Thumb Coverage
David Elliot
The primary goals of thumb reconstruction are to restore length and sensation. A thumb should be of adequate length to allow for pinch to the index and middle fingertips and to participate in span grasp with all five digital tips. Adequate length is also essential for developing power grip. The surgeon aims to provide adequate coverage of the deeper, vital structures with soft tissue and skin of good quality. Sensibility of the tip is of particular importance, being crucial to fine pinch. A thumb “post” with no or little movement distal to the basal joint, and/or poor tip shape and sensation, can still work to aid in hand function but will not allow for finesse of function.
In attempting to obtain optimum reconstruction one should avoid shortening the thumb unless absolutely necessary. We encourage distal replantation or composite graft replacement, and also look to homodigital flap reconstruction whenever possible. Care should be spent in nail bed preservation and repair. Any nail greater in length than one third of its normal length should be retained, at least at primary surgery. Reconstruction of the thumb defects with the use of skin grafts from elsewhere on the body can create patches of dissimilar color, texture, and thickness and a noticeably poor cosmetic result. Finally, with respect to mobility and rehabilitation, the time-honored plastic surgical techniques of skin cross-finger, thenar, groin, and cross-arm flaps should be avoided, if possible, as they tether the injured thumb to another part of the body, thus preventing adequate therapy, which may promote edema and stiffness.
Homodigital Flap Reconstruction
Homodigital flap reconstruction involves rearrangement of the soft tissues of the injured digit to achieve healing without seeking tissue for reconstruction from outside that digit. This concept of reconstruction has definite advantages for thumb reconstruction. In particular, it reconstructs “like with like” and avoids the creation of further scarring and morbidity elsewhere on the hand or body. While homodigital reconstruction is advantageous in these respects, the availability of donor tissues within the thumb is obviously limited.
Perhaps the single most important surgical pearl to remember when using homodigital reconstruction is that the thumb and fingers have an astonishing ability to close skin defects of considerable size by a combination of wound contraction and re-epithelialization (Fig. 24-1). Thus, if a portion of the wound can heal under moist antiseptic dressings through secondary intention, the surgeon may use the homodigital flaps to cover only those portions of the wound which contain exposed vital structures or to improve soft tissue coverage over bone. The flap does not have to cover the entire defect, only the essential components of the defect.
Preoperative Planning
Preoperative planning should include AP and lateral radiographs in addition to a thorough hand exam. Concomitant arterial and nerve injuries can often be identified prior to exploration within the operating room. Many thumb injuries will occur in conjunction with other hand injuries and revascularization of injured digits takes precedence over coverage issues. Wounds should be debrided of all necrotic tissue and free of infection before embarking on soft tissue coverage.
Patient Positioning
Patients are positioned supine on the operating room table. General or regional anaesthesia may be used during the surgical procedures. In some cases, thumb or wrist blocks may be used when performing smaller flaps or for debridement procedures. An upper arm tourniquet is placed prior to prepping and draping the patient. Surgery is always performed under tourniquet control to aid in visualization of vital structures.
The following sections present our preferred techniques for thumb reconstruction based on location of the original defect.
Palmar Defects
Neurovascular Tranquilli-Leali or Atasoy-Kleinert Flap
Indications/Contraindications
Historically, the original Tranquilli-Leali or Atasoy-Kleinert flap has been described to cover partial amputation defects of the distal phalanx; however, these flaps do not work well on the thumb because of the inflexibility of the subcutaneous soft tissues. Laterally based single pedicle flaps, vascularized in the same way by the small vessels beyond the trifurcations of the digital arteries, also move poorly. The neurovascular Tranquilli-Leali or Atasoy-Kleinert flap is designed to be much larger and is islanded on both neurovascular pedicles bilaterally (Fig. 24-2). The flap is designed to extend to, or across, the IP joint crease proximally. This flap works well for minor transverse or oblique injuries of the distal phalanx with exposure of bone.
This flap can be used for stump reconstruction of any length of amputated thumb and is more useful than the original Tranquilli-Leali flap; however, it moves less freely than on a finger, partly because of the fibrous nature of the subcutaneous tissues of the thumb and partly because of what has been described as the “vertical dimension” of the thumb, that is its palmar-dorsal width at the tip (1). On fingers, it can be used to reconstruct defects with a palmar slope of up to 30 degrees; on the thumb it can only reconstruct defects with bone exposure which are dorsally facing, transverse, or palmar facing with less than 10 degrees of slope (Fig. 24-3).
Surgical Technique
The incisions of the V cross the interphalangeal joint crease at an angle and thus do not cause contractures (see Figs. 24-2 and 24-3). When designing the flap, one takes the V incisions out almost to the lateral nail folds distally. Having made the flap wide, the leading edge of the flap after advancement is wider than the original thumb tip. Unless the lateral corners of the flap are excised, this results in a spatulate end to the digit. Cutting off the lateral corners and allowing the resulting raw edges and tip to epithelialize not only narrows the digital tip but also rounds it to achieve a good appearance. The flap is designed as a “V” at its proximal extremity and was conceived to close proximally as a “Y” after the flap has moved distally. Mostly, the proximal donor defect is left open to close under dressings as primary closure of the vertical limb of the “Y” tightens
the thumb too much proximally over the vascular pedicles of the flaps and compromises vascular inflow into the flap.
the thumb too much proximally over the vascular pedicles of the flaps and compromises vascular inflow into the flap.
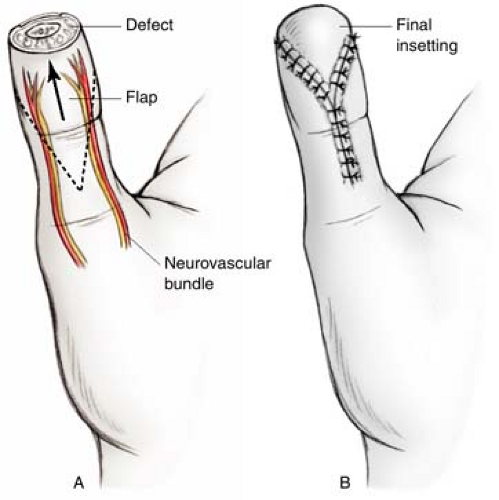 FIGURE 24-2 A,B: Illustration of the neurovascular Tranquilli-Leali flap. The flap extends proximally beyond the IP crease and includes both the neurovascular bundles. |
Moberg Flaps
Indications/contraindications
With greater losses of palmar thumb tissue, more sloping palmar oblique injuries, and when the whole distal pulp of the thumb has been avulsed, the neurovascular Tranquilli-Leali flap is too small and cannot advance sufficiently. For larger thumb defects confined to the distal phalanx we favor the use of a modified Moberg flap. The Moberg flap, as described by Moberg in 1964, is an advancement flap based on both neurovascular bundles of the thumb (2). The advantages of this flap are that it returns sensation and glabrous skin to the defect site. The downside to the original flap design was the IP joint flexion contracture necessary to achieve suture of the flap distally to the nail. Our preferred modification of the Moberg flap avoids the IP joint flexion necessary with the original to advance the flap to the tip of the digit. This is, essentially, O’Brien’s modification of the Moberg flap, but uses a “V” tail proximally instead of a skin graft at the base of the thumb (Fig. 24-4) (3). This V-Y Moberg flap achieves the same excellent results as the original Moberg flap in terms of sensibility of the thumb tip, but without the restrictions of interphalangeal joint movement associated with the original flap or the need for skin graft of the O’Brien modification.
There is no danger of dorsal skin loss in raising Moberg-type flaps on the thumb, as the dorsal skin of the thumb has a separate blood supply. Because of the safety of the V-Y Moberg flap, the speed and ease with which it can be dissected, and the excellent sensibility of the thumb tip which can be achieved with it, this technique remains our favorite thumb tip reconstruction if the defect is limited to the distal phalangeal segment of the thumb.
Technique
The flap is created laterally along the mid-lateral lines on each side of the thumb and with the tip of the proximal “V” well back on the thenar eminence, at least as far proximally as a line drawn proximally from the ulnar border of the middle finger. This creates a large flap which incorporates the more lax subcutaneous tissues of the thenar eminence. Smaller flaps with the proximal “V” at the base of the thumb move less easily and less far distally. The wider and longer flap avoids any need for addition of techniques to accommodate tightness at the base of the thumb. The use of this flap is considerably extended in reconstructing palmar oblique defects if the pulp distally which is denuded of skin cover remains as the leading edge of the flap, with suture of subcutaneous tissue, not skin, to the nail distally then epithelialization under dressings (Fig. 24-4).
Other Flaps
Other flaps have an infrequent use in reconstruction of the tip and palmar surface of the thumb but can be useful.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










