The Rotator Cuff
Richard K.N. Ryu MD
Graham R. Hurvitz MD
The majority of symptomatic rotator cuff disease patients respond to a nonoperative program emphasizing the restoration of normal biomechanics, unrestricted motion, and functional force couples.
Early surgical management should be considered for acute rotator cuff tears in physiologically young and very active individuals.
The ability to recognize the complex layered anatomy in addition to the tear configuration is critical if an anatomic repair is to be achieved.
The rotator cuff muscles centralize the humeral head and permit a single center of rotation while providing stability and strength. During active shoulder elevation, the rotator cuff muscles depress the humeral head, allowing efficient elevation of the extremity.
When surgery is necessary, the goal should be to properly and anatomically restore the balanced forces of the supraspinatus and deltoid muscles so that their counteraction is maintained.
Tearing of the rotator cuff as a function of age is a common occurrence. Many of these tears may be clinically silent.
Mechanical impingement is the most common recognizable source of recurring rotator cuff pain and disability in the active population. When impingement-type symptoms present in a younger patient, great care must be taken to avoid overtreating because the impingement may be internal or may be secondary to instability which effectively moves the cuff closer to the arch.
The unaffected shoulder can serve as a “normal” template for comparison during physical examination. One should survey for atrophy or asymmetry, especially in the supra- and infraspinatus fossae. Long-standing rotator cuff tears are often accompanied by significant, visible atrophy.
The initial evaluation of the painful shoulder should include quality plain radiographs. The standard radiographs should include a true anterior-posterior view with the shoulder in the internal and neutral position, an axillary view and the outlet (supraspinatus) view described by Neer and Poppen which is used to evaluate and classify acromial morphology and arch anatomy.
Magnetic resonance imaging (MRI) is the test of choice when evaluating the soft tissues of the shoulder. T1 weighted images revealing increased signal in the rotator cuff, combined with a focal defect or loss of continuity of the cuff on the T2 weighted image, is a common finding when a full or partial-thickness tear is encountered.
MRI scans for those anticipating shoulder surgery can be helpful in evaluating tears, assessing possible atrophy, and establishing the presence of co-morbidities.
Injuries to the rotator cuff occur commonly. Treatment for these common disorders is most effective when a management algorithm can be developed based on a keen understanding of pertinent anatomy, pathology, and outcomes studies supporting specific treatment. Suffice to say that the majority of patients with symptomatic rotator cuff disease respond to a well-planned, nonoperative program emphasizing the restoration of normal biomechanics, unrestricted motion, and functional force couples. Clearly there will be
those patients in whom the pathology has progressed to a point where surgical intervention may be appropriate.
those patients in whom the pathology has progressed to a point where surgical intervention may be appropriate.
This chapter is organized into three sections: The first details the anatomy, biology, function, and pathoanatomy; the second section focuses on the physical exam and diagnostic testing; the final section considers treatment alternatives and selected techniques.
Anatomy and Biology
The rotator cuff consists of the supraspinatus, infraspinatus, teres minor, and subscapularis muscles, all of which arise from the scapula and insert into the proximal humerus. The subscapularis muscle is innervated by the upper and lower scapular nerves, and arises from the anterior surface of the scapula, inserting into the lesser tuberosity. The nerve supply to the supraspinatus is provided by the suprascapular nerve, and the muscle originates from the supraspinatus fossa, inserting into the greater tuberosity. The infraspinatus muscle is also innervated by the suprascapular nerve after it passes around the spinoglenoid notch. The muscle arises from the infraspinatus fossa and inserts into the posterolateral aspect of the greater tuberosity. The axillary nerve innervates the teres minor, which originates from the inferior and lateral aspect of the scapula, inserting into the inferior portion of the greater tuberosity.
Another important and under appreciated feature of the rotator cuff is its distinct layered makeup (1,2,3). The first layer is a superficial one extending from the coracoid process to the greater tuberosity following the course of the coracohumeral ligament. The second layer consists of the supraspinatus and infraspinatus tendinous fibers. Layer three is composed of the same muscle groups, but the fibers are oriented obliquely and interconnect with the adjacent rotator cuff fibers including the subscapularis. The deep fibers of the coracohumeral ligament make up the fourth layer extending into the supraspinatus and infraspinatus junction laterally. Layer five represents the actual capsular layer of the joint. The ability to recognize the complex layered anatomy in addition to the tear configuration is critical if an anatomic repair is to be achieved. Furthermore, collagen organization is more robust on the bursal aspect of the rotator cuff as compared to articular-sided fibers (4,5), a pertinent fact when evaluating partial thickness tears. It is also worth noting that a significant contribution to the vascular environment of the rotator cuff, when considering healing potential, may arise from adjacent subacromial structures including the bursa (6,7).
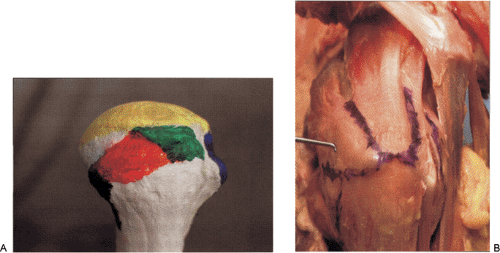
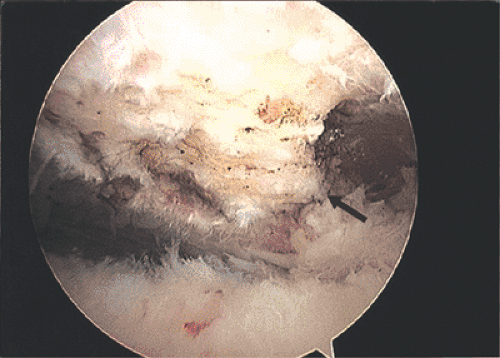
Investigators have further refined the insertional anatomy of the rotator cuff components (8,9). Each segment of the rotator cuff has a specific “footprint” that can be quantified. This is particularly important when assessing partial thickness cuff tears (Fig 13-1). The depth of the tear, as judged by the amount of exposed “footprint,” allows the clinician to not only estimate the severity of the tear, but to also choose the most effective treatment (10,11,12).
The vascular anatomy of the rotator cuff has been well described. The anterior humeral circumflex, the subscapular, and the suprascapular arteries provide the primary blood
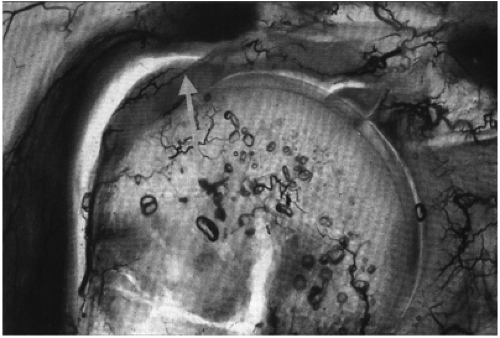
supply to the rotator cuff (13,14,15). Lindblom has described an area of avascularity in the supraspinatus tendon proximal to its insertion into the greater tuberosity (16,17) (Fig 13-2). Other authors have reported a dynamic reason for the decreased vascularity within the supraspinatus tendon, citing a “wringing out” effect with supraspinatus tension (18). Benjamin (19) described the histological transition that takes place from tendon to calcified fibrocartilage to bone, accounting for the vascular differences at the insertion site. The zone of uncalcified fibrocartilage is more avascular with respect to the other zones and may be vulnerable to delayed or incomplete healing when traumatized.
supply to the rotator cuff (13,14,15). Lindblom has described an area of avascularity in the supraspinatus tendon proximal to its insertion into the greater tuberosity (16,17) (Fig 13-2). Other authors have reported a dynamic reason for the decreased vascularity within the supraspinatus tendon, citing a “wringing out” effect with supraspinatus tension (18). Benjamin (19) described the histological transition that takes place from tendon to calcified fibrocartilage to bone, accounting for the vascular differences at the insertion site. The zone of uncalcified fibrocartilage is more avascular with respect to the other zones and may be vulnerable to delayed or incomplete healing when traumatized.
The subacromial arch is defined as the space between the distal clavicle and acromion superiorly and the humeral head inferiorly. This space between the acromion and humeral head averages 8 to 12 millimeters on plain x-ray, and can be further divided into the coracoacromial arch which is formed by the acromion, coracoacromial ligament and the coracoid process. As the rotator cuff passes beneath this arch, contact between the tendons and the arch can occur, leading to tendon pathology as well as secondary changes to the arch in the form of traction-based ossification within the coracoacromial ligament at the acromial attachment site (20,21,22,23,24,25,26) (Fig 13-3).
Function
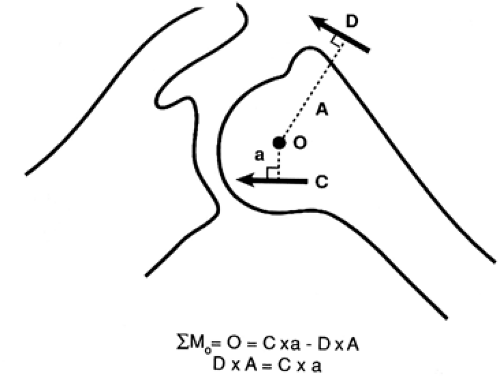
The rotator cuff muscles centralize the humeral head and permit a single center of rotation while providing stability and strength. During active shoulder elevation, the rotator cuff muscles depress the humeral head, allowing efficient elevation of the extremity while the head remains reduced in the glenoid (27,28,29,30). Studies have been performed evaluating the individual rotator cuff muscles and their respective contribution to shoulder strength. The supraspinatus and infraspinatus provide approximately 45% of abduction strength and the infraspinatus contributes nearly 90% of external rotation power (31,32). The supraspinatus and deltoid muscles provide balancing forces in the coronal plane of motion (33) (Fig 13-4).
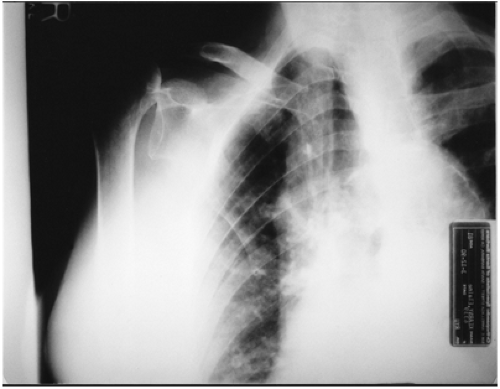
 Fig 13-3. Radiograph of subacromial outlet reveals sharp, bony excresence (arrows) originating from coracoacromial ligament attachment site. |
The importance of balanced force couples cannot be overemphasized, and the goal of surgery, when necessary, should be to properly and anatomically restore these forces
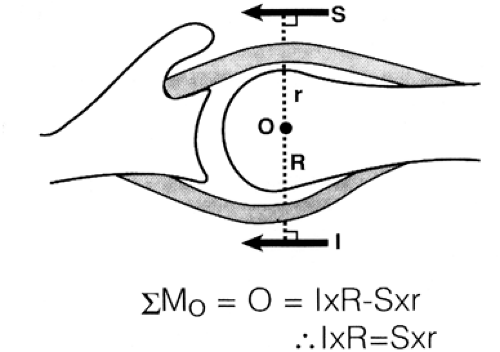
such that their counteraction is maintained. Furthermore, the importance of the transverse force couple and the need for balanced function in this plane was further emphasized by Burkhart (34,35,36,37,38) (Fig 13-5). Loss of greater than half of the infraspinatus or loss of subscapularis function leads to superior humeral head migration, a phenomenon often detected on plain films as the acromial-humeral head distance diminishes to less than 7 millimeters (Fig 13-6).
such that their counteraction is maintained. Furthermore, the importance of the transverse force couple and the need for balanced function in this plane was further emphasized by Burkhart (34,35,36,37,38) (Fig 13-5). Loss of greater than half of the infraspinatus or loss of subscapularis function leads to superior humeral head migration, a phenomenon often detected on plain films as the acromial-humeral head distance diminishes to less than 7 millimeters (Fig 13-6).
If the coronal and transverse force couples remain functional and balanced, the end result is a properly centered humeral head and surprisingly good function even if a significant, possibly irreparable tear is present. Burkhart remains a pioneer in helping us recognize that torn rotator cuffs can be very functional and that attempting to “cover the humeral head” utilizing nonanatomic tissue re-approximation is an approach that must be avoided (35). Burkhart’s concept of partial repairs in an effort to restore force couples has been successfully applied in lieu of tendon transfers that may serve only to weaken the balanced force couple (36,37,38,39,40).
 Fig 13-6. Loss of interval between humeral head and acromion indicates massive rotator cuff tear and compromised humeral head containment. |
Although there has been speculation that the biceps serves as a humeral head depressor and maintains an active role in shoulder function, comparative anatomic studies (41) as well as electromyographic data indicate that the biceps probably does not function as a humeral head depressor (42), and that the hypertrophy often encountered in the massive rotator cuff tear may be inflammatory in origin (43) as opposed to a reflection of intrinsic strengthening (44). There is some evidence from EMG studies that the biceps may serve as an additional shoulder stabilizer in those with anterior shoulder instability (45,46).
Pathoanatomy
Before describing the mechanics of rotator cuff pathology, post-mortem studies provide an interesting backdrop to the issue of etiology. There is little doubt that rotator cuff tearing is a function of age among other factors. Post-mortem studies have indicated an incidence of full or partial thickness tears ranging from 5% to nearly 40% (47,48,49,50,51). Fukuda et al. (52) reported a 13% incidence of partial rotator cuff tears in a cadaveric study of 249 anatomic specimens. The prevalence of these partial thickness tears appears to increase with age. DePalma (53) studied 96 shoulders of patients aged 18 to 74 years without a history of shoulder dysfunction and found an incidence of partial ruptures of the supraspinatus tendon in 37%. Petersson (54) reported on 27 asymptomatic patients ranging from 55 to 85 years of age with a nearly 50% incidence of full or partial thickness tears based on arthrographic studies. Suffice to say that tearing of the rotator cuff as a function of age is clearly a common occurrence. Furthermore, many of these tears, both full thickness and partial, may be clinically silent (10,49,55). As clinicians, we must be cautious in attributing causation to findings detected during diagnostic testing as these results may simply reflect the senescence process without significant clinical sequelae.
After a tear is noted, its natural history deserves attention. Several authors have reported on the progression of partial to full thickness tears (49,56,57). There is also evidence that full thickness tears are unable to heal spontaneously although an ineffective healing response may occur (58,59). Codman (60) believed that spontaneous healing of partial tears might occur, yet histological studies of partial thickness rotator cuff tears has yielded no evidence of active repair (61). Yamanaka (56) studied 40 patients with symptomatic articular-sided partial rotator cuff tears treated nonoperatively with serial arthrography. Repeat arthrography revealed that 10% of the tears had presumably healed, 10% had decreased in size
while enlargement of tear size occurred in 51%, and 28% progressed to a full thickness tear. A study comparing operative and nonoperative treatment for full-thickness rotator cuff tears concluded that larger rotator cuff tears in older individuals most likely progress in size although they can remain clinically quiescent (48). The study also concluded that the results of rotator cuff repair are clearly superior to that achieved with nonoperative measures only.
while enlargement of tear size occurred in 51%, and 28% progressed to a full thickness tear. A study comparing operative and nonoperative treatment for full-thickness rotator cuff tears concluded that larger rotator cuff tears in older individuals most likely progress in size although they can remain clinically quiescent (48). The study also concluded that the results of rotator cuff repair are clearly superior to that achieved with nonoperative measures only.
In a compelling longitudinal study of the natural course of rotator cuff tears, Yamaguchi et al. (49) reported on the risk of progression of asymptomatic rotator cuff tears detected by ultrasound in 58 patients with unilateral symptoms and bilateral rotator cuff tears. Fifty-one percent of asymptomatic tears became symptomatic over a three-year follow-up period. Nine of 23 patients restudied with ultrasound clearly demonstrated an increase in tear size, and no patient showed evidence of healing.
Etiology
When considering the possible causes of rotator cuff disease, mechanical impingement of the rotator cuff is considered the most common recognizable source of recurring pain and disability in the active population. Neer’s classic work (20,62) served to organize the clinician’s approach to rotator cuff disease and, most importantly, to define rotator cuff pathology as a spectrum of disease ranging from reversible edema to cuff fiber failure.
Primary impingement occurs at the anterior one third of the acromion and coracoacromial arch (24,63,64,65,66,67,68). The mechanical stresses endured by the rotator cuff, as well as its poor vascular design, both dynamic and static, have been well documented (13,14,15,16,17). Additional factors influencing rotator cuff pathology include acromial shape (20,22,24,69,70,71), slope (21,72,73,74,75), coracoacromial ligament size (76,77), postfracture deformity, os acromiale (78,79,80,81,82) and acromioclavicular joint spurring (24,83). Snyder (72) has recently reported on the “keeled” acromion, a particularly pernicious acromial variant associated with rotator cuff injury.
Functional abnormalities, such as asynchronous shoulder motion, posterior capsular contractures, scapular dyskinesia, glenohumeral instability, and distant neurological injury leading to weakness can also adversely affect the rotator cuff on a secondary basis with increased impingement forces concentrated in the subacromial space (84,85,86,87).
Impingement may occur from a direct mechanical insult, usually the result of an acromial excrescence excoriating the bursal aspect of the rotator cuff (Fig 13-7). However, another plausible injury cascade begins with intrinsic cuff failure, leading to insufficient humeral head depression and subsequent superior migration with creation of a traction spur within the coracoacromial ligament as a secondary phenomenon (24,26,68,71). The cause for intrinsic cuff failure can range from fatigue on an overuse basis to underlying shoulder instability or superior labral pathology, injuries that have been associated with internal impingement and articular sided cuff failure (88,89,90,91,92,93). Regardless of etiology, a narrowed or stenotic supraspinatus outlet poses continued risk to the rotator cuff.
History
Rotator cuff disease, especially that related to the impingement phenomenon, is usually evident from the history alone. A painful range of motion beginning at 70 degrees of forward flexion through 120 degrees is commonplace with pain localizing to the anterior-superior shoulder, often radiating down the lateral upper arm into the deltoid insertion. Overhead activities are the most provocative, and in instances where the rotator cuff has actually torn, night pain and difficulty sleeping are common complaints. Motion is usually not restricted, other than that due to pain; however, for longer standing injuries, a secondary adhesive capsulitis pattern can be encountered, especially in the older population. Most often the onset of pain is insidious and takes place over a longer period of time, but for those with an acute injury, a tearing sensation associated with profound early weakness may be the presenting history.
Because rotator cuff disease reflects a spectrum of pathology, the history and physical findings may overlap. There may be little difference in the presentation and findings of patients with isolated impingement, partial and even small full thickness rotator cuff tears.
Physical Examination
After completing a detailed history, a focused examination can be undertaken. It is critical to compare extremities as the unaffected shoulder can serve as a “normal” template to
which one can compare. One should survey for atrophy or asymmetry, especially in the supra and infraspinatus fossae. Long-standing rotator cuff tears are often accompanied by significant, visible atrophy. Examination should include assessment of range of motion, both active and passive, observing forward flexion, abduction in the scapular plane, internal rotation, and external rotation both in abduction and with the elbow at the side. Careful evaluation of scapular tracking should be included as poor scapulo-thoracic mechanics can lead to secondary subacromial pathology. In some instances of suspected impingement, simply treating scapular dyskinesia can alleviate secondary subacromial space symptoms (84,86,87). Strength testing should be performed in an attempt to isolate the different components of the rotator cuff to assess weakness. The “lift-off” test can help to assess subscapularis integrity (94) (Fig 13-8).
which one can compare. One should survey for atrophy or asymmetry, especially in the supra and infraspinatus fossae. Long-standing rotator cuff tears are often accompanied by significant, visible atrophy. Examination should include assessment of range of motion, both active and passive, observing forward flexion, abduction in the scapular plane, internal rotation, and external rotation both in abduction and with the elbow at the side. Careful evaluation of scapular tracking should be included as poor scapulo-thoracic mechanics can lead to secondary subacromial pathology. In some instances of suspected impingement, simply treating scapular dyskinesia can alleviate secondary subacromial space symptoms (84,86,87). Strength testing should be performed in an attempt to isolate the different components of the rotator cuff to assess weakness. The “lift-off” test can help to assess subscapularis integrity (94) (Fig 13-8).
 Fig 13-8. Lift-off test evaluating integrity of the subscapularis. May be difficult position to achieve in patients limited by pain and motion restrictions. |
Although clinically useful, placing the arm in the testing position can be provocative and difficult to achieve, especially in the older population. The “belly-press” test (or Napolean sign) can also help determine integrity of the subscapularis, is less provocative than the “lift-off” test and can actually be quantified to assess partial tears as well (95,96) (Fig 13-9).
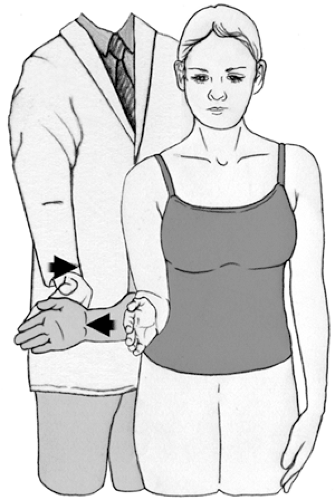 Fig 13-10. External rotation testing evaluates infraspinatus and teres minor integrity. Weakness indicates loss of posterior transverse force couple. |
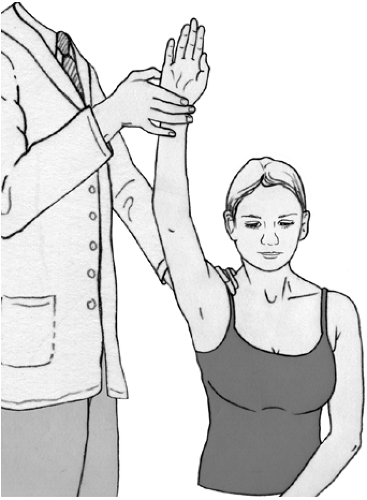 Fig 13-12. Neer sign for impingement. Neer test utilizes the same maneuver following a subacromial injection of anesthetic. Amelioration of pain confirms diagnosis of impingement. |
Resisted external rotation with the elbow by the side is useful in detecting tears extending into the infraspinatus (Fig 13-10).
This manual test is critical for assessing the posterior transverse force couple while the “belly-press” test determines subscapularis function. If significant weakness is noted in either or both muscle groups, loss of humeral head containment is imminent if not already present. Loss of the normal distance between the humeral head and acromion should be evident, and one must proceed with great caution if a decompression is undertaken. Violation of the arch in conjunction with inadequate transverse force couples may ultimately lead to erosion of the acromion by the humeral head and subsequent anterior-superior humeral head migration (97,98,99) (Fig 13-11).
This manual test is critical for assessing the posterior transverse force couple while the “belly-press” test determines subscapularis function. If significant weakness is noted in either or both muscle groups, loss of humeral head containment is imminent if not already present. Loss of the normal distance between the humeral head and acromion should be evident, and one must proceed with great caution if a decompression is undertaken. Violation of the arch in conjunction with inadequate transverse force couples may ultimately lead to erosion of the acromion by the humeral head and subsequent anterior-superior humeral head migration (97,98,99) (Fig 13-11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree