Fig. 5.1
Medial view of a sagittal section of a human cadaver (medial pterygoid muscle removed) showing the course of the lingual nerve (a), the inferior alveolar nerve (b), and the mylohyoid nerve (c) in the L3M region (Preparation of Prof. Dr. Alfonso Rodríguez, Chairman of Anatomy and Embriology of the Universitat Autònoma de Barcelona (UAB))
An important difference between LN and IAN, as mentioned above, is that the latter has an intraosseous course, which protects it against damage and in case of sectioning, provides a scaffold for nerve regeneration. Unfortunately, in case of compression, the stiffness of the mandibular canal can foster nerve damage, especially in case of swelling or bleeding within the canal. As the LN lies within soft tissue, close to the lingual cortical plate, it is more exposed to compression, and scratching or catching can occur more easily as a result of the use of retractors, burs, or other surgical instruments.
There are other nerves that can be also damaged as a result of L3M extraction. The mylohyoid nerve, a branch of the IAN, innervates the mylohyoid muscle, the anterior belly of the digastric muscle, the skin of the inferior part of the chin, the submandibular and sublingual glands, and, in approximately half of the cases, the lower incisors [23, 24]. Its impairment is much more infrequent and less noticeable by the patient than that of the IAN, since it affects only a small skin area in the lower part of the chin, close to the midline. However, the etiology and pathogenesis of neural damage is quite similar to the injury of the LN.
Finally, the buccal nerve can also be damaged as a result of L3M extraction. This nerve, which must be anesthetized to extract the L3M, is formed by sensory fibers carrying input from the buccal mucosa, the buccal gingiva and mucosa of the lower molars (and eventually premolars), and the skin. It can be damaged as a result of excessive reflection of the buccal flap or in the rare cases of an intraosseous course of the buccal nerve, but this injury seems to be very uncommon.
5.2 Etiology and Prevention of Damage to the Lingual Nerve
There is a great variation in the dental literature regarding the prevalence of LN injury after L3M extraction. This fact reflects important differences in the management of the soft and hard tissues on the lingual side of the L3M.
5.2.1 Buccal Versus Lingual Approach for L3M Removal
The L3M usually lies closer to the lingual cortical plate, which is considerably thinner than the buccal plate. This anatomic difference is the rationale for the so-called lingual split technique, which consists of removing the thin lingual cortical plate using a chisel or a bur and extracting the L3M through the resulting lingual opening. The lingual split is performed quickly and simply, but manipulation on the lingual side of the L3M renders an unacceptably high prevalence of LN injuries [11]. Despite the claim that these injuries are transient in nature, it must be taken into account that any nerve compression or scratching can cause axonal degeneration. Thus, the ideal situation is to avoid all types of nerve manipulation and possible injury, even mild traction on the nerve. Indeed, a systematic review has confirmed that the lingual approach causes significantly more LN injuries than the standard buccal approach [25].
In uncommon cases, the LN can lie over the crest distal to the lower second molar covering the impacted L3M. This situation places it at risk in case of surgical L3M extraction, since the incision can section or scratch the nerve [21, 22]. Thus, it is advisable to stay away from the crest distal to the second molar and to place the incision slightly towards the buccal mucosa in a distobuccal extension (Fig. 5.2). The buccal approach requires a greater amount of bone removal than the lingual approach, but it is safer for the LN. However, the non-raised soft tissues of the lingual side of the wound often limit the surgeon’s vision. To facilitate it and to “protect” the lingual soft tissues and the lingual cortical plate during bone removal or tooth sectioning, different separators have been proposed [26, 27]. In the past, some authors thought that the wider the retractor on the lingual side of the flap, the better, because it increased the risk of transient LN injury but decreased the risk of a permanent damage. However, as lingual retraction itself has been recognized as a major risk factor of LN damage, as reported in the next section, the use of retractors has been progressively abandoned.


Fig. 5.2
Design of an envelope flap for L3M extraction (blue line). The incision over the impacted L3M should be slightly buccal to the crest, from the distobuccal aspect of the adjacent lower second molar towards the external oblique ridge. Avoiding the crestal bone over the L3M eliminates the possibility of LN section if the LN is over the crest
5.2.2 Use of Separators to Retract the Lingual Flap
As mentioned above, different types of separators have been advocated to retract the lingual flap during L3M extraction. They are inserted between the lingual cortical plate and the mucosa of the lingual side of the flap (Fig. 5.3) in order to better visualize the bone that covers the L3M and to “protect” the lingual flap from any elevator or bur trauma. This “protection,” sometimes performed with quite wide instruments to cover a larger area, has been traditionally recommended [12]. Failure to prove that the lingual flap was retracted has even resulted in medicolegal problems [28].
Fig. 5.3
(a) Insertion of a separator (Freer periotome) gives better vision of the bone distal to the lower second molar and prevents accidental impingement of the bur in the lingual flap. However, it traumatizes the soft tissues of the lingual side of the wound and causes an increase in LN injuries. (b) It is advisable to use only a buccal approach, without separating the soft tissues on the lingual side of the wound. The flap yields a good vision and does not put the LN at risk (Images reprinted with permission from Gargallo-Albiol et al. [32])
However, many publications have shown that reflecting the lingual tissues during L3M extraction does not avoid, and even favors, the occurrence of LN injuries [5, 12, 29–31]. A systematic review has demonstrated that the buccal approach, without any lingual tissue retraction, causes approximately nine times less transient injuries than the same approach with retraction of the lingual soft tissues [25]. On the other hand, a randomized controlled trial (RCT) at our institution demonstrated three times more LN injury when the lingual flap was retracted, although this difference was not significant due to small sample size and low prevalence of LN damage [32]. The major role played by lingual flap retraction in the etiology of LN injuries was confirmed after a report showed how lingual flap retraction was associated with transient LN injuries [31]. As a result, the surgical technique was modified to avoid lingual flap tissue manipulation, and then the number of transient LN injuries was divided by four [33]. An RCT has confirmed that lingual flap retraction significantly increases transient LN damage [34]. Therefore, current evidence suggests not only that the buccal approach is safer for the LN than the lingual approach, but the buccal approach should be performed without any retraction of the lingual tissues, if possible.
5.2.3 Use of Burs or Chisels
Currently the preferred method for bone removal in L3M extractions is with the use of a bur and a handpiece. However, especially when using the lingual split technique, bone removal can be accomplished with a chisel. Although some reports have concluded that chisels are safer and associated with less IAN injuries [5], this is not valid since burs are easy to control and allow very precise bone removal as opposed to chisels.
Today there are several other instruments that can be used to remove bone. Er:YAG or Er,Cr:YSGG lasers can perform very controlled bone removal and even tooth sectioning (Fig. 5.4) [35]. However, although some lasers are very precise and gentle tools for bone removal, tooth sectioning is usually performed using a rotating bur, which is considerably faster and allows better tactile control of deep tooth sectioning. Also piezosurgery can be used to remove bone during L3M extraction [36]. Although the postoperative course seems to be comparable to the conventional osteotomy using burs, the piezosurgery instrument, unlike the bur, does not cause harm if it contacts the IAN or LN. But, piezosurgery is slower to perform, and there is limited evidence on its potential beneficial effects in L3M removal.
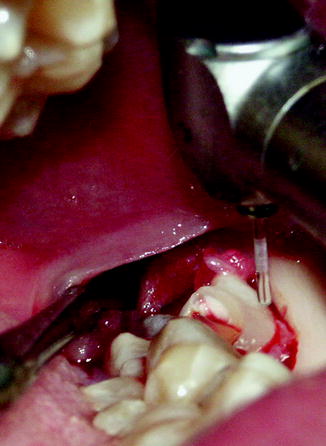
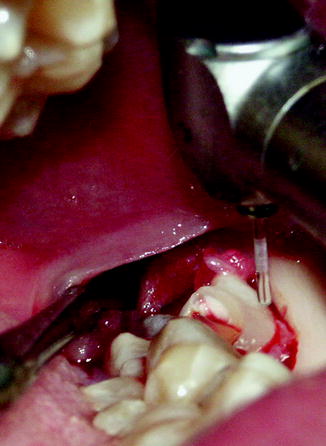
Fig. 5.4
Extraction of a L3M using Er,Cr:YSGG laser. The optic fiber tip allows a precise and effective bone removal. Tooth sectioning can also be performed using the same technology, but for practical reasons a handpiece is often used (Courtesy of Dr. Josep Arnabat-Domínguez, Professor of Oral Surgery of the University of Barcelona and Codirector of the EMDOLA Master Degree. Barcelona, Spain)
5.2.4 Integrity of the Lingual Cortical Plate
During bone removal, and especially tooth sectioning, care must be taken so that the lingual cortical plate is not perforated. An attempt to complete the extraction in the minimal possible time can lead to careless grinding of the bone beyond the L3M tooth. As the roots usually lie very close to the lingual cortical plate, or even perforate it occasionally, there is a risk of penetration through this thin cortical into the soft tissues on the lingual side. Perforation of the periosteum can directly damage the LN or cause fibrosis that can compress the nerve during healing.
It is of utmost importance to maintain the lingual cortical plate in an undamaged condition since it is functioning to protect the LN. Allowing adequate time to plan and perform any root or tooth sectioning of the L3M, avoiding excessive stretching of the lingual soft tissues, and maintaining an undisturbed visualization of the surgical field are the keys to avoid placing the lingual cortical plate, and thus, the LN, at risk for iatrogenic injury.
5.2.5 Wound Cleaning and Suture
Suture placement has not been identified as a significant risk factor of LN injuries in L3M extraction. However, in surgical L3M extractions, the surgeon should consider the possibility of a close relationship of the LN and the crestal bone distal to the adjacent second molar and avoid placing the sutures too inferior on the lingual side.
After the removal of partially erupted L3M, any fibrotic, cystic, or inflammatory tissue should be carefully removed to facilitate primary wound closure and prevent degeneration of those tissues into cysts or tumors. However, caution should be applied when removing soft tissue after the extraction, such as fibrous tissue or remnants of the dental follicle since the IAN may be exposed in the socket. Good vision of the lingual side of the wound and avoiding excessive stretching of the tissues are important to avoid damaging the LN, in case it lies close to the distal bone of the second molar. Excessive stretching or tissue removal must be avoided, and it is better not to obtain primary closure of the wound rather than risking an LN damage. In case of an iatrogenic LN injury from suturing, the cause can be the wound caused by the needle or compression due to the suture thread. Any transient LN paresthesia is likely from a compressive injury to the LN from the suture, and this will likely resolve spontaneously.
5.2.6 Experience of the Surgeon
Some reports have shown that senior surgeons seem to cause significantly more LN injuries during L3M extraction [11, 29]. This fact could be related to a selection bias (senior surgeons tend to operate the deepest or more difficult L3Ms) or due to the use of a more aggressive technique. In fact, the prevalence of LN injuries in these reports is very high (from 11.5 to 36.0 % for senior surgeons). Moreover, in one of these reports [29], the correlation between depth of impaction and LN injury was only appreciated in L3M operated by senior surgeons under general anesthesia, which supports the probable explanation of a more aggressive technique.
Indeed, at least for buccal approaches to L3M extraction, surgical inexperience seems to be associated to LN injuries only when the lingual soft tissues are elevated to place a separator, since lingual flap retraction is the most relevant cause of LN injury as discussed above [31]. Indeed, the opposite has also been found, and there are certainly other reports that indicate that resident surgeons in training have a higher incidence of IAN and LN injuries than faculty surgeons and that the surgical time is increased for the more inexperienced surgeons.
5.2.7 Age
Although some reports suggest that the prevalence of trigeminal nerve injuries could slightly increase with age [10, 37], prevalence of LN injury after L3M extraction does not seem to depend on age [31, 33], as much as it does with IAN injury [38, 39]. Other reports do show a clear association between postoperative L3M extraction and paresthesia, as well as other complications, in the older patient population.
5.3 Etiology and Prevention of Damage to the Inferior Alveolar Nerve
The most important risk factor for IAN injuries caused by L3M extraction is the anatomical proximity between the roots of the third molar and the mandibular canal. Thus, prevalence of IAN injuries is not only technique-dependent, but, instead, it depends upon preoperative factors that can be identified with a thorough clinical and radiological examination. As a result, the range of prevalence of IAN injury caused by L3M extraction is not as broad as in the case of LN injuries.
5.3.1 Germenectomy Versus Delayed Extraction
Germenectomies, or surgical extractions of L3M whose roots have not developed or have less than two thirds of root formation, have a significantly lower risk of IAN injury, with the percentage of IAN impairment being 0–0.3 % [40, 41]. This is probably due to several factors including (1) the root is separated from the mandibular canal and it usually gets closer to it as the root grows, (2) the bone is more flexible in teenagers than in adults, and (3) the force that must be applied to luxate and elevate the tooth is considerably lower than for L3M with formed roots.
On the other hand, germenectomy is usually performed without a clear indication for extraction. In fact, the guidelines for extraction promulgated by SIGN (Scottish Intercollegiate Guidelines Network) and NICE (National Institute for Health and Clinical Excellence) do not support extraction of asymptomatic third molars, which is generally the case with germenectomies, with some exceptions (for instance, difficulty in obtaining dental care in certain remote areas) [42, 43]. Thus, it must be taken into account that although the risk of IAN damage is lower, germenectomy could have an unfavorable risk–benefit ratio. Nevertheless, asymptomatic third molars may not be disease-free if affected by periodontal disease, for instance. Other guidelines, such as the AAOMS Clinical Practice Guidelines for Oral and Maxillofacial Surgeons, are not so restrictive as the NICE or SIGN guidelines [44].
5.3.2 Radiological “Alert” Signs
Superposition of the mandibular canal and the roots of the L3M in the panoramic radiograph can be the result of a true anatomical relationship such that the mandibular canal is in close proximity to the tooth roots, or merely a projection artifact, where the mandibular canal lies in a buccal or lingual position and it is physically separated from the L3M. To distinguish cases where there is a true anatomical contact between the mandibular canal and the L3M, seven “warning” signs have been described including [45] (Fig. 5.5) the following: darkening of the root, deflection of the root, narrowing of the root, deviation of the mandibular canal, narrowing of the mandibular canal, interruption of the white lines of the mandibular canal, and a dark and bifid root. It seems that interruption of the white line, darkening of the root, and deviation of the mandibular canal are consistently associated with a greater risk of IAN surgical exposure or damage [17, 38, 39, 45–47]. The absence of any of these signs, and, of course the lack of superposition of the mandibular canal and the L3M roots, seems to rule out the possibility of IAN damage if proper surgical technique is used. Indeed, radiological signs have proved to be very specific in ruling out IAN exposure during surgery with a negative predictive value of the surgeon’s evaluation of radiological signs of approximately 99 % [48]. However, the existence of several “warning” signs in the panoramic radiograph has a low sensitivity for detection of IAN exposure (approximately 25 %). Also, these signs have also a low positive predictive value of IAN damage; the presence of several signs indicates a risk of IAN damage between 10 and 20 % [17], which is approximately the prevalence of IAN paresthesia when a CT scan shows that the cortical outline of the mandibular canal is disrupted by the L3M [49].
Fig. 5.5
Examples of radiographic predictors of potential nerve injury, including (a) darkening of the root, (b) deviation of the mandibular canal, (c) interruption of the white lines of the mandibular canal, (d) deflection of the root, and (e) narrowing of the root
5.3.3 Conventional Radiography Versus Computed Tomography
Two-dimensional radiographs provide only an approximation of the relationship between the roots of the L3M and the mandibular canal (Fig. 5.6). The existence of a true anatomical relationship can only be detected using tomographic techniques. However, due to the high prevalence of superposition of the L3M roots and the mandibular canal, the low positive predictive value for nerve injury of the computed tomography (CT) (similar to the orthopantomography), and the increased cost and radiation exposure of this technique, its systematic use does not seem to be justified for routine evaluation.
Fig. 5.6
Portion of a panoramic radiograph showing signs of root proximity to the inferior alveolar canal
CT is especially useful to evaluate the risk–benefit ratio of an L3M extraction, and it helps selecting the surgical strategy when the mandibular canal is close to the cementoenamel junction (Fig. 5.7) or when it is suspected to perforate an L3M root. In the first case, ostectomy can help to avoid the risky areas, buccal or lingual to the L3M, and in the second example, tooth sectioning can avoid a traction injury or avulsion of the IAN.

Fig. 5.7
CT of a L3M depicts a mandibular canal close to the buccal CEJ. Removal of the buccal bone should be performed with extreme caution, as it can decorticate and eventually injure the mandibular canal, although it is not in contact with the tooth. In this case CT offers important information to plan the operation

Fig. 5.8
CT section displaying the roots of a L3M close to the lingual cortical plate. This should alert the clinician of two dangers: (1) accidental displacement of the roots to the submandibular space during luxation and (2) risk of laceration of the lingual periosteum that could cause fibrosis near the LN
Nevertheless, CT does not seem to modify the surgical technique in most cases, and the prevalence of IAN injury seems to be approximately the same with or without a preoperative CT [17]. Therefore, it is questionable whether a CT is required in other situations than those described above although it is undeniable that it provides valuable information (Fig. 5.8).
The spread of cone-beam computed tomography (CBCT) has made 3-D techniques available in dental offices. This technique, despite being less precise than conventional CT because of patient movement, is less expensive and delivers a low radiation dose.
5.3.4 Ostectomy and Tooth Sectioning (Burs, Chisels, Piezosurgery, and Laser)
Ostectomy and tooth sectioning can reduce the amount of strength that must be applied to the roots of the L3M during extraction. If the L3M are in close proximity to the mandibular canal, this action is clearly beneficial, as it reduces the chances of IAN compression. However, if ostectomy is made without caution, it can cause direct damage to the IAN, or increase wound bleeding, which in turn can cause an IAN injury by compression. Ostectomy must be controlled and thoroughly oriented to facilitate luxation and avoid IAN or LN impingement.
Piezosurgery reduces the chances of nerve damage due to impingement of the burs or chisels into the mandibular canal and also reduces vibration or strength required to perform ostectomy or tooth sectioning. However, there is lack of data on IAN damage comparing piezosurgery with the conventional buccal approach with burs, which is the most common technique used for L3M extraction.
Different laser types have also been used for L3M extraction. Although some lasers, such as Er:YAG or Er,Cr:YSGG laser, can be safely used for this indication and compare favorably with the conventional buccal approach with rotating burs [35], some laser light wavelengths and power settings can directly damage the IAN. Moreover, although ostectomy can be easily and safely performed using lasers, tooth sectioning is usually carried out with rotating instruments for practical reasons. Finally, there is no clear evidence that laser surgery reduces IAN injuries.
5.3.5 Drainage and Postoperative Dressings
Placing antiseptic, antibiotic, or caustic substances into the empty socket after L3M extraction has been recommended for the open treatment of the wound to prevent alveolar osteitis or as a complement to cyst removal [50]. However, in case of nerve exposure, it is advisable to not use intra-alveolar tetracycline because of its documented neurotoxicity [51, 52]. In the case of Carnoy’s solution for complementary surgical treatment of keratocystic odontogenic tumors, although it has been shown to damage peripheral nerves when left in contact for several minutes [53], it seems to be safe [54]. Carnoy’s solution should not be in potential contact with the IAN over 3 min, and special care should apply if the epineurium is not intact [53].
The wound resulting from extraction of the L3M can be closed tightly with sutures and left open to heal secondarily, or a drainage tube or gauze can be inserted to facilitate drainage. It seems that secondary closure (i.e. not covering the socket completely with mucosa) causes less postoperative swelling and pain [55], which could have a beneficial effect on the recovery of the IAN and LN. The insertion of a drainage tube could also prevent swelling [56], with an effect comparable to using a systemic corticosteroid medication [57].
5.3.6 Age
Age is a risk factor for IAN nerve injury caused by L3M extraction [10, 38] and is also a risk factor for poor recovery and wound healing. Age decreases the chances of spontaneous neurosensory recovery and the recovery rate is slower [39]. The explanation for this phenomenon remains speculative, and mechanisms include a reduced neuronal plasticity, a slower recovery rate, or a greater surgical trauma. Indeed, it is well known that age plays an important role in peripheral nerve regeneration, since younger patients recover more easily than older patients [58–61].
5.3.7 Anti-inflammatory Treatment
Although data are limited to a preliminary RCT with a small sample size and thus must be considered with caution, dexamethasone seems to reduce IAN hypersensitivity after L3M extraction [62]. As corticosteroids effectively control swelling after L3M extraction [63–65], the mechanism for reduction of IAN damage is probably a reduction in swelling, which minimizes the chance of nerve compression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








