comminution. Although the system can be unwieldy with 27 separate injuries described, for the purposes of developing a surgical tactic, the authors find it useful to group the fractures according to the AO/OTA system.
Ruedi and Allgower’s seminal English language article in 1969 described a principled technique for ORIF of the tibial plafond that demonstrated a substantial improvement in functional outcome, complications from arthrosis, and a minimal treatment complication rate compared to nonoperative management. This landmark article would become the benchmark for the treatment of these injuries with only 3 of 84 consecutive patients that developed a deep-wound infection. Subsequent to this publication, the history of open reduction and plate fixation of tibial plafond fractures in North America demonstrated a high rate of deep-wound infection and complications with associated poor outcomes. At least two major differences can be identified between Ruedi’s study and subsequent studies with higher complication rates noted: (a) the time delay from injury to definitive surgery and (b) the mechanism of injury. Though infrequently noted, 75% of Ruedi’s patients were definitively managed surgically on the day of their injury. Fourteen patients were delayed for over 7 days secondary to “severe swelling or doubtful skin conditions,” and the remaining six patients had been treated initially with casting elsewhere but the exact time to their definitive procedure was not indicated. Furthermore, of the 84 fractures in Ruedi’s manuscript, 60 fractures (71%) occurred from skiing injuries, 19 fractures (23%) occurred
from a fall between 3 and 12 feet, and only 5 fractures (6%) occurred from higher-energy traffic accidents. Comparatively, the subsequent North American literature describes a time delay between injury and definitive treatment between 3 and 6 days. Additionally, a greater proportion of these patients sustained their injuries from higher-energy motor vehicle collisions or other industrialized mechanisms. While other variables may also be responsible for the differences in outcomes and complications, the difference in timing and injury mechanisms remain key differences and have shaped the evolution of tibial pilon fracture care over the past 30 years.
from a fall between 3 and 12 feet, and only 5 fractures (6%) occurred from higher-energy traffic accidents. Comparatively, the subsequent North American literature describes a time delay between injury and definitive treatment between 3 and 6 days. Additionally, a greater proportion of these patients sustained their injuries from higher-energy motor vehicle collisions or other industrialized mechanisms. While other variables may also be responsible for the differences in outcomes and complications, the difference in timing and injury mechanisms remain key differences and have shaped the evolution of tibial pilon fracture care over the past 30 years.
Because of the problematic soft-tissue complications that became evident with open reduction and internal fixation (ORIF), the optimal treatment for these injuries was reassessed and the development of staged ORIF was developed. Specifically, this entails performing definitive ORIF only after a period of soft-tissue recovery. Two separate reports by Sirkin and colleagues and Patterson and Cole in 1999 have led to its popularization and concluded that the historically high rates of infection associated with ORIF of pilon fractures may have been due to attempts at immediate fixation through swollen and compromised soft tissues.
There is still no consensus on the optimal treatment for these injuries; however, staged ORIF of high-energy tibial pilon fractures has decreased wound complication rates commensurate with those seen in the initial Ruedi and Allgower’s work. Overall, a deep-wound sepsis rate of approximately 2% to 5% for closed fractures is a reasonable estimate, with higher rates likely in open fractures. Staged treatment requires the early application of at least a spanning external fixator with or without fibular fixation. Key points for successful treatment are the restoration of limb alignment, length, and rotation and placement of external fixator pins well outside the area of surgical exposure or anticipated definitive implants. This strategy allows for more extensive approaches for internal fixation in order to optimize articular reduction while decreasing the likelihood of soft-tissue compromise. In addition, advances in minimally invasive-plating techniques, development, and familiarity of alternate exposures and the availability of low-profile anatomic plates have given the surgeon more tools to address these challenging injuries.
INDICATIONS AND CONTRAINDICATIONS
The vast majority of displaced pilon fractures should be treated with internal or external fixation with very limited indications for nonoperative treatment. In displaced and comminuted fractures, nonoperative treatment often leads to a malunion and occasionally a nonunion. However, some completely nondisplaced fractures may be treated nonoperatively with cast immobilization until radiographic signs of union are present. This treatment is followed with progressive weight bearing in a removable cast boot. In patients with significant medical comorbidities who cannot tolerate surgery or in those that are bedridden or nonambulatory, a closed manipulative reduction may be performed followed by cast immobilization. Alternatively, in those patients with significant shortening, calcaneal traction for a short period of time (<2 weeks) followed by casting may be performed.
Displaced pilon fractures are typically treated operatively. Although the optimal treatment method has not been determined, there is general consensus that restoration of alignment and articular congruity and correction of talar subluxation will improve outcomes.
PREOPERATIVE PLANNING
History and Physical
A complete history of the injury should be obtained. Understanding the mechanism of injury helps to determine the presence of associated injuries as well as the anticipated soft-tissue disruption associated with the pilon fracture. Other important factors include medical comorbidities, nicotine use, employment and hobbies, location, and timing of the injury, as well as any preexisting ankle joint conditions. Since these injuries are often
the result of an axial load, a complete musculoskeletal survey must be completed to assess for other extremity fractures, spine, or pelvic injuries. Focused physical examination of the affected extremity should include assessment of the soft tissues. The presence of abrasions, open wounds, fracture blisters, contusions, skin tenting, and swelling should be noted. Gross deformities should be realigned during the physical examination. Pulses should be documented as well as a complete peripheral nerve examination of the tibial and peroneal (superficial and deep) nerves in both their sensory and motor distributions.
the result of an axial load, a complete musculoskeletal survey must be completed to assess for other extremity fractures, spine, or pelvic injuries. Focused physical examination of the affected extremity should include assessment of the soft tissues. The presence of abrasions, open wounds, fracture blisters, contusions, skin tenting, and swelling should be noted. Gross deformities should be realigned during the physical examination. Pulses should be documented as well as a complete peripheral nerve examination of the tibial and peroneal (superficial and deep) nerves in both their sensory and motor distributions.
Imaging Studies
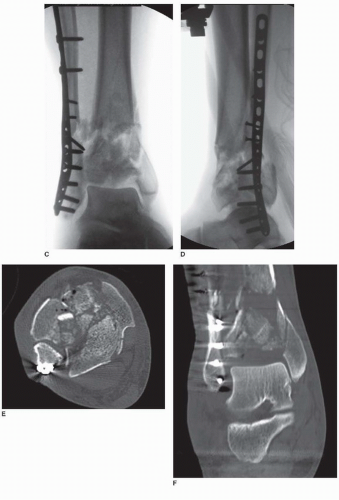
Radiographic evaluation of pilon fractures includes standard anteroposterior (AP), mortise, and lateral images. Full-length radiographs of the tibia and fibula should also be included to evaluate for more proximal injuries. Computed tomography (CT) with sagittal and coronal reformations provides more detail of fracture orientation to allow for accurate preoperative planning. CT scanning, however, should be deferred until after a provisional reduction (i.e., external fixator with or without fibular fixation) has occurred as it will provide more accurate information about the fracture configuration (Fig. 31.2). If the plain radiographs demonstrate a relatively simple fracture pattern without significant shortening in a patient with a minimal softtissue injury, acute CT scanning is appropriate to plan for definite operative fixation.
Timing of Surgery
There is a wide spectrum of presentations of pilon fracture, and surgical timing must be tailored to each individual case. The key factor in determining timing of surgery is the condition of the soft-tissue envelope. Open fractures should be treated emergently with irrigation and débridement followed by spanning external fixation or definitive fixation. While not every tibial plafond fracture requires staged treatment, the authors have found this treatment strategy to be successful in the management of the large majority of these injuries. Accordingly, if the patient is going to be treated with staged ORIF, reestablishing limb length and alignment, and relieving the skin of any areas of pressure should be done within the first 24 to 48 hours after appropriate medical clearance has been obtained. The second stage is then performed when the swelling has sufficiently resolved, usually 1 to 2 weeks after the index procedure. The soft tissues at this point will demonstrate skin wrinkles, loss of “shininess,” reepithelialization of fracture blisters, and a general pliability to the soft-tissue envelope.
SURGERY: STAGED OPEN REDUCTION AND INTERNAL FIXATION
The authors treat the majority tibial plafond fractures with staged ORIF using the general principles outlined by Ruedi and Allgower four decades ago. The goals are anatomic articular reduction and anatomic restoration of length, alignment, and rotation of the distal tibia. Conceptually, pure isolated medial buttress plating, as originally described by Ruedi and Allgower, is less important as choosing an implant, or implants, that are appropriate to support the anticipated loads that the articular and diaphyseal fracture components may encounter. This treatment method requires close attention to the creation of a surgical tactic at each intervention. Failure to do so may compromise the final result and increase the risk of complications.
Stage 1: Fibular ORIF and Spanning Tibiotalar External Fixation
The goal of the initial operative stage is on the reduction and stabilization of the osseous component of the fracture, particularly restoration of limb length, alignment, and rotation, but primarily as it relates to its effects on soft-tissue stabilization. Specifically, this means the elimination of skin tenting, soft-tissue distortion, areas of ischemia from displaced osseous fragments, and restoration of soft-tissue length. This first stage is typically performed urgently as soon as the patient’s general condition permits. Critical elements of this stage include the accurate placement of skin incisions, external pin placement, anticipation of where definitive tibial surgical
incisions and implants will be placed, and the execution of optimal reduction of the fibula and tibial fractures. It is the authors’ opinion that, if possible, the surgeon performing the initial stage should also perform the definitive stage or share a similar management philosophy. Decisions and treatments that occur during this initial stage can have significant impact on the final result. Furthermore, one should not be lulled into the assumption that this stage is “simple” or only “provisional.”
incisions and implants will be placed, and the execution of optimal reduction of the fibula and tibial fractures. It is the authors’ opinion that, if possible, the surgeon performing the initial stage should also perform the definitive stage or share a similar management philosophy. Decisions and treatments that occur during this initial stage can have significant impact on the final result. Furthermore, one should not be lulled into the assumption that this stage is “simple” or only “provisional.”
Preoperative Planning
The key features of this stage include the anticipation of all skin incisions (for this and later stages), débridement of any open wounds, ORIF of an associated fibular fracture, and closed manipulative reduction and temporary spanning external fixation of the tibial plafond fracture. Close evaluation of the injury radiographs will help determine whether an associated fibula fracture failed predominantly in compression, tension, or rotation and aid in selecting optimal fibular fixation. It is infrequent that anything beyond fibular fixation and tibiotalar spanning external fixation is performed in the first stage, but there are some exceptions. In a small subset of tibial plafond-fracture patterns, extension of the fracture may propagate into the diaphysis. Occasionally, acute reduction and stabilization of this fracture component during the initial stage may facilitate the subsequent stage of definitive articular and axial reductions and fixations (Fig. 31.3). Similarly, widely displaced or rotated posterolateral Volkmann fragments may also be addressed during the initial stage. While this is an infrequent occurrence, a careful preoperative plan will allow the fibula fracture and posterolateral Volkmann fragment to be addressed via the same posterolateral skin incision. It is imperative, however, that the surgeon refrain from overzealous open tibial reductions during this initial stage.
Positioning and Draping
The patient is placed supine on a radiolucent operating table. A soft supportive bump or roll is placed beneath the ipsilateral buttock, flank, and shoulder region to minimize the tendency for the entire limb to externally rotate. A sturdy foam ramp or pillow is placed beneath the injured extremity to slightly flex the ipsilateral hip and knee and elevate the leg, thereby allowing easier access to the posterolateral aspect of the fibula and to allow unobstructed lateral fluoroscopic imaging of the foot, ankle, and tibia. The ipsilateral arm is placed across the chest to avoid a traction injury to the brachial plexus. All bony prominences should be padded, particularly the fibular head and lateral malleolar regions of the contralateral leg. A tourniquet is rarely used for this procedure.
The leg is shaved, aseptically prepared, and free-draped to the mid-thigh. A first-generation cephalosporin antibiotic is administered within 60 minutes of the surgical incision. The image intensifier is brought in from the contralateral side of table. When performing operative fixation of the fibula, the monitor is best viewed when it is located at the foot of the bed. During the application of external fixation, particularly when applying traction to the foot, the monitor is best positioned closer to the head of the bed.
Approach
FIBULA
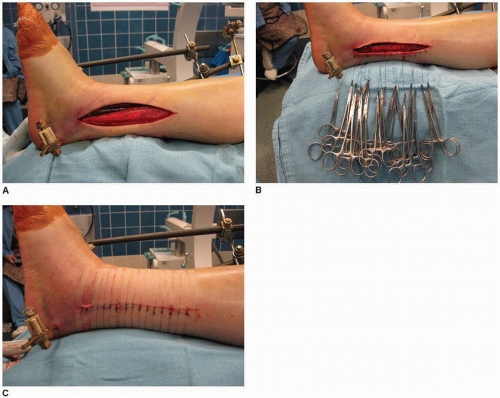
While a straight lateral incision is typically performed for simple fractures of the fibula, the skin incision for fibular fixation in the setting of a tibial plafond fracture should be performed in a relative posterolateral location; specifically, slightly posterior to the palpable posterior border of the fibula. This allows for the use of
the same incision if a posterolateral tibial approach is later chosen and increases the soft-tissue bridge if an anterolateral exposure is required for tibial fixation. This posterolateral incision is also not directly located over the subcutaneous fibula and therefore may help to minimize wound complications in this area (Fig. 31.4).
the same incision if a posterolateral tibial approach is later chosen and increases the soft-tissue bridge if an anterolateral exposure is required for tibial fixation. This posterolateral incision is also not directly located over the subcutaneous fibula and therefore may help to minimize wound complications in this area (Fig. 31.4).
The incision is longitudinal and centered over the fibula fracture. Dissection is carried directly through the subcutaneous tissue, and the fascia of the lateral compartment is incised longitudinally along the entire length of the skin incision. The anterior edge of the incised fascia is then retracted anteriorly, and the peroneal musculature is retracted posteriorly. To preserve vascularity to the skin, care is taken to minimize the creation of planes between the subcutaneous tissue and the fascia over the lateral compartment. Depending on the location of the fracture, the superficial peroneal nerve may be encountered within the lateral compartment prior to exiting the fascia and traveling within the subcutaneous layer.
TECHNIQUE
Fibular reduction and stabilization positively influence the initial management of these injuries in the following ways:
Restoration of accurate fibular length, alignment, and rotation indirectly reduces the majority of tibial deformity secondary to the ligamentous and other soft-tissue attachments between the two bones.
After fibular reduction and fixation, residual tibial displacement can be managed with an ankle joint spanning external fixator using the reduced and stabilized fibula as a fulcrum.
Fibular reduction commonly neutralizes the tendency for valgus angulation and/or lateral translation of the talus and associated tibial pilon fracture fragments.
Anatomic reduction of the fibula allows indirect reduction of the associated anterolateral (Chaput) and posterior (Volkmann) tibial articular fragments via the anterior and posterior distal tibiofibular syndesmotic ligaments, respectively.
Fibular malreduction, therefore, may result in the talus not being centered beneath the anatomic axis of the tibia or may result in distal tibial metaphyseal malalignment. Notably, extension malreduction of the fibula is not infrequent
and results in anterior translation of the talus relative to the anatomic axis of the tibia and ultimately anterior talar extrusion from beneath the tibial plafond. Fibula fractures that occur predominantly from rotational or tension mechanisms are typically stabilized with one-third tubular plates. Unlike rotational ankle fractures, however, the associated fibular fractures seen with high-energy tibial plafond fractures fail in compression or tension. Compression failures frequently demonstrate comminution with transverse and oblique fracture plane orientations. Tension failures are usually simpler, in terms of comminution, and generally occur in a relatively distal location. While one-third tubular plates may occasionally be satisfactory, stiffer constructs are often required. Stacked one-third tubular plates, precontoured distal fibular periarticular plates, and 2.7-mm or 3.5-mm dynamic compression plates may be required. Manufactured, stiff precontoured periarticular distal fibular plates are particularly advantageous, in that they provide satisfactory stability, while providing a reduction template by virtue of their design.
and results in anterior translation of the talus relative to the anatomic axis of the tibia and ultimately anterior talar extrusion from beneath the tibial plafond. Fibula fractures that occur predominantly from rotational or tension mechanisms are typically stabilized with one-third tubular plates. Unlike rotational ankle fractures, however, the associated fibular fractures seen with high-energy tibial plafond fractures fail in compression or tension. Compression failures frequently demonstrate comminution with transverse and oblique fracture plane orientations. Tension failures are usually simpler, in terms of comminution, and generally occur in a relatively distal location. While one-third tubular plates may occasionally be satisfactory, stiffer constructs are often required. Stacked one-third tubular plates, precontoured distal fibular periarticular plates, and 2.7-mm or 3.5-mm dynamic compression plates may be required. Manufactured, stiff precontoured periarticular distal fibular plates are particularly advantageous, in that they provide satisfactory stability, while providing a reduction template by virtue of their design.
The fibula is reduced using direct or indirect techniques or a combination thereof, and stabilizing implants are typically applied to the posterolateral aspect of the bone. The placement of supportive bumps solely beneath the posterior aspect of the hindfoot or ankle, as is commonly done for rotational ankle fractures, should be avoided as this can result in an extension deformity of the fibula and tibia. If improved access to the fibula is required, the entire leg should be elevated and supported on several bumps to avoid creating this common but avoidable angulatory deformity.
While fibular reduction and fixation is typically performed prior to tibial reduction and external fixation, there are occasions where reversal of this sequence may be advantageous. If limb shortening or instability is significant, obtaining fibular reduction will be problematic. In these situations, external fixation of the tibial component is performed initially to obtain provisional restoration of length, alignment, and rotation. Fibular reduction and fixation is then performed. Similarly, in the setting of a comminuted fibula fracture, where a comparatively minimally comminuted tibial fracture component exists, closed manipulative reduction and external fixation of the tibia initially may more accurately restore length, alignment, and rotation of the limb and facilitate the subsequent fibular reduction. In situations with significant fibular comminution, indirect reduction using a periarticular fibular plate is very useful. Using an open approach, but with minimization of dissection in the zone of injury, the distal portion of the plate is applied to the lateral malleolus in an anatomic position and held with Kirschner wires (K-wire) and a small bone-holding clamp. Gradual restoration of fibular length is achieved with traction applied to the foot and heel. Once length is achieved, the proximal portion of the plate is secured to the fibula proximal to the fracture using another bone-holding clamp. The reduction is then adjusted until there is clinical and fluoroscopic confirmation of restoration of length.
TIBIA
Very infrequently, the x-rays demonstrate a widely displaced or dislocated posterolateral Volkmann fracture fragment. This injury pattern can be particularly challenging since definitive tibial plafond anterior exposures may not allow adequate visualization or opportunity for satisfactory stabilization of this fragment. In these situations, a posterolateral surgical approach to the tibia can be performed in conjunction with the initial stage and will simplify the subsequent tibial reduction and fixation (Fig. 31.5).
The patient is positioned in the lateral decubitus position with the uninjured limb down and held there with a deflated beanbag. The down limb is padded, particularly around the peroneal nerve at the knee and the lateral malleolus. A ramp pillow or folded blankets are used to support the injured extremity. The skin incision is performed halfway between the posterior border of the fibula and the lateral aspect of the Achilles tendon. Care is taken to avoid injury to the sural nerve. The fascia overlying the peroneal musculature and tendons is incised and the peroneals are retracted anteriorly. The underlying fascia is identified and incised longitudinally, exposing the flexor hallucis longus (FHL) muscle and tendon. This unit is elevated from the posteromedial aspect of the fibula and retracted posteromedially. During this dissection, the peroneal artery and accompanying veins may be encountered immediately posterior to the fibula and require ligation. The posterior Volkmann fragment is then identified, cleansed of organizing hematoma, and the posterior tibiofibular ligment is left intact if present. The fibula can then be approached by now retracting the peroneals posteriorly. Fibular reduction often greatly aids in the reduction of the posterior Volkmann fragment and is the first-reduction maneuver performed. In situations where a poor ligamentotaxis effect on the fragment with fibular reduction occurs, reduction of the fibula helps to bring the talus into a more centralized position beneath the tibia allowing easier manipulation of the Volkmann fragment. One-third tubular, one-quarter tubular, or 2.0-mm plates are typically satisfactory for achieving stability. It is imperative that unreduced anterior and central plafond fracture fragments not be secured with fixation that is used to stabilize the Volkmann fragment to the posterior tibial metaphysis. Once the fibula and Volkmann fractures are reduced and stabilized, the beanbag can be inflated, and the patient is allowed to roll backward to a “sloppy lateral” position. This will allow the application of the external fixator.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree