The Sural Artery Flap
Michael Sauerbier
Thomas Kremer
Indications/Contraindications
Soft tissue defects of the lower one-third of the leg and the calcaneal region remain crucial issues. This area is easily susceptible to trauma, and defects of this area are commonly experienced in orthopaedic and trauma surgery.
This region is characterized by tightness and limited mobility of the skin and, frequently, by poor circulation. Thus, chronic and diabetic ulcers, pressure sores, unstable scars, or chronic infection following Achilles tendon rupture or trauma surgery often occur in the distal parts of the leg. Furthermore, exposure of viable structures such as neurovascular bundles, tendons, bone, or osteosynthesis material is a common clinical occurrence due to the superficial course of these structures in the lower one-third of the leg.
In these patients, vascularized soft tissue reconstruction is necessary if further soft tissue damage, with subsequent infection and a potential risk of osteitis, is to be prevented. Relatively few procedures for cutaneous coverage have demonstrated real effectiveness and an acceptable morbidity. In recent years, free microvascular tissue transplantation has become a reliable option among patients suffering from acute or chronic defects in the lower one-third of the leg. Free flaps such as the gracilis flap or the latissimus dorsi flap, as well as fasciocutaneous flaps (e.g., anterolateral thigh flap, parascapular flap, lateral arm flap, and free groin flap) are frequently performed for limb salvage. Despite the fact that free microvascular transplantation possesses the disadvantages of extensive surgery, sophisticated equipment, general anesthesia, and high costs, this procedure often remains the only option for reconstruction of large defects in this region for limb salvage (Fig. 29-1).
For the coverage of smaller defects, alternative options such as pedicled flaps (e.g., flexor digitorum communis flap, medial plantar flap, [hemi-] soleus muscle flap, abductor hallucis flap, peroneal brevis flap, and lateral supramalleolar flap) have been developed (Table 29-1). In 1992, Masquelet et al. published their experimental work involving skin island flaps supplied by the vascular axis of sensitive superficial nerves. The distally based sural artery flap, which is perfused by reverse flow through the anastomosis between the superficial sural artery and the lowermost perforator of the peroneal artery, forms part of this group. One of the advantages of this thin fasciocutaneous flap is that it permits skin coverage with ideal contouring. Other advantages are that it can be performed quickly, the soft tissue coverage is durable, postoperative discomfort and donor site morbidity are minimal, and it is unnecessary to sacrifice major vessels. This flap has been used for the successful coverage of defects of the posterior and inferior surface of the heel, the Achilles tendon, the middle and distal one-third of the leg, and the dorsum of the foot and the lateral—as well as medial—malleolus (Tables 29-2 and 29-3; Figs. 29-2,29-3,29-4).
The sural artery flap is insensate and is not an option in cases in which sensitivity is an issue. Furthermore, the sacrifice of the sural nerve results in hyposensitivity of the lateral border of the foot.
Because perfusion of large sural artery flaps (> 9× 12 cm) is unreliable, it is not deemed suitable for coverage of extensive defects of the lower one-third of the leg. Moreover, higher complication rates have to be anticipated in patients with comorbidities such as peripheral artery disease, diabetes mellitus, and venous insufficiency. The sural artery flap is contraindicated in patients with destruction of the vascular pedicle or the lowermost perforator of the peroneal artery (see Table 29-2).
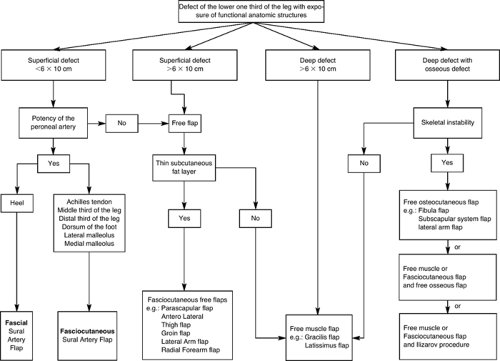 FIGURE 29-1 Treatment algorithm. Small superficial defects of the lower one-third of the leg can be treated by a sural artery flap if the defect size is smaller than 6 × 10 cm. Larger superficial defects can be reconstructed by fasciocutaneous free flaps, whereas deep defects, especially in combination with osseous, defects should be reconstructed by muscle flaps. Defects in the weight bearing area of the heel should be reconstructed by fascial sural artery flaps to prevent pathologic movement of the subcutaneous layer. For alternative pedicled flaps to the lower limb, see Table 29-1. |
Table 29-1. Flaps and Their Indications According to Location | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 29-2. Advantages and Disadvantages of the Sural Artery Flap | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 29-3. Indications for Sural Artery Flap Reconstruction | |
|---|---|
|
Preoperative Planning
A thorough clinical and radiologic examination of the donor and the recipient sites is mandatory, and it is first necessary to estimate the size of the recipient site defect. There are no studies regarding maximum flap dimensions with regard to safety, but small and moderate-sized defects can usually be covered satisfactorily. Defects up to 9 × 12 cm have been successfully reconstructed using sural artery flaps. Radical debridement may result in an enlargement of the defect, and this should be taken into account in the preoperative planning.
An examination of the patient’s peripheral function should be performed to determine the total extent of the injury. Depending on the size and location of the defect, various functional structures may be exposed or destroyed. Changes in the normal resting position of the foot and toes will help identify the loss of continuity of lower extremity tendons, and traditional functional tests will confirm the loss of active range of motion. A careful examination of sensitivity and muscle function helps to evaluate the extent of the defect in terms of destruction of sensor or motor nerve components. Additionally, peripheral perfusion should be ascertained by simple palpation of pulses or by Doppler probe. If in doubt, an angiogram should be performed. If any of these structures have been destroyed, additional reconstruction procedures must be planned. In patients suffering from chronic or infected wounds or diabetic gangrene, additional osteitis or osteomyelitis must be considered and conventional radiographs and/or magnetic resonance imaging (MRI) scans can help to prove the existence or extent of altered osseous structures.
Table 29-4. Preoperative Planning for Sural Artery Flap Reconstruction |
|---|












