The Pediatric Athlete
Pierce M. Sherrill
This chapter is devoted to children, defined as those who have not finished their physical growth. Children are not miniature adults. They are growing—sometimes rapidly—while negotiating a complex landscape of physical, mental, social, emotional, and spiritual hurdles. Many are in puberty, which is second only to infancy in the amount of growth and development a child completes (1).
There is only one universal rule in treating sports injuries in children: “Tailor the process to the child’s specific needs.” Muscle, tendon, and ligament may become tight or lax as growth proceeds; this mandates changes in the standard exercise prescription. A child’s skeletal muscle responds differently to strength training; routine adult conditioning may do more harm than good to a child. Some injuries, such as apophysitis, only develop in the skeletally immature; others, such as osteochondrosis, develop differently in children.
DEMOGRAPHICS
The 2000 census reported 61,297,467 children aged 5 to 19 in the United States. They comprised 21.78% of the total population. Of these, 69.22% were white; 15.10%, African American; 3.45%, Asian; 1.17%, American Indian/Alaska Native; 0.18%, Hawaiian/Pacific Islander; 7.36%, other; and 3.52%, “two or more races.” There were slightly more males than females (2).
EPIDEMIOLOGY
The Centers for Disease Control and Prevention reports that almost 6 million high school students play team sports. Another 20 million participate in recreational or competitive sports outside the school setting. There are over 775,000 emergency department visits per year for sports injuries to children under the age of 15. Given the 41,077,577 children aged 5 to 14 in the 2000 census, this yields an annual incidence of 1.88% (3).
Gender and Racial Differences
There are distinct gender differences, and more subtle racial/ethnic differences in the kinds and mechanisms of injury in the pediatric population. Females participate in fewer sports involving contact, collision, or combat. Despite this, their injury rates approximate and sometimes exceed those of their male counterparts. Offer et al. (1) observe that many girls succumb to social pressures against vigorous exercise. This lack of conditioning contributes to injury risk. Females are also more likely to participate in appearancesensitive sports such as gymnastics, figure skating, and dance. These sports emphasize flexibility and slenderness over strength. This increases the risk for injuries such as spondylolisthesis and joint instability.
Girls enter puberty about 2 years earlier than boys. They begin their final growth spurt earlier, and their epiphyses close about 2 years earlier as well. As a result, girls have 2 years less growth than boys. Women are, in the aggregate, shorter in stature and have less muscle mass than men.
Girls have a wider pelvis, greater femoral anteversion, and more genu valgum. There is less vastus medialis development, and a greater incidence of patella maltracking. Girls also have more lumbar hyperlordosis, and a greater risk
for nutritional disorders. All of these factors increase a girl’s risk for musculoskeletal injury (4).
for nutritional disorders. All of these factors increase a girl’s risk for musculoskeletal injury (4).
Despite the earlier puberty, girls at age 16 average 75% of the strength of their male counterparts, and they have proportionately less muscle mass. However, Offer (1) observes that when girls engage in strenuous and vigorous exercise through childhood, they develop a magnitude of strength similar to that of boys. It is not yet clear how much of the observed difference is sociocultural, and how much is hormonal or developmental.
Racial and ethnic differences include sport of preference; method of training; emotional response to injury; social and family support; folklore about health, injury, and healing; and expectations for recovery.
UNIQUE ISSUES
Physical
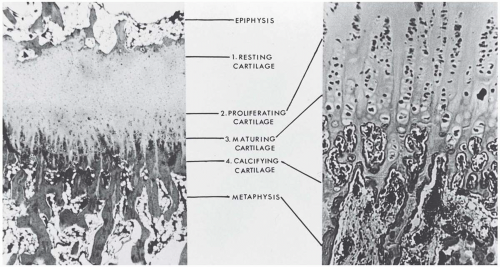
Children have open epiphyses, or bone growth plates. The epiphyses consist of uncalcified cartilage, and are the most fragile segment in the bone-joint-ligament-tendon-muscle complex (Fig. 44.1). Epiphyses are vulnerable to compressive and shear forces. In children, a joint sprain may actually be an epiphyseal fracture. It is critical to establish the appropriate diagnosis, since epiphyseal fractures carry the risk of premature closure and asymmetrical bone growth.
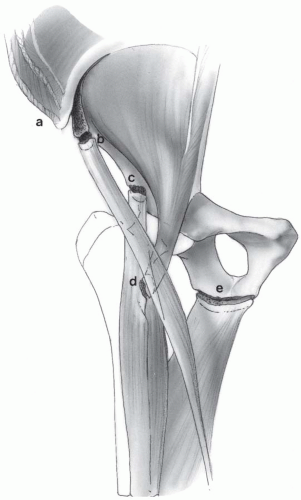
Similarly, children have apophyses. These tendon insertions into bone share many features of the epiphysis, but are most vulnerable to traction. During puberty, skeletal muscle increases in bulk and strength before its apophyseal insertion calcifies. If the strength of the muscular contraction exceeds that of its anchor, a traction injury (apophysitis) can result (Fig. 44.2).
Articular cartilage is softer in children; their subchondral bone resembles the epiphysis and is just as vulnerable to shear and compression injury. The injuries that produce chondromalacia in adults can cause subchondral fractures and osteochondritis dissecans in children (4). These injuries may need more aggressive management, including surgical débridement (5).
A child’s muscular strength, VO2max, and cardiac output are proportionately lower than an adult’s; however, surface area-to-body mass is greater in children (6).
Skeletal muscle in preadolescents does not hypertrophy in response to strength training. The strength gains achieved in children are the result of enhanced neuromuscular recruitment and motor-unit synchronization (5). Preadolescent weight training has also been shown to facilitate Wolff’s law of soft tissues, that is, the body’s tendency to remodel connective tissues along lines of greatest force (7). Prepubescent weight training (in a carefully supervised setting that emphasizes technique over power) can enhance late-adolescent strength gains. Once androgenic adult hormones appear, muscle hypertrophy can occur.
Social
More people are involved in the treatment of the pediatric athlete than the adult athlete. Permission to treat comes from parent or guardian, as does transportation to and from treatments. Parents and coaches may need to be included in return-to-play decisions. Also, they may have unreasonable expectations and may need more education than the athlete. Family, teammates, and coaches may need to help ensure compliance with treatment. On the other hand, these same people may provide conflicting advice or enable self-defeating behaviors.
The injured child will have evolving relationships with family, coaches, and peers. The injury may affect the child’s self-image, or social standing as a successful athlete. The injury may have impact on peer relationships within or outside the team.
Mental
The injured child will not have an adult’s comprehension of the injury. Erickson and Piaget each developed an outline for the stages of a child’s psychosocial development (3). Both note that the adult’s ability to deal with a complex issue such as an athletic injury develops relatively late in adolescence.
A child may see a painful procedure as punishment, or misconstrue the physical contact between caregiver and patient. Education and instructions may be misinterpreted or forgotten, especially if they conflict with what is heard from parents or coaches. Younger children may not believe the injury will heal.
Emotional and Spiritual
When injured and unable to compete, adolescents can respond with behaviors that are out of proportion to the actual injury (9). Most injured athletes go through a grief process like that described by Elizabeth Kübler-Ross (10) in her work with the dying patient. The denial, anger, bargaining, depression, and acceptance seldom follow a smooth, orderly progression: the patient may exhibit several stages at once, or become locked in one stage. Such behaviors may also need treatment.
Another normal coping technique in the pediatric athlete is regression, in which the child temporarily adopts behaviors from a younger age (11). What appears to be immaturity is actually healthy coping; it allows the child some emotional breathing room as he or she tries to deal with unfamiliar stresses.
Magical thinking can persist well into adolescence. Some children see their injury as punishment for a sin that is completely unrelated to the problem at hand. They may try to buy a cure with ritual behaviors. Children sometimes see the caregiver as an adult authority figure and rebel directly or passively-aggressively. Feelings of invulnerability increase the risk for injury in adolescents.
APPROACH TO THE PEDIATRIC ATHLETE
The basic precept in caring for the pediatric athlete is to tailor the process to the child’s specific needs, as previously mentioned. This process includes noting the patient’s stage of musculoskeletal development, and whether he or she has begun or ended a growth spurt.
Strength and flexibility imbalances need to be addressed in the treatment plan. The following points deserve mention:
Aggressive strength programs begun during a growth spurt may contribute to the injury, because they may aggravate tight muscle-tendon units (12).
Hypermobility in an adolescent may be present as the normal part of a growth phase, and does not in and of itself indicate somatic dysfunction.
If the hypermobility is truly pathologic, direct-action manipulation, or any technique that increases mobility in a hypermobile segment, is inappropriate (3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree