The Neuromuscular Hip
Kevin I. Perry
Miguel E. Cabanela
Rafael J. Sierra
Introduction
The hip joint is commonly affected in patients with neuromuscular disorders. As a result of muscle imbalance and the ensuing subluxation or dislocation of the hip joint, painful degenerative arthritis can develop that may ultimately require surgical intervention to improve function and relieve pain in these patients.
In general terms, the underlying etiology of the hip dysfunction may be due to either intrinsic or extrinsic factors. Intrinsic muscle imbalance about the hip occurs during childhood and plays a primary role in subsequent hip problems. Extrinsic causes of neuromuscular imbalance occur in stable hips that develop degenerative arthritis in later life. Muscle imbalance in these hips plays a secondary role. The muscle imbalance related to the presence of strong hip flexors and adductors that overpower weaker or absent hip abductors and extensors is the main reason leading to hip instability. However, soft tissue contractures about the hip and anatomic variations leading to coxa valga, increased femoral anteversion, and increased acetabular index also play a role in the pathogenesis of this disorder.
Patients who have a neuromuscular disease may need treatment for their hip disease for two general reasons: either the disease process (e.g., cerebral palsy (CP) or myelomeningocele) has led to dysplasia of the hip, which in turn has evolved into degenerative arthritis, or the degenerative joint disease has developed independently of the neurologic disease (e.g., Parkinson disease).
Neuromuscular conditions can be divided into two basic categories. The first type of muscle paralysis or paresis is flaccid paralysis or decreased muscle tone, in which the lower motor neurons or peripheral nerves are involved, and the second is spasticity or increased muscle tone, which involves the upper motor neurons or the cortex of the brain. Both flaccid and spastic types are found in intrinsic and extrinsic disorders. The first type includes conditions such as poliomyelitis, Down syndrome, myelomeningocele, and the second type includes conditions such as CP, Parkinson disease, and stroke. Most commonly in the young patient with a neuromuscular hip, successful containment of the hip can be achieved with various treatment modalities such as soft tissue releases, open reduction, femoral and acetabular osteotomies, or a combination of these procedures. If containment cannot be achieved and hip subluxation or dislocation occurs, hip reduction is not likely to result in pain relief. Cooperman et al. (1) have found that half of these hips become painful, most likely because the cartilage of the femoral head has degenerated and therefore management with a resection arthroplasty, arthrodesis, or total hip arthroplasty (THA) is frequently indicated.
In discussing the neuromuscular hip, certain differences between flaccid and spastic paralysis must be delineated. The spastic muscle has increased tone and often functions in both phases of gait. The flaccid muscle is paralyzed to a greater or lesser degree, but it always functions according to its normal role. Intact sensation is usually present in CP, but it may be diminished in adult patients who have suffered a cerebrovascular accident (CVA). Myelomeningocele patients have significant loss of sensation, whereas polio patients have intact sensation. Although diminished sensation itself plays no role in hip instability, its lack is an important consideration in planning surgery, as well as in the prognosis for the joint.
The purpose of this chapter is to review current surgical options in adult patients with neuromuscular hip problems, with a special emphasis on joint replacement, its planning, execution, and possible complications in this group of patients.
Patients with Increased Muscle Tone (Spasticity–Rigidity)
The major causes of spasticity are CP and spinal cord injuries in the child or young adult and CVAs, Parkinson disease, or neuropathic joints in the older patient.
Cerebral Palsy
Hip deformities in CP are second in frequency to talipes equinus. The incidence of hip subluxation/dislocation has been reported to be from 2.6% to 28% in different series (2,3). Hip dislocation/subluxation is more common with severe or total-body involvement. Deformities of the hip joint in patients with CP not only produce pain and prevent ambulation, but can also interfere with the patients’ sitting ability and hygiene in the most profoundly affected. As noted, the
direct cause of hip instability is muscle imbalance resulting from hip adductors and flexors overpowering the hip abductors and extensors. Femoral anteversion contributes to the problem, as does pelvic obliquity. Hip subluxation/dislocation generally occurs in the child with more severe involvement. Early surgical treatment during childhood consists of muscle releases to obtain balance, and early femoral varus rotation or acetabular osteotomies for containment of the femoral head. If early surgical intervention is not performed, the uncovered femoral capital epiphysis becomes deformed from the tremendous pressures subjected by the overlying capsule and spastic abductor muscles leading to painful arthritic changes in adolescents and adults.
direct cause of hip instability is muscle imbalance resulting from hip adductors and flexors overpowering the hip abductors and extensors. Femoral anteversion contributes to the problem, as does pelvic obliquity. Hip subluxation/dislocation generally occurs in the child with more severe involvement. Early surgical treatment during childhood consists of muscle releases to obtain balance, and early femoral varus rotation or acetabular osteotomies for containment of the femoral head. If early surgical intervention is not performed, the uncovered femoral capital epiphysis becomes deformed from the tremendous pressures subjected by the overlying capsule and spastic abductor muscles leading to painful arthritic changes in adolescents and adults.
