Thumb Carpometacarpal Joint Resection Arthroplasty
Matthew M. Tomaino
DEFINITION
Osteoarthritis, or more appropriately osteoarthrosis, is a common problem in the hand. The trapeziometacarpal joint is commonly affected, second in frequency only to the distal interphalangeal joint. Trapeziometacarpal joint osteoarthritis, however, can be much more disabling secondary to pain and weakness of grip and pinch strength.
The surgical management of symptomatic basilar joint arthrosis varies according to the anatomy, radiographic staging, intraoperative confirmation of disease stage, and patient requirements.
ANATOMY
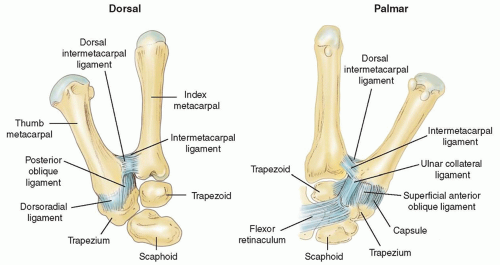
The thumb carpometacarpal (CMC) joint is a biconcave joint, allowing for motion in three planes: flexion-extension, abduction-adduction, and pronation-supination.
There are minimal constraints from an osseous standpoint, making the ligamentous structures extremely important in providing stability to the base of the thumb. A total of 16 ligaments have been described around the thumb CMC joint, 7 of which are primary stabilizers of the thumb metacarpal (TM).
PATHOGENESIS
The pathogenesis of CMC joint arthrosis is multifactorial, involving biochemical and biomechanical influences. The synovial fluid within the joints contains cytokines that invariably play a role in cartilage degradation and decreased ability to withstand the loads generated at the joint during daily activities.9 Although not clearly delineated, estrogen or estrogen-related compounds probably play some protective role, which may explain the increased incidence of osteoarthritis in postmenopausal women (10 to 15:1).
The palmar or anterior oblique ligament (AOL), or so-called beak ligament, has been shown to be the most important stabilizing ligament of the thumb. Degeneration or functional incompetence of this ligament leads to laxity, abnormal translation of the metacarpal on the trapezium, increased shear forces, and resultant abnormal wear patterns. This eburnation of the articular cartilage initially occurs along the palmar aspect of the joint.10 With progression of disease, osteophytes develop and eburnation progresses throughout the entire joint surface.
Osteoarthrosis can also develop from damage and disruption of the articular cartilage. Any fracture through the metacarpal or trapezium joint surfaces yield arthrosis. Anatomic restoration of the joint surface can minimize this sequela but cannot eliminate the risk entirely. Paradoxically, however, a Bennett fracture may protect the joint from the development of osteoarthritis, assuming subluxation has been treated, by virtue of consequential unloading of the volar aspect of the joint.
NATURAL HISTORY
Arthrosis of the thumb CMC joint begins along the palmar aspect of the metacarpal secondary to laxity of the AOL. As the process progresses, the entire base of the metacarpal and distal trapezium becomes involved.
There is initial eburnation of the cartilage, which progresses to osteophyte formation. As the disease continues, the TM assumes an adducted position and the metacarpophalangeal (MCP) joint may compensate by becoming hyperextensile, resulting in varying degrees of MCP joint hyperextension.
The disease can involve all the trapezial articulations as well as the scaphotrapezoidal joint.15
PATIENT HISTORY AND PHYSICAL FINDINGS
Thumb CMC joint arthrosis often presents with pain at the base of the metacarpal. The pain may or may not be present at rest. It will be exacerbated with activities involving loading the TM base, such as turning a doorknob, twisting a lid off a jar, or turning a key.
With advanced disease, the thumb subluxes in a dorsal direction and becomes fixed in adduction. This manifests as a prominence at the base of the thumb and decreased ability to abduct the thumb away from the palm. In an effort to compensate for this, the MCP joint will often hyperextend, creating a zigzag deformity.
Symptoms do not always correlate with the clinical or radiographic appearance, meaning that a patient may have advanced clinical and radiographic disease but be minimally symptomatic. Conversely, a patient may have substantial symptoms with minimal radiographic changes and no clinical deformity at rest.
Other conditions causing pain at the base of the thumb must be eliminated, such as de Quervain disease, trigger thumb, and carpal tunnel syndrome. Although more than one condition may exist, the physical examination can usually determine the most troubled area.
Physical examination includes the following:
Point tenderness assessment: With the TM adducted, the CMC joint is palpated beneath the thenars. Tenderness confirms the clinical significance of changes seen on radiographs.
Reproduction of symptoms on the CMC grind test confirms the CMC joint as a site disease.
Key pinch assessment: If dynamic collapse accompanies pinch, MCP joint fusion or capsulodesis is recommended (FIG 2).
IMAGING AND OTHER DIAGNOSTIC STUDIES
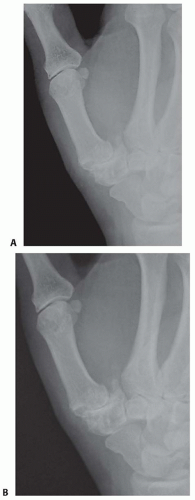
Plain radiographs are the imaging modality of choice for evaluation of thumb CMC joint arthrosis. These include a pronated anteroposterior (AP) (Robert’s view), lateral, and a 30-degree posteroanterior stress view (FIG 3).
Eaton and Littler have described a radiographic staging system, which is commonly used, but Tomaino et al15 have emphasized routine assessment of the scaphotrapezoidal joint, both radiographically and intraoperatively, to rule out scaphotrapezoidal arthritis—what they termed stage V disease.
Stage I: normal-appearing or widened joint space secondary to synovitis
Stage II: joint space narrowing and osteophyte formation smaller than 2 mm
Stage III: joint space narrowing with osteophytes larger than 2 mm
Stage IV: scaphotrapezial joint space involvement in addition to narrowing of the TM joint
Stage V: stage IV appearance with the addition of narrowing or osteophytes in the scaphotrapezoid joint
The scaphotrapezoid joint is not specifically addressed in this system and may be difficult to assess radiographically, but it should always be assessed clinically during operative intervention because it may be a source of continued pain.
DIFFERENTIAL DIAGNOSIS
De Quervain disease
Trigger thumb or stenosing tenosynovitis
Carpal tunnel syndrome
NONOPERATIVE MANAGEMENT
Most patients with symptomatic thumb CMC joint arthrosis benefit from a trial of conservative therapy, which may include corticosteroid injection, thenar isometric strengthening exercises, and splinting.
Although this will not eliminate the problem or alter the underlying disease process, conservative treatment often reduces symptoms, at least transiently, allowing the patient the opportunity to plan for surgical treatment at the most opportune time.
Differential injection of steroids can also be helpful to assess how much of a patient’s symptoms are coming from the thumb CMC joint versus other areas (carpal tunnel or de Quervain disease).
SURGICAL MANAGEMENT
The indications for surgical intervention for symptomatic thumb basilar joint arthrosis include pain and weakness.
There are multiple procedures used to treat symptomatic CMC thumb arthritis, many of which have merit depending on the extent of arthritic involvement.
Pantrapezial involvement contraindicates the use of arthrodesis or implant arthroplasty, in particular, because of the risk of incomplete pain relief.
Arthrodesis may be preferable in younger, high-demand patients such as laborers.
Resection arthroplasty can be performed with ligament reconstruction or without (hematoma distraction arthroplasty).5,7
The flexor carpi radialis (FCR) and abductor pollicis longus (APL) are most commonly used when performing “suspensionplasty.”
Preoperative Planning
Consideration should be given to the age of the patient and the demands placed on the thumb.
Dynamic collapse of the MCP joint during key pinch necessitates MCP fusion or capsulodesis.
Intraoperative evaluation of the scaphotrapezotrapezoidal (STT) joint is critical to ensure adequate pain relief after surgery. Thus, hemitrapeziectomy is rarely performed once the decision to proceed with conventional resection arthroplasty is made. If retention of the proximal trapezium is elected because of the absence of STT disease, Artelon resurfacing or joint arthroplasty may be elected.
Intraoperative assessment of the scaphotrapezoidal joint is recommended, and if changes exist, a 2- to 3-mm resection of the proximal trapezoid is performed.15 Care is taken not to injure the capitate.
Suspensionplasty ensures stability of the TM during pinch and grip, resisting the cantilever bending forces that will potentially lead to subluxation and proximal migration compared to trapeziectomy alone.
Intermediate-term outcome of the hematoma distraction arthroplasty suggests that this procedure may have a role in providing excellent pain relief in well-selected patients for whom grip strength is a less important issue.5
Positioning
The patient is supine, and the involved hand and arm are supported by a hand table.
Approach
Trapezium excision and ligament reconstruction and suspensionplasty can be performed using the Wagner (volar) approach or a dorsal approach. I prefer the dorsal approach except when performing an Eaton ligament reconstruction, in which case a volar approach is used. I have modified my technique since performing the ligament reconstruction and tendon interposition (LRTI) arthroplasty exclusively during the first 10 years of practice.12,14
Over the past 5 years, I have performed a suspensionplasty using a distally based slip of the APL tendon, which obviates the need for a bony channel. This is a variation of other suspensionplasty techniques.8,11,16 In addition, I no longer pin the joint or interpose tissue into the space remaining after trapezial resection. The procedure is performed more expeditiously and seems to be associated with equivalent outcomes.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree