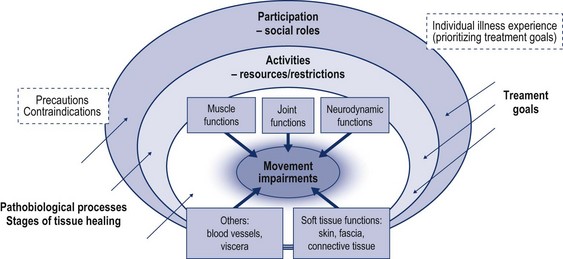
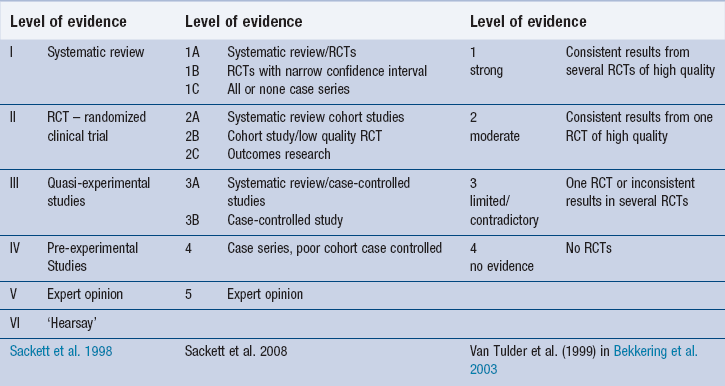
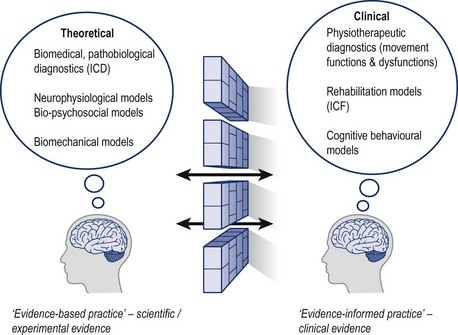
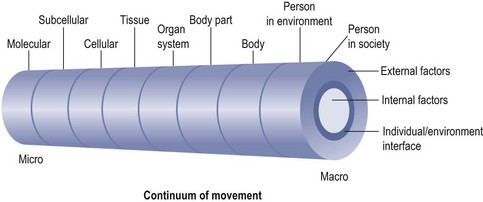
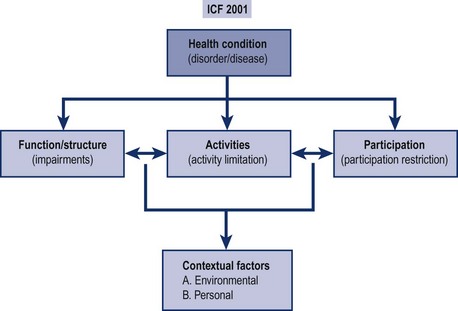
2 In the past few decades the science of physiotherapy has established itself in the field of the movement sciences. It has become accepted that physiotherapists follow a specific movement-rehabilitation paradigm within a bio-psychosocial framework ( CSP 1990, CPA 1992, KNGF 1998, APTA 2001). The roots for this perspective are inherent to the profession, however, it was Hislop’s groundbreaking lecture, which laid the foundation for movement as the core of the declarative knowledge of the profession ( Hislop 1975). She proposed a cybernetic model with a hierarchy of functions for the research, analysis and treatment of human motion. Cott et al. (1995) have elaborated on Hislop’s model with the movement continuum theory of physiotherapy ( Fig. 2.1). Interrelated levels of molecules, cells, tissues, organ systems, body parts and physical and social environment all have an influence on a person’s movement functions. It is recognized that external, social and cultural factors, as well as internal, physiological and psychological factors influence the movement functions at each level of the movement continuum. Each level has a current movement capacity and a movement potential, which ideally should be the same. In this movement continuum all the different concepts and methods of physiotherapy should find their place. Figure 2.1 Movement continuum theory: suggested model of body of knowledge of physiotherapy. The levels are interdependent: functions of one level influence movement capacity of other levels. This model should incorporate all concepts of physiotherapy practice. Reproduced with permission from Cott et al. 1995. In the developmental process of this specific physiotherapeutic movement paradigm, numerous authors around the globe postulated the necessity of this viewpoint as well as the need for clinicians to make a movement diagnosis as a basis for treatment (Rose 1988, 1989; Sahrmann 1988, 1993, Guccione 1991, Grant 1995, Delitto & Snyder-Mackler 1995, Hüter-Becker 1997, de Vries & Wimmers 1997). Also Maitland, in his early development of the concept, postulated that his work was related to the treatment of ‘movement directions’, which need to be analyzed on their quality, range of motion, motor reactions and pain. The core of the concept was dedicated to the rehabilitation of movement functions, overall well-being and meaningful actions ( Maitland 1986). While the movement continuum theory ( Cott et al. 1995) eventually may become the theoretical model which underpins clinical practice and guides research efforts, in daily practice it may not be suitable for making a physiotherapy diagnosis, as the micro levels describe aspects of movement, which cannot be directly observed with the regular clinical examination tools of the physiotherapist. Therefore, diagnosis in physiotherapy may be expressed in terms of movement dysfunctions using the levels of disability as described in the International Classification of Functioning, Disability and Health (ICF) ( WHO 2001): • Functions are the physiological or psychological functions of body systems. • Body structures are anatomical parts of the body such as organs, limbs and their components. • Impairments are problems in function or structure such as significant deviation or loss. • Activity is the execution of a task or action by an individual. • Participation is involvement in a life situation. • Activity limitations are difficulties an individual may have in executing activities. • Participation restrictions are problems an individual may experience in involvement in life situations. • Environmental and personal factors make up the physical, social and attitudinal environment in which people live and conduct their lives. One suggestion is to incorporate the ICF in the basic taxonomy of physiotherapy and manual therapy practice (Hengeveld 1998, 1999) to allow follow-up of treatment goals beyond impairment levels, as debated by Dekker et al. (1993) and Van Baar et al. (1998ab). The analysis of impairments of movement functions has been the specific domain of manual therapists for a long time. Figure 2.2 delineates a model in which manual therapists can integrate their specific taxonomy of analysis of the components of movement impairment into a model of the ICF. This model may further serve in the definition of comprehensive treatment goals at all levels of disablement, in which the individual illness experience ( Kleinmann 1988) may determine the priorities of goal setting at each level of disablement. In rehabilitation, the specific strengths of the different professions may be better utilized: for example, generalist physiotherapists and occupational therapists have developed many skills in rehabilitation at the levels of activities and participation, whereas manual therapists are able to give their special contribution to a team through the analysis and treatment of movement impairments and pain. The physiotherapy profession has come a long way since Hislop’s historical, groundbreaking lecture in 1975. Many countries have established scientific communities and a regular exchange of information at conferences, in peer-reviewed journals and by electronic means is taking place. As is the case with many other professions in the medical field, physiotherapy has moved into the era of evidence-based practice. Practice guidelines are being developed and recommendations for care are given based on reviews and meta-analyses of clinical trials. Evidence-based practice has been defined as follows ( Sackett et al. 1998): It is emphasized that evidence-based medicine is not ‘cook book’ medicine and the clinician needs a mastery of patient interviewing and physical examination skills ( Sackett et al. 1998, p 2, 3, IX). Sackett et al. (1998) and Straus et al. (2005) described different levels of evidence, which are, however, in contrast to levels of evidence as described by van Tulder et al. (1999, in Bekkering et al. 2003) ( Table 2.1). It appears that both listings have been developed from different viewpoints. While van Tulder et al.’s list might help scientists with meta-analyses and forms the basis for the development of practice guidelines, Sackett et al.’s list has probably been developed from a clinician’s point of view. In particular, van Tulder et al.’s levels of evidence list might cause clinicians problems in various daily clinical situations because physiotherapists often need to make decisions on treatment for problems for which no randomized control trials (RCTs) have been published. For example, the treatment of common problems such as osteoarthritis of the carpometacarpal joint with passive mobilizations and muscular control does not appear to have caught the interest of clinical researchers yet. A CINAHL and Medline Database search up to December 2011 reveals that there are no studies investigating this topic, although numerous studies have dealt with the physiotherapeutic treatment of osteoarthritis of other joints, such as the knee complex or hip (e.g. Hoekstra 2004, Ottawa Panel 2005, Dieppe & Lohmander 2005, Moss et al. 2007, Altmann et al. 2010). Similar examples can be given for the treatment of neurodynamics and movement disorders. A body of knowledge, underpinned by systematic inquiry, is growing, however, to date, only few systematic reviews have been published ( Ellis & Hing 2008). Therefore, a list of levels of evidence, which integrates only RCTs may leave physiotherapist-clinicians with a sense of discomfort, particularly because they have been integrated into practice guidelines ( Bekkering et al. 2003) and therefore may have implications on policies being derived from them. • In the rehabilitation of painful movement disorders, the way that treatment is applied, the communication between the physiotherapist and the patient and aspects such as motivation, beliefs, learning experiences, collaboration, education, setting, individual concerns and so on may influence the results of the treatments applied ( Linton 1998). In decision-making processes with regard to treatment subtle non-biomedical cues as intonation of voice, body language, facial expression and selection of words may have a decisive influence on the way treatment is being applied ( Stein 1991). This raised the question: if the effects of a sound therapeutic relationship as a basis for clinical practice have already been researched in such detail that RCTs and meta-analyses would be available to underpin current clinical practice? ( Linton 1998). • Regardless of available studies, it is more likely that evidence-based practice guidelines may at times give an indication as to which decisions not to take, such as, for example, avoiding bed rest and overreliance on X-rays, but they may give little indication as to which topics specifically should be addressed, which may be of concern to the individual patient and which may influence the final outcome of the patient’s problem ( Van Tulder et al. 2006, Vleeming et al. 2008). In an analysis of evidence-based practice and client-centred care, Bensing (2000) raises the question as to how much client-centeredness is represented within evidence-based practice and how far evidence-based client-centred practice has been established to date. She argues that evidence-based practice, in spite of its definition, has become more disease-oriented rather than client-oriented. In a client-centred approach clinicians should base their decisions on the best available evidence and an individual’s needs and preferences. She postulates that with the development of guidelines, protocols and standards derived from evidence-based medicine, ‘the discussion about norms and values seems to shift from the clinician’s consultation room to the conference room of the professional association’ ( p. 19), in which there may be no space left for individual decision-making processes by the clinician collaboratively with the client. In this way, individualization of treatment may become restricted and the responsibility for clinical decisions shifts from a personal clinician-patient decision to a professional group decision ( Bensing, 2000). In a study with audiotaped interviews and questionnaires with one-month follow up Turner et al. (1998) concluded that providers typically addressed medical issues, but did not assess or inconsistently assessed functional limitations related to pain and did not discuss how to resume normal activities, although this was a highly rated goal for most patients. Physicians often did not adequately reassure patients that serious conditions were ruled out, nor did they consistently address explicit worries by the patient. Foster et al. (2008) support the need to assess patients’ cognitions about their back problem, as they concluded from their study, using various questionnaires that patients expecting their back problem to last a long time, perceiving serious consequences or holding weak beliefs in the controllability of their pain, were more likely to have poor outcomes six months after initial consultation. On the other hand, Moore et al. (2000) point out that illness perceptions, such as pain-related worries and fear–avoidance beliefs, may be more effectively treated when self-care about pain and functional limitations are addressed at an initial consultation and written information material, such as books or videos, is provided. • The inclusion and exclusion criteria for many studies form another aspect of the dilemma. Physiotherapists may not always recognize their own patients as they are presented in clinical studies: inclusion criteria may be based on pathobiological diagnoses rather than on movement disorders ( Maluf et al. 2000) or outcome measures used in the studies may not reflect the relevant clinical outcome measures of pain and movement function of the physiotherapist ( Jones & Higgs 2000). Nevertheless in recent years several classifications appear to give a more suitable reflection of the clinical reality of physiotherapists, such as, for example: McKenzie’s (1981) classification of pain distribution and a patient’s reactions to repeated movements; Sahrmann’s and O’Sullivan’s classification of movement and motor control ( O’Sullivan 2005), and also the adaptation of O’Sullivan’s work on movement disorders of the foot and ankle ( Kangas et al. 2011). However, it appears that no internationally established, validated classification system is available yet for physiotherapy-specific research ( Billis et al. 2007). • Another dimension of the dilemma may lie in the fact, that many of the problems encountered in daily physiotherapy practice are multicomponential and multidimensional movement disorders, whereas many studies deal with problems which are unistructural in nature, in which it is assumed that the problems have a single cause and need a single treatment approach. • Studies with regard to outcome measurements may not be of the same relevance as outcome measurements in daily clinical practice ( Jones & Higgs, 2000). Furthermore, it appears that in every newly built scientific community similar discussions seem to take place, on for example, the questions of validity, reliability, sensitivity and specificity of clinical assessment procedures. Some scientists seem inclined to recommend discarding tests with low reliability coefficients, for example, palpation procedures and intervertebral mobility tests, without offering useful alternatives to assess the parameter concerned ( Comeaux et al. 2001, Bullock-Saxton et al. 2002). However, a more differentiated analysis of reliability studies and their results show that values may increase if the data are being clustered ( DePoy & Gitlin 1998), or when reference standards different from inter-therapist comparisons are being employed ( Jull & Bogduk 1988, Phillipps and Twomey, 1996). Although it may be useful to discard examination and treatment methods, which are proven to be ineffective, no relevant procedures should be rejected without offering meaningful alternatives. • Whether there is an increasing gap between research-based knowledge and its application in clinical practice is debatable. Some authors claim that clinical practice by definition lags behind science ( Van den Ende 2004). However, Schön (1983) argues that the experiential knowledge base of clinicians needs to be respected, as clinicians often need to interpret incomplete and ambiguous information in order to make decisions with regard to practice. In particular, experiential knowledge with insights or unusual observations from numerous clinical situations may lead to meaningful research questions, which over time could be generalized in overall practice (e.g. the application of neurodynamics examination and treatment or passive mobilization treatment under compression of joint surfaces). In such cases clinical practice may be ahead of science. In fact, it is noted by Parry that many physiotherapists who contributed to current clinical practice employed forms of qualitative research without explicitly referring to it: As a consequence of these dilemmas physiotherapists are frequently left to their own devices when making the best decisions with and for their patients in daily practice. They often need a balanced and pragmatic approach towards clinical practice and results from evidence-based practice. Not only will physiotherapists need a mastery of patient interviewing and physical examination skills ( Sackett et al. 1998), but they will also need a proficiency in the application of various treatments, including communication abilities and clinical reasoning skills. Clinical reasoning may be summarized as ‘wise action’ ( Jones 1995), in which physiotherapists endeavour to integrate three areas into their decision-making processes: 2. The best of current therapies with sound assessment procedures and varied treatment strategies 3. The best of the patient–therapist relationship, with a client-centred approach with empathy, unconditional regard and genuineness ( Rogers 1980), communication, educational strategies and an awareness of the possibilities of a cognitive–behavioural approach to the overall therapeutic process. Nevertheless, evidence-based practice is an essential skill for enhancing clinical practice; however, it can only be applied successfully with an increased awareness of clinical reasoning processes ( Jones & Higgs 2000) and consequent assessment procedures. Here evidence-based practice correlates with one of the main pillars of this concept of physiotherapy: the primacy of clinical evidence ( Wells 1996). Maitland’s ‘brick wall’ model of clinical reasoning serves as a framework for decision-making processes (see Chapter 1). It serves therapists to take different viewpoints in the analysis of a person’s (movement) disorder and pain. The brick wall model of clinical reasoning delineates that a conscious distinction needs to be made in the application of biomedical, pathobiological knowledge and physiotherapy-specific insights. It serves physiotherapists to dissociate from biomedical diagnoses, without discarding them, and to formulate a physiotherapeutic, movement-oriented diagnosis as a basis for decision-making processes with regard to specific physiotherapeutic treatment. The brick wall model of clinical reasoning laid the foundation for physiotherapists to become aware that they should apply different paradigms in the problem-solving processes with a patient. In addition to biomedical and physiotherapeutic paradigms, other models and perspectives may be integrated in the brick wall model of clinical reasoning. It is postulated that physiotherapists or manual therapists use various paradigms (models) in their clinical reasoning processes, which, dependent upon the clinical relevance of a given situation, may be employed more or less dominantly ( Banks & Hengeveld 2010). Several of these models appear to be more or less profoundly scientifically examined and hence contribute more or less to the accepted body of knowledge of the scientific communities concerned. However, it seems possible that some studies resulting from less dominant paradigms in a scientific community may find less acceptance and may not be regarded as relevant knowledge contributing to the levels of evidence. Figure 2.3 illustrates different paradigms in clinical reasoning processes. As stated before in this chapter the basis of physiotherapy diagnosis stems from the subjective and physical examination and exploratory treatments ( Banks & Hengeveld 2010). Passive mobilizations play a central role in physiotherapy diagnosis in many movement disorders – not only for screening with the aim of reproducing the patient’s symptoms emanating from different joints, neural structures or soft tissue areas, but also during exploratory treatment and reassessment. The latter demonstrates an important principle of this concept of manipulative physiotherapy: differentiation not only by assessment procedures, but also by treatment. The terms of the International Classification of Functioning, Disability and Health (ICF – WHO 2001) may serve as a basis in the description of the physiotherapeutic diagnosis (see Fig. 2.4). A comprehensive description of a patient’s condition needs to integrate observations regarding functional and possible structural impairments, activity and participation resources and/or limitations, the influence of biomedical conditions on the levels of functioning and possible social – psychological contributing factors to the levels of functioning ( Fig. 2.4). Figure 2.4 Physiotherapeutic diagnosis needs to encompass all dimensions of the ICF (after WHO 2001). Reproduced with permission from Banks & Hengeveld 2010.
The Maitland Concept
Evidence-based practice and the movement sciences
Introduction
Physiotherapy diagnosis and ICF
International Classification of Functioning, Disability and Health (ICF)
Evidence-based practice
Dilemmas and challenges of evidence-based practice
Evidence-based practice and clinical reasoning
Movement sciences and paradigms to movement
Paradigms to movement
Physiotherapy diagnosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Maitland Concept: Evidence-based practice and the movement sciences