Chapter 7. The principles of managing trauma
Fractures
Trauma and fractures are not the same thing. When a limb is broken, every tissue in it is damaged. The fact that the bony injury is the only one visible on the radiograph does not make it the most serious. Radiographs do not show severed nerves, crushed muscles, ruptured blood vessels or torn ligaments, any more than they tell whether a wound is contaminated, how the injury occurred or how it should be treated.
The severity of an injury is greatly influenced by the violence of the impact. A leg broken by a car travelling at 95 km/h (60 m.p.h.) will be more seriously injured than one broken by tripping over the cat (Fig. 7.1). In the high speed injury there will be damage to all the soft tissues as well as bone, and possibly damage to the blood vessels. The bone ends will be crushed and devitalized, nerves stretched or severed, and muscles crushed. Although the bone may unite soundly and in good position, so that it is even stronger than before the injury, damaged muscles cannot be restored, and severed nerves will never be the same, however meticulously they are repaired.
 |
| Fig. 7.1 Violence of impact. Cats cause less damage than cars. |
To understand the damage to the soft tissues, imagine the position of the limb at the moment of impact when the bone ends were widely separated (Fig. 7.2). By the time the patient reaches hospital, the soft tissues will have bounced back almost to their normal position and the radiographs give no indication of the extent to which the soft tissues were stretched. This is not a difficult concept, yet inexperienced casualty officers frequently decide how to treat a patient just by examining the radiograph and this can lead to disaster.
 |
| Fig. 7.2 Displacement of fragments. Soft tissues recoil and pull bone fragments back together after an impact. Try to imagine how the fragments and soft tissues must have been at the time of greatest displacement. |
Even if the fracture is treated correctly in the accident department, soft tissue injuries can still spoil the result of the finest fracture management. This is easily forgotten when the patient is sitting in the fracture clinic with an injured limb hidden inside a cast. If the radiographs look normal it might be imagined that all that needs to be done for the limb to work normally again is to remove the cast. This is not so.
Fracture management can therefore be divided into three phases. Early management is directed to converting contaminated wounds to clean wounds, and the second stage to joining together those things that have broken, notably bone. The third stage consists of separating those things that have stuck together but should be separate, particularly muscles and joint surfaces.
There is no point in achieving a perfect radiograph with solid bone if the muscles cannot operate the joints. On the other hand, it is equally bad to start early rehabilitation and produce excellent muscles around a malunion. A balance must be struck between these two conflicting aims. The correct approach is to start mobilization and vigorous physiotherapy as soon as it is safe to do so, but to choose the right moment takes experience.
Recognizing a fracture
The physical signs of a fracture
• Abnormal movement in a limb due to movement at the fracture site.
• Crepitus or grating between the bone ends.
• A deformity that can be seen or felt.
• Bruising around the fracture.
• Tenderness over the fracture site.
• Pain on stressing the limb by bending or longitudinal compression.
• Impaired function.
• Swelling at the fracture site.
Although it is usually easy to know when a bone is broken, it is surprisingly easy to miss a fracture and some are notorious for the number of times they escape recognition.
If either of the first two signs on the list above are present, there is a fracture, but these signs are absent if the ends are impacted. Undisplaced fractures cause no deformity, bruising can take hours to appear and unconscious patients cannot report pain or tenderness.
The following fractures are often missed (Fig. 7.3):
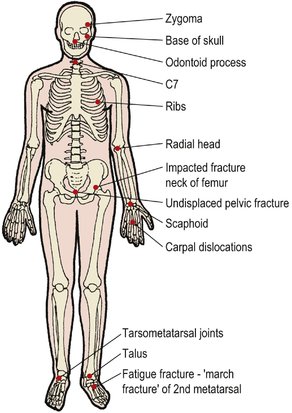 |
| Fig. 7.3 The fractures that most often escape diagnosis. |
1. Impacted fractures of the femoral neck.
2. Fractures of the ribs.
3. Fractures of the skull, particularly the base of the skull.
4. Facial fractures, particularly the zygoma.
5. Fractures of the radial head.
6. Fatigue fractures before the callus has appeared.
7. Fractures of the scaphoid.
8. Fracture dislocations of the carpus, particularly the lunate.
9. The seventh cervical vertebra.
10. Undisplaced fractures of the pelvis.
11. Fractures of the odontoid.
12. Fracture dislocations of the tarsometatarsal joint.
13. Fracture of the talus.
Natural history of fractures
Grass grows without gardeners and bones unite without orthopaedic surgeons. Like a gardener, the orthopaedic surgeon tries to make nature’s task easier, but nothing will ‘make’ a bone unite if the circumstances are not right.
Untreated, fractures can do one of several things. At best, they unite soundly in good position to give a perfect result, but they may be slow to unite ( delayed union), fail to unite at all ( non-union) or unite in the wrong position ( malunion) (Fig. 7.4).
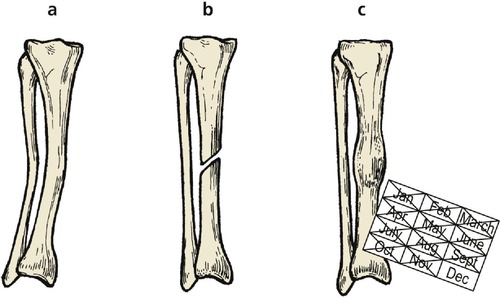 |
| Fig. 7.4 (a) Malunion; (b) non-union; (c) delayed union. |
There is no hard and fast rule to say how any one fracture will behave without treatment but, in general, fractures in cancellous bone unite soundly and non-union is seldom a problem, although there may be malunion. In contrast, the long bones are susceptible to non-union, particularly if there is poor blood supply to the bone ends as a result of extensive soft tissue damage.
Patients are, understandably, very eager to know how long their bone will take to join, but fractures unite gradually and the question ‘Has the fracture joined yet?’ is impossible to answer. A bone is only united when it is strong enough to take its normal load; this varies from bone to bone, but a good rule of thumb is to say that most bones join in 8 weeks, lower limb bones take twice as long and fractures in children take half as long.
A very rough guide to fracture healing
Bones join in 8 weeks, but double this in the lower limb and halve it for children.
Fracture healing
The healing of bone explains the clinical behaviour of a uniting fracture. Immediately after the fracture the bone ends rub together and cause crepitus, which is distressing to the patient. After about 14 days, fibrous tissue has replaced the blood clot between the bone ends and the crepitus ceases but the fracture remains mobile.
At about 4 weeks the fracture becomes ‘sticky’ and movement is less obvious. During the next 2 months the bone becomes solid but not always strong enough to do all that is asked of it, particularly if it is a weight-bearing bone in the lower limb.
As healing proceeds, the mass of tissue around the fracture becomes hard and produces a fusiform callus. Patients are often alarmed by the swelling and think they have cancer. They must be reassured that it is a sign of good fracture union. The callus never disappears completely but becomes smaller with time as the soft tissue swelling around it diminishes and remodelling occurs.
Malunion
The term malunion is applied to a bone that has united soundly but in the wrong position (Fig. 7.5). This sounds alarming but does not always matter greatly. Fractures of the clavicle almost always unite with a little shortening and overlap, which is quite acceptable and does not affect the functional result, but in fractures where the fragments are pulled apart by the unopposed action of different muscle groups, the functional result of malunion is poor.
 |
| Fig. 7.5 Non-union, malunion and cross-union. This patient had non-union of the tibia, malunion of the fibula and cross-union between the two. |
Cross-union. Cross-union, in which two adjacent bones become linked by new bone, is a variety of malunion. Cross-union in the forearm blocks pronation and supination.
Non-union
If the healing process fails, the bone ends do not unite and remain separate. This is a serious problem in a weight-bearing bone but may cause less disability in other situations, such as a fractured metacarpal. Two types of non-union are seen: (1) hypertrophic, and (2) atrophic.
Hypertrophic non-union is characterized by a massive cuff of bone around the ends of the fractures that looks a little like an elephant’s foot (Fig. 7.6a). These fractures are trying desperately to heal and can be helped to do so by realigning the limb and preventing movement between the bone ends. Prevention of movement can be done by rigid internal fixation, or intramedullary or extramedullary stabilization.
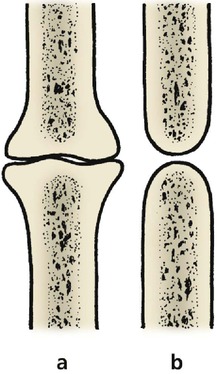 |
| Fig. 7.6 Shape of bones in (a) hypertrophic non-union and (b) atrophic non-union. |
Atrophic non-union shows rounding of the bone ends (Fig. 7.6b), sometimes so marked that the tips of the bone ends resemble pencils, and the medullary cavity may be closed. This is indicative of a poor blood supply to the bone ends.
A pseudarthrosis forms in some patients (Fig. 7.7). If there is no sign of osteogenesis, treatment must aim to ‘kick start’ this by bone grafting with fresh cancellous bone or marrow.
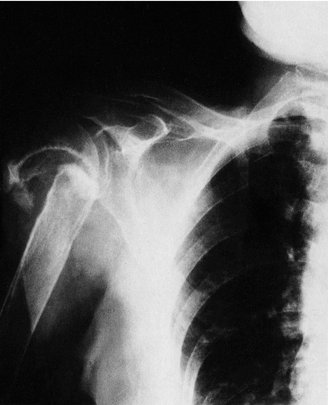 |
| Fig. 7.7 Non-union of a fracture of the surgical neck of the humerus. A pseudarthrosis has formed at the site of the fracture. |
Delayed union
A fracture with delayed union takes longer to unite than normal but eventually does so. It is important to distinguish delayed union from non-union, as delayed unions will unite with time and attention to correct immobilization of the fracture fragments. Non-unions, however, may need operative intervention in order to allow the bone ends to unite. Separation of the two types can be difficult. Unless there are positive signs of non-union, such as closing of the medullary cavity of the fragments, which makes the diagnosis easy, or an improvement between one radiograph and the next, diagnosis rests on comparing the rate of bone union with the normal rate of healing of a fracture in the same situation.
Classification of fractures
Simple and compound
Fractures can be classified in many ways but the simplest and most practical was the ancient classification of the old military surgeons who regarded all fractures as simple or compound.
Open and closed
Modern treatment of ‘compound’ fractures is so effective that the term is no longer applicable. Apart from this, fractures with intact skin can be far from ‘simple’ to treat and ‘compound’ may be confused with complicated, comminuted or multiple. ‘Simple’ and ‘compound’ have been replaced by ‘ closed’ and ‘ open’ but ‘compound’ is sometimes used to describe how the skin has been damaged (Fig. 7.8). A fracture in which the skin has been penetrated by a bone fragment from inside the leg is sometimes referred to as ‘compound from within’ to distinguish it from a true open fracture and to emphasize the potential danger.
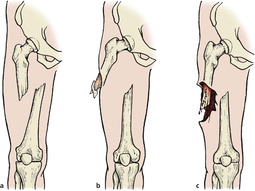 |
| Fig. 7.8 Open and closed fractures: (a) closed fracture; (b) ‘compound from within’; (c) an open fracture with contamination. |
Shape
Fractures can also be classified according to the shape of the fragments and this is helpful in deciding management (Fig. 7.9).
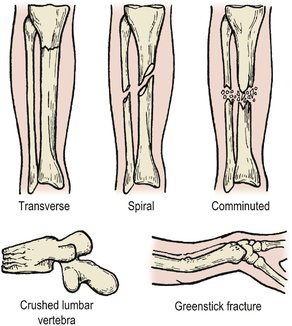 |
| Fig. 7.9 Patterns of fracture. |
Transverse fractures are the result of a direct blow or a pure angular force applied to the bone. The shape of the bone ends helps transverse fractures to stay aligned more easily than fractures which do not fit together so neatly.
Oblique or spiral fractures. Most long bone fractures are caused by a violent twisting movement about the long axis of the bone rather than the sideways bending which causes a transverse fracture. A sharp twist to the leg while the foot is stuck in a rabbit hole produces a spiral fracture of the tibia, even if radiographs suggest that the fracture line is oblique. In fact, oblique fractures are rare and are almost always a radiological artefact.
The fragments of a spiral fracture are more difficult to balance against each other than the square end of a transverse fracture and are very unstable. The bone spikes damage blood vessels, nerves or skin and the tips of the spikes can themselves break off to produce a triangular fragment known as a ‘butterfly’ fragment.
Crush fractures. A fracture in which cancellous bone is squashed or crushed presents a difficult problem because there are no fragments left to manipulate back into position. If the fracture site is opened up and the cortex of the bone replaced in its normal position, a large cavity remains and the bone can only be restored to its normal shape by packing the space with bone graft or holding the sides of the cavity apart by external fixation.
Crush fractures are typically seen in the lumbar vertebrae, tibial plateaux and calcaneum.
Greenstick fractures. When a green stick breaks, it does not snap cleanly but bends so that one ‘cortex’ buckles while the other remains intact. If the force is very great, one side may snap while the other remains intact – try it. If a green stick fractured in this way is straightened it bounces back slightly but will not hold its correct position.
Fractures of long bones in children behave in the same way. The compressed cortex first buckles to produce a ‘buckle’ fracture. If the force continues, the cortex under tension will fracture (Fig. 7.10). Because of the resilience of the bone, reduction is only possible if the fracture is made complete or if three-point pressure (p. 127) is applied. Fortunately, fractures in children remodel well enough to restore the normal anatomy and the deformity of most greenstick fractures can be accepted.
 |
| Fig. 7.10 A greenstick fracture of the radius with buckling of the dorsal cortex and a crack in the anterior cortex. |
Mechanism of injury
Fractures can be caused in several ways (Fig. 7.11).
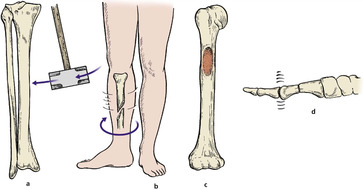 |
| Fig. 7.11 Mechanism of injury: (a) direct violence; (b) indirect violence; (c) pathological through a tumour; (d) fatigue. |
Direct violence
Bones can be broken by a direct blow and many patterns are seen. A sharp blow on the front of the knee may shatter the patella into many small fragments held together by soft tissue, like a boiled sweet broken in its wrapper (p. 254), but the fragments of a tibia fractured in a road traffic accident will be widely separated.
Indirect violence
More fractures are caused by indirect violence than direct violence. In this type of trauma, usually a twisting injury, no violence is applied to the site of the fracture itself. Open fractures are therefore uncommon, although the bone fragments can penetrate the skin from inside, making the fracture ‘compound from within’.
Pathological fractures
Pathological fractures occur through abnormally weak bone. Tumours, cysts and osteoporotic bone are common sites of pathological fractures (Fig. 7.12).
 |
| Fig. 7.12 Pathological fracture (a) through a metastasis in the humerus; (b) of the tibia through porotic bone. |
Fatigue fractures
Repeated small bending stresses will break any material (Fig. 7.13




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