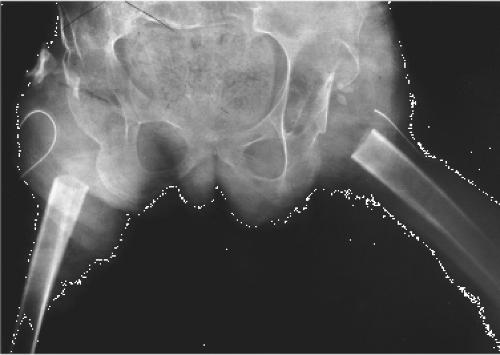
 Figure 74.1. Thirty-seven-year-old patient with spastic cerebral palsy. Patient has intractable pain in the left hip. |
In the adult patient, the aim of treatment is to prevent contractures that lead to hip subluxation or dislocation or if end-stage arthritis has occurred to eradicate pain in the affected arthritic joint (Fig. 74.1). Surgical options include resection arthroplasty or interposition arthroplasty, arthrodesis or total hip replacement arthroplasty.
Resection Arthroplasty
Resection arthroplasty needs to be very extensive to relieve pain and deformity reliably and, therefore, is reserved for patients who are unable to walk and whose functional needs might include improved hygiene and ease of positioning. However, the incidence of recurring pain and heterotopic bone formation and overall poor results has led many surgeons to abandon this procedure. McCarthy et al. (4) published the largest series to date in 1988. The authors reported the results of 58 proximal femoral resections in 34 patients, with ages ranging from 15 to 60 years. All of the patients in this study had severe arthritic hips. Pain was relieved and sitting improved in 33 of the 34 patients. Ectopic bone was noted in 53 hips. Only three hips required revision because of heterotopic bone formation. In 1978, Castle and Schneider (5) had also described an extensive proximal femoral resection with interposition arthroplasty with good long-term pain relief, improved sitting, and ease of perineal care in 12 patients (Table 74.1). In this operation, the proximal femur is resected below the lesser trochanter, the capsule is closed over the acetabulum with the detached end of the iliopsoas tendon, and the vastus lateralis is sutured over the stump of the proximal femur. The abductor muscle mass is interposed between the two (Fig. 74.2).
Koffman (8) reported in 1981 the experience at Rancho Los Amigos Hospital. Ten proximal femoral resections were performed in six severely disabled cerebral spastic patients. One of the six patients required a second resection and one other patient required insertion of a THA for continued pain. Almost all patients had heterotopic ossification (HO) and in a few the HOs were symptomatic and interfered with sitting.
Root and Bostrom reported in the first edition of this chapter on 15 proximal femoral resections done at the Hospital
for Special Surgery (HSS). The first three hips were treated with distal femoral skeletal traction, but because of difficulty in immobilizing these patients and significant knee flexion contractures, the authors abandoned skeletal traction in the postoperative period. Three of the 15 hips required revisions because of extensive heterotopic bone formation and pain. To prevent HO, the authors of this series treat all resections with 600 to 800 rads of radiation to the hip area on postoperative day 1, which has prevented significant heterotopic bone formation in these patients.
for Special Surgery (HSS). The first three hips were treated with distal femoral skeletal traction, but because of difficulty in immobilizing these patients and significant knee flexion contractures, the authors abandoned skeletal traction in the postoperative period. Three of the 15 hips required revisions because of extensive heterotopic bone formation and pain. To prevent HO, the authors of this series treat all resections with 600 to 800 rads of radiation to the hip area on postoperative day 1, which has prevented significant heterotopic bone formation in these patients.
Table 74.1 Interpositional Arthroplasty in Cerebral Palsy | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
Proximal femoral resection is contraindicated in ambulatory patients because the restored limb cannot bear weight. Resection also should not be performed in young, growing children because of upward migration and heterotopic bone formation in this group.
Hip Arthrodesis
Hip arthrodesis is an option that is rarely indicated. In ambulatory patients, THA is usually a more attractive option. Contraindications to hip arthrodesis include contralateral hip involvement and the presence of spine deformity. Many of the painful, dislocated hips occur in severely involved patients who have bilateral hip dysplasia as well as some degree of spinal deformity, thus ruling out hip arthrodesis as a surgical option (9).
In 2003 investigators at the Santa Casa Medical Hospital in Brazil reported on 14 patients (14 hips) with spastic CP and painful unilateral chronic hip dislocations or subluxations that were treated with hip arthrodesis and followed for a mean of 5.3 years (9). Four of these patients were diplegic ambulators and seven were bedridden. All had some form of internal fixation ranging from cancellous screws to rigid fixation with an AO-DCP 4.5-mm plate in six hips and the AO cobra plate in four hips. Eight hips had postoperative spica casting. The arthrodesis position was mean of 40 degrees of flexion (20 to 60 degrees), 15 degrees of abduction (0 to 52 degrees), and neutral rotation. Postoperatively, three patients with pseudoarthroses required a second procedure, but did eventually go on to union. The authors report that all patients were pain free at last follow-up. Functional status improved or remained the same in all patients. Five of seven bedridden patients became sitters and all preoperative ambulatory patients continued to ambulate in the community.
In 1986, Root et al. (10) reported on eight CP patients with ages ranging from 13 to 34 years who had unilateral hip arthrodesis. All of these patients had painful arthrosis of the hip associated with subluxation or dislocation. Of the original eight patients, six had successful fusions and two required revisions. One of the revisions was ultimately converted to a total hip replacement.
The advantages of a successfully arthrodesed hip are elimination of pain, the ability to sit and stand, and long-term durability. The disadvantages are the high incidence of failure and the need for prolonged postoperative immobilization.
Prosthetic Interposition Arthroplasty
In 1999, Gabos et al. (11) reported the use of a prosthetic interposition arthroplasty in 11 nonambulatory patients with severe mental retardation and CP. Due to the patients’ small proximal femoral diameter and abnormal acetabular contour, two custom proximal femoral replacements and 12 humeral replacements (with or without glenoid replacement) were implanted. The level of resection was either basicervical (n = 3), intertrochanteric (n = 4), or subtrochanteric (n = 7) dictated by the amount of remaining soft tissue tension. Patients were immobilized postoperatively in either abduction pillows (n = 9) or by bilateral leg casts fixed with broomsticks (n = 5) (modified Petrie) for 4 to 6 weeks. Postoperatively four hips dislocated. There was one clinical failure. This patient had constant pain in a dislocated hip. The remaining 10 patients had improvement in sitting ability or tolerance at an average of 4 years and 9 months.
Total Hip Arthroplasty
Since the advent of THA, many patients and caretakers choose this option over arthrodesis or proximal femoral resection for the treatment of the painful hip in CP. The concerns with THA include its long-term durability (as many of these patients are young at the time of implantation), the abnormal muscle strength, the spasticity and contractures that are often present, and poor patient compliance with postoperative regimens. On the other hand, loads across the hip joint may be decreased in this group of patients because they have a low level of activity and often use crutches for ambulation (12).
The indications for performing a total hip replacement in the spastic patient are the following:
Hip pain refractory to medication.
Decreased function in standing, limited sitting, and difficulty with perineal hygiene.
The potential for standing or walking, transfer ability, or upright sitting in a wheelchair.
An absolute contraindication is the presence of ongoing hip infection. Mental retardation is a relative contraindication, as patients who are severely retarded and essentially bedridden are poor candidates.
To the authors’ knowledge, the first report on THA in patients with CP was by Koffman et al. (8). Five THAs were performed on four CP patients with total-body involvement between 1974 and 1977. Only one of four patients was ambulatory. The average age of the patients was 33 years (range 21 to 57). All patients had pain with walking (the ambulatory patient) or with sitting. Three different designs were used: the Sivash, the LaGrange-Letournel, and the Trapezoidal-28. The average follow-up was 4 years. One patient had a dislocation with subsequent loosening of the acetabular component and another patient underwent a resection arthroplasty for a painful implant. Arthroplasty was deemed successful in only one patient. The authors reported that the most common complication at that time was HO. They noted that surgery was technically challenging and they recommended that the acetabular component be placed in more anteversion and the femoral component be placed in slight retroversion in nonambulatory patients. Subsequent to this report, Root (13) and Skoff and Keggi (14) also reported on THA in selected patients with CP. Their results were more promising than Kauffman’s original series.
In 1986, Root et al. (10) reported on the HSS experience. In this series there were 15 total hips done in 15 patients with a follow-up of 2.5 to 12 years. Contractures were released in 11 of 15 hips. All acetabular and femoral components in this series were fixed with cement. Two hips underwent bone graft augmentation for a deficient acetabulum. A postoperative hip spica cast was used in 13 of 15 patients to prevent dislocations and promote healing of the greater trochanter. Pain relief was complete in 14 of 15 patients. Range of motion (ROM) was improved in all patients. There were two frank dislocations and one hip had persistent subluxation with flexion past 90 degrees. Three patients underwent a second operation: One acetabular component was revised for recurrent dislocation, one femoral component was revised for loosening, and one hip was reoperated on for removal of painful trochanteric wires. In 1993, Buly et al. (15) expanded this group to include 18 patients in whom 18 total hips were performed. At an average of 10 years, prosthetic survivorship was 95%.
In 2000, Weber and Cabanela (16) reported the Mayo Clinic experience of THA in patients with CP. The minimum follow-up was 2 years. There were ten males and six females and the average age at the time of surgery was 48.5 years (range 22 to 79). The type of CP was hemiplegia in seven patients, diplegia in four, quadriplegia in two, athetoid quadriplegia in two, and athetoid diplegia in one. The diagnosis leading to THA was primary degenerative hip disease in three patients, arthritis secondary to hip dysplasia in eight, and failed treatment of a fracture of the femoral neck in five.
The preoperative pain was severe in five patients, moderate in nine, slight in one, and unknown in one. Preoperatively, three patients were unable to walk, five walked indoors only, six were community ambulatories, and one patient could walk an unlimited distance; the walking status of the last patient was unknown. The operation was performed through an anterolateral approach in eight patients, a transtrochanteric approach in seven, and a posterolateral approach in one.
Cemented fixation of both components was performed in 12 patients, cementless fixation in two, and a hybrid technique (cup cementless, femur cemented) in two (Fig. 74.3). Soft tissue releases were performed in two patients. One patient was immobilized postoperatively in a spica cast and another in a hip guide brace in an effort to decrease the risk of postoperative dislocation.
At an average of 10 years (2.5 to 21 years), 15 patients were alive. Eleven patients had complete resolution of their pain, two had partial resolution, and one complained of moderate diffuse lower extremity pain. The patient with diffuse lower extremity pain went on to revision at 13 years postoperatively for loosening of both components. Nine of 15 patients had improvement in their walking status, five had no change, and one walking status was unknown.
Intraoperative complications included a trochanteric fracture in one patient and an acetabular fracture on press-fit impaction of an uncemented component in another. Postoperatively, complications included one trochanteric avulsion (after a transtrochanteric approach), one heel ulceration (in a patient that was casted), one ileus, and one case of urinary retention. Four patients have been reoperated on: one for fixation of a trochanteric avulsion, one adductor tenotomy for spasticity, one for removal of painful HO, and one revision of both components for loosening as stated above.
 Figure 74.3. The same patient as in Figure 74.1 8 years after hybrid total hip arthroplasty. The patient is doing exceptionally well and has absolutely no symptoms in the hip. Note slight wear on the polyethylene acetabular liner. |
Radiographs were assessed in 11 patients at the time of last follow-up. Ten stems were solidly fixed and one had some lucency, but was not symptomatic. Nine acetabular components appeared well-fixed, one had lucencies in zones I, II, and III, and another cup was clearly moving, but only caused slight pain in a patient who was still able to walk independently. The authors concluded that THA remains a reasonable option with satisfactory results in patients with CP.
In 2008, Schroeder et al. (17) reported on 18 THAs done in 16 ambulatory patients with CP. The mean age at the time of surgery was 42 and the average follow-up was 10 years. All patients reported a significant amount of pain relief after their THA. At the time of last follow-up, no stem had been revised and four of 18 cups had been revised: three for aseptic loosening and one for recurrent dislocation. In addition, one patient dislocated at 3 months postoperatively, but was treated with closed reduction without further dislocation. The
authors concluded that despite an increased complication rate compared with the standard patient population, THA provides ambulatory patients with CP long-term pain relief and improved function.
authors concluded that despite an increased complication rate compared with the standard patient population, THA provides ambulatory patients with CP long-term pain relief and improved function.
In 2009, Raphael et al. (18) reported on 56 patients (59 hips) with CP treated with THA for a painful hip. The average age at the time of surgery was 30.6 years and average follow-up was 9.7 years. They reported pain relief in all patients and 52/59 hips returned to their prepain functional status. At the time of last follow-up, 9/59 (15%) hips had undergone revision either for component loosening or persistent dislocation. The authors concluded that THA can provide durable pain relief and improved function in patients with CP and severe coxarthrosis.
From the literature one can conclude that THA remains a valuable option for the patient with CP who has incapacitating pain. Pain relief and function can be improved in the majority of patients. Longevity of the implant can also be expected (>95% at 10 years). Technical considerations include paying attention to adductor spasticity that may require adductor tenotomy at the time of implantation. Placing more anteversion on the socket and placing it a little more horizontal, especially in nonambulatory patients, may offer protection from dislocation. If instability is a concern intraoperatively, postoperative support with a hip guide orthosis or even a hip spica cast should be considered.
Finally, in the patient with a preoperative hip subluxation or dislocation the authors prefer to use the posterolateral approach in an effort to protect the abductors which are frequently deficient in this patient population. With the advent of larger femoral heads and a good capsular repair, the authors believe the difference in dislocation risk compared to an anterolateral approach is negligible. The acetabular component should be brought down to the true acetabulum rather than placing it in a high hip center, and should be positioned into slightly less abduction and more anteversion; in addition, at the end of the procedure, the posterior structures (i.e., capsule and external rotators) should be meticulously repaired. In select cases where the surgeon is particularly concerned about dislocation, hip resurfacing or dual-articulation acetabular cup systems may be employed for further stability.
Parkinson Disease
The prevalence of Parkinson disease in the general population older than 60 years is 1% (19). The incidence rate is 20.5 per 100,000 and concomitant dementia is three times more frequent in this population than in a control group (20). Current medical management effectively controls tremors, rigidity, and akinesia; nevertheless, impairment of balancing reflexes in the more advanced stages of disease is aggravated by the postural hypotension that is a side effect of levodopa.
Degenerative arthritis of hips in patients with Parkinson disease may occur through natural processes or after hip fractures. There is extensive literature on the treatment of hip fractures in patients with Parkinson disease (Table 74.2) (6,21,22,23). Eventov et al. (21) in 1983 reported on 62 Parkinson disease patients with hip fractures, of which 39 were subcapital and 23 were intertrochanteric. Thirty-four patients with subcapital fractures had primary hemiarthroplasty, 11 patients with intracapsular fractures had nail–plate insertion, and 12 refused surgery. Five patients were too medically unstable for surgery. Regardless of fracture type, these patients had high mortality and morbidity rates, with pneumonia being the most frequent complication. Patients treated with surgery had better functional results and a better quality of life than patients treated conservatively. In 1988, Staeheli et al. (23) reported high rates of complications at 6 months (mostly urinary tract infections and pneumonias) and a high mortality rate (20%) after 50 hemiarthroplasties in 49 patients with Parkinson for the treatment of femoral neck fractures (Garden III and IV). Despite this, functional results were good. Eighty percent of the survivors could walk. The authors attribute the good results to the rapid mobilization of the patients postoperatively and to the release of contracted adductor muscles at the time of surgery.
Londos et al. (22) in 1989 recommended internal fixation over primary hip arthroplasty for patients with Parkinson
disease and femoral neck fractures. They treated 32 patients with internal fixation. Twenty-four displaced fractures were complicated by six nonunions and three segmental femoral head collapses. In the eight nondisplaced fractures, one case of segmental collapse was diagnosed. Healing complications occurred in 33% of their patients. Three patients with complications required total hip replacement. They compared healing complications to a nonambulatory population of 547 patients with femoral neck fractures. In 151 uncomplicated fractures, healing complications occurred in 8%. In 196 patients with displaced fractures, healing complications occurred in 40% of survivors. Although these authors recommended internal fixation over primary arthroplasty in Parkinson disease patients with femoral neck fractures based on the similar outcomes of internal fixation in a general population of displaced fractures, it would seem logical that perhaps primary arthroplasty should be performed in both population groups for displaced fractures.
disease and femoral neck fractures. They treated 32 patients with internal fixation. Twenty-four displaced fractures were complicated by six nonunions and three segmental femoral head collapses. In the eight nondisplaced fractures, one case of segmental collapse was diagnosed. Healing complications occurred in 33% of their patients. Three patients with complications required total hip replacement. They compared healing complications to a nonambulatory population of 547 patients with femoral neck fractures. In 151 uncomplicated fractures, healing complications occurred in 8%. In 196 patients with displaced fractures, healing complications occurred in 40% of survivors. Although these authors recommended internal fixation over primary arthroplasty in Parkinson disease patients with femoral neck fractures based on the similar outcomes of internal fixation in a general population of displaced fractures, it would seem logical that perhaps primary arthroplasty should be performed in both population groups for displaced fractures.
Table 74.2 Hip Fractures in Parkinson Disease | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|