1.6 The thoracolumbar fascia Functional anatomy of the locomotor system, which is strongly linked to biomechanics, attempts to explain how bones, ligaments, and muscles operate as a system. Consequently, use of categories like spine and pelvis can be misleading. From a biomechanical and neurophysiological point of view they are fully integrated. “Back muscles”, for instance, are categorized in descriptive anatomy as typically spinal. However, parts of these “back muscles” bride the sacroiliac (SI) joints. As an example, in man the multifidus muscle shows an extensive attachment to both the sacrum and the iliac crest (Vleeming & Stoeckart 2007). With the use of descriptive anatomical models it is tempting to regard pain in the area of the SI joints as a separate syndrome, not as part of low back pain. However, these joints are fully and crucially integrated in the spine–pelvis–leg mechanism (Snijders et al. 1993a). To function properly this mechanism needs stability of the pelvis (external movement of the pelvis) and the SI joints and symphysis (internal movement of the pelvis), for effective use of the three levers connected to the pelvis: two legs and the spine. Effective load transfer across the SI joints requires specific action of a variety of muscles, leading to sufficient compression of the SI joint, preventing shear (Snijders et al. 1993a, b). In increasing compression the biceps femoris and gluteus maximus muscles play a role (Vleeming et al. 1989a,b, 1992b 1996; DonTigny 1990; Vleeming 1990; Van Wingerden et al. 1993). Both muscles are attached to the sacrotuberous (and partially the sacrospinous) ligament which functionally bridges the SI joint. Obviously, pain in the area of the SI joints is not necessarily a local problem; it can be symptomatic of a failed load transfer system (Snijders et al. 1993a, b). The strong thoracolumbar fascia (TLF) (Tesh et al. 1987) can be used for load transfer from the trunk to the legs (Mooney et al. 2001). The posterior (PLF) and middle layer (MLF) of this fascia are of special interest because of the multiple connections with muscles. The main interest is whether muscle-induced tension of this fascia can assist in effectively transferring load between spine, pelvis, legs, and arms. From an anatomical point of view the following was noticed: In all preparations, the posterior layer of the thoracolumbar fascia covers the back muscles from the sacral region through the thoracic region as far as the fascia nuchae. At the level of L4–L5 and sacrum strong connections exist between the superficial and deep lamina. The transverse abdominal and internal oblique muscles are indirectly attached to the thoracolumbar fascia through a dense raphe formed by fusion of the middle layer (Adams & Dolan 2007) of the thoracolumbar fascia and both laminas of the posterior layer. This “lateral raphe” (Bogduk & Macintosh 1984; Bogduk & Twomey 1987; DeRosa & Porterfield 2007) is localized lateral to the erector spinae and cranial to the iliac crest. The superficial lamina of the posterior layer of the thoracolumbar fascia is continuous with the latissimus dorsi, gluteus maximus, and partly the external oblique muscle of the abdomen and the trapezius muscle. Cranial to the iliac crest, the lateral border of the superficial lamina is marked by its junction with the latissimus dorsi muscle. Barker and Briggs (2007) reported that the superficial lamina also has an attachment of variable thickness to the lower border of the rhomboid major muscle (Barker & Briggs 2007). In the pelvic region the deep lamina is connected to the posterior superior iliac spines, iliac crests, and the long posterior sacroiliac ligament (O’Rahilly et al. 1990). This ligament originates from the sacrum and attaches to the posterior superior iliac spines. The study presented here confirms some previous studies and disagrees with others. The bilaminar structure of the posterior layer of the thoracolumbar fascia has been described by Fairbanks, and O’Brien (1980), Gracovetsky (1990), Macintosh and Bogduk (1986), Bogduk and Macintosh (1984),and Bogduk and Twomey (1987). They describe the orientation of the fibers of the superficial and deep lamina as, respectively, caudomedial and caudolateral. The present study confirms the orientation of the laminae and their attachments. It is noteworthy that according to most studies (Fairbanks & O’Brien 1980; Bogduk & Macintosh 1984; Bogduk & Twomy 1987) the latissimus dorsi is mentioned as the significant structure from which fibers of the superficial lamina originate. The gluteus maximus as origin for the formation of the superficial fascia is ignored. Bogduk and Macintosh (1984) state that fibers located caudally from L3 decussate to the contralateral site, although it was not possible to trace the precise origin of these fibers because of strong fusion to midline structures. The present study confirms the phenomenon of crossing fibers. The level of the crossing varies from L2–S2. In contrast to the study of Bogduk and Macintosh, no connections were found between the serratus posterior inferior and the superficial lamina: Its fascia is exclusively connected to the deep lamina. Bogduk and Macintosh (1984) and Bogduk and Twomeny (1987) describe the deep lamina as a structure consisting of bands of collagen fibers extending from the lumbar spinal processes to the iliac crest and lateral raphe. However, we can not confirm the existence of bands of collagen fibers; we find a continuous layer. The authors pay no attention to the sacral part of the deep lamina. As a consequence, the connections with the sacrotuberous ligaments are omitted. Therefore the biomechanical model as proposed by Bogduk and Twomey (1987) is incomplete. The bracing effect of the thoracolumbar fascia on the lower lumbar spine and SI joints, essential for proper load transfer between spine and legs (Snijders et al. 1993a,b), can only be adequately described if the caudal part of the thoracolumbar fascia is included.
An integrated functional view of the anatomy of the TLF and coupled structures
Introduction
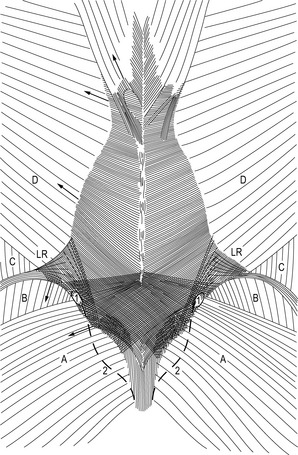
Superficial lamina (Fig. 1.6.1)
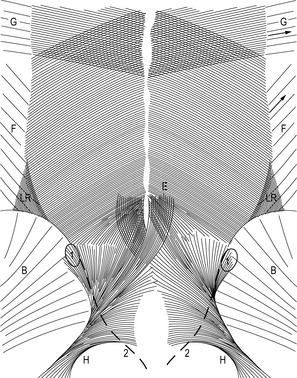
Deep lamina (Fig. 1.6.2)
Kinematics
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree