The Korean Experience in Total Hip Arthroplasty
Shin-Yoon Kim
Osteonecrosis of the femoral head (ONFH) is the death of the cellular portion of the bone, with subsequent structural changes, leading to progressive collapse of the femoral head followed by degenerative arthritis of the hip joint. Diverse conditions have been implicated in the development of secondary osteonecrosis (ON), including corticosteroids, alcohol abuse, trauma (femoral neck fracture), gout, diabetes, and sickle cell anemia. Although the precise pathophysiology of ONFH is not clear, it has been suggested that a common source of ONFH involves an interruption of the blood supply to the femoral head, thus leading to ischemic insult and bone collapse. Ischemia can be produced by vascular interruption (fractures or dislocations), by thrombotic occlusion (intravascular coagulation), or by extravascular compression (marrow fat enlargement). Current evidence suggests that intravascular coagulation and microcirculatory thrombotic occlusion likely provide a final common pathway for nontraumatic ON. In this chapter, we are going to introduce new attempts at treatments and procedures and review the recent studies of ONFH performed at Kyungpook National University hospital and Korean Hip Society, compared with studies in other countries.
Epidemiology
ONFH frequently affects young and active patients between 20 and 50 years of age. Larvenia et al. (1) reported new cases of ONFH in the United States of America number between 10,000 and 20,000 per year. In Japan, Fukushima et al. (2) reported the number of idiopathic ONFH was estimated to be 11,400 during 2004. The peak in age distribution in patients in this group occurred in their 40s. In younger patients under 40 years of age, the most frequent causative factor was systemic steroid administration (51%). Systemic lupus erythematosus was reported as the most frequent (31%) underlying disease. In response to this condition, hip replacement was the most frequently performed procedure (65%). In Korea, the average estimated number of annual cases was 14,103, indicating a 28.91 per 100,000 average occurrence over a 5-year (from 2002 to 2006) period (3). Males predominated the patient population. Alcohol abuse (32.4%) was the most frequent causative factor, and bilateral involvement was noticed in 37% of patients. Hip arthroplasty was the most frequently performed initial treatment (63.9%).
Natural History
Symptomatic ONFH may require many kinds of medical or surgical interventions to relieve pain and to prevent collapse or progression of the disease. ONFH usually presents bilaterally without symptom and the treatment of the asymptomatic hip can be controversial. Therefore, it is critical to evaluate the overall inevitability of progression to symptomatic disease and/or femoral head collapse as well as to determine which radiographic and demographic factors influence preservation or progression of ONFH, to select the appropriate medical and/or surgical interventions.
Min et al. (4) monitored 81 patients (81 asymptomatic hips) whose other hips had nontraumatic symptomatic ONFH with minimum 5-year follow-up prospectively, and they concluded that only the extent of large necrotic lesions and location of type C2 necrotic lesions predicted collapse. Nam et al. (5) reported 1 of 21 hips with small (<30% of area of the femoral head) necrotic lesions, 11 of 24 hips with medium (30% to 50%) necrotic lesions, and 50 of 60 hips with large (>50%) necrotic lesions which became painful with a minimum 5-year follow-up. Johannson et al. (6) performed a comprehensive literature search including 16 studies of 664 hips of untreated asymptomatic ONFH to evaluate the differences in outcomes based on lesion size, lesion location, and radiographic stage at the time of diagnosis.
Small, medially located lesions had a probability of collapse of <10%. Patients with sickle cell disease had the highest frequency of progression and patients with a history of systemic lupus erythematosus had the most benign course. They recommended considering joint-preserving surgical treatment in asymptomatic patients with a medium size or large, and/or laterally located, lesion because of a high incidence and probability of progression to symptomatic hip and femoral head collapse.
Head-Preserving Procedures
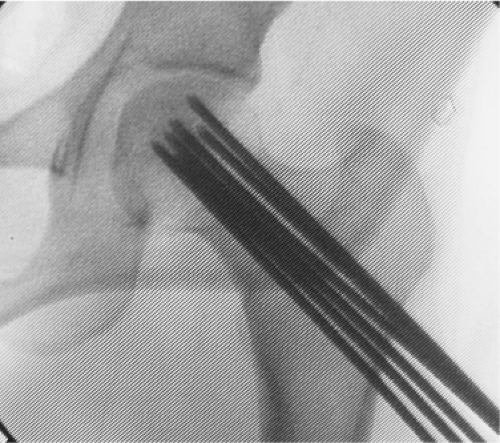
Multiple Drilling
Instead of traditional core decompression using an 8- to 10-mm wide cannula, Korean surgeons tried a new technique using multiple small drillings with a 9/64 Steinmann pin or 3-mm drill bit (Fig. 65.1). We previously reported that multiple drilling had excellent results in a precollapsed head with small or medium size at medial or central located lesion (7). Subsequently, Mont et al. (8) reported an 80% success rate in tage I hips and a 57% success rate in stage II hips with a mean follow-up of 2 years, with no surgical complications. Song et al. (9) reported comparable results of multiple drilling with those of core decompression as reported in the literature—a 79% success rate in stage I hips and 77% success rate in stage II hips with a minimum follow-up of 5 years in 163 hips (136 patients). All (15/15) small lesions (<25% involvement) and 84% (37/44) of medium-sized lesions (25% to 50%) were successfully treated. We previously reported that percutaneous multiple drilling was more effective than core decompression for the prevention of collapse and dome depression in precollapsed lesion of ONFH (10). However, there is no prospective and randomized comparative study between core decompression and multiple drilling yet. This technique is technically straightforward with few complications or morbidity.
Vascularized Fibular Grafting
We previously reported vascularized fibular grafting (VFG) had better clinical results and was a more effective way to prevent the collapse and depression of the femoral head with a large lesion than nonvascularized fibular grafting in a prospective case control study with a minimum 3-year follow-up (11). Yoo et al. (12) reported long-term results with a minimum 10-year follow-up of VFG in 110 patients (124 hips). They found improved or unchanged radiographs in 37 of 59 stage II hips and 39 of 65 stage III hips. Thirteen hips (10.5%) (13 patients) failed treatment and underwent total hip arthroplasty (THA). The location and size of the necrotic lesion and the patient’s age influenced long-term survival of the graft. In the United States, Edward et al. (13) retrospectively reviewed 61 patients (65 hips) who underwent FVFG for precollapse ONFH. Forty-nine of 65 hips (75%) had surviving FVFG for at least 10 years. In the last follow-up, 39 of 65 hips (60%) had surviving FVFG, with a mean graft survival time of 15 years (range, 10.5 to 26.1 years). Twenty-six of the 65 hips with FVFG (40%) underwent conversion to THA at a mean of 8 years postoperatively. Demographic factors, lesion size, additional procedures, and low preoperative function were not associated with changes in graft survivorship. Pain and function were similar in patients with surviving FVFG and patients who had conversion to THA. Patients with surviving FVFG were more likely to engage in impact sports or active events than patients who had conversion to THA. They continue to use FVFG for treating patients younger than 50 years with symptomatic, precollapse ONFH.
Transtrochanteric Rotational Osteotomy
Transtrochanteric rotational osteotomy, originally developed by Sugioka in Japan (14), displaces the necrotic portion of the femoral head from a weight-bearing zone and replaces it with healthy cartilage and living bone. In Korea, Ha et al. (15) reported the results of 105 patients (113 hips) who underwent an anterior transtrochanteric rotational osteotomy for the treatment of ONFH with a mean of 51.3 months follow-up. Secondary collapse occurred in 27 hips (24%), and 14 hips (12%) were converted to a THA. The age of the patient (>40 years), body mass index (≥24 kg/m2), and extent of the necrosis (a combined necrotic angle of ≥230 degrees) were associated with secondary collapse. Yoon et al. (16) introduced the modified transtrochanteric rotational osteotomy for the treatment of large-sized ONFH. After transtrochanteric rotational osteotomy, he created a window in the neck–head junction and inserted a muscle–pedicle–bone graft from anterior greater trochanter where the distal gluteus medius muscle is attached.
Cell Transplantation
Recently, several studies have shown that the transplantation of mesenchymal stem cells (MSCs) could improve Harris hip scores and radiographic findings in patients with ONFH. The clinical results of those studies had a close relationship with the numbers and concentration of the MSCs transplanted in studies undertaken in Europe (17,18).
Kim and Kwon modified and tried multiple drilling and transplanted bone marrow stem cells into the necrotic lesions of femoral head in 159 hips (113 patients) (unpublished data). To prevent the leakage of bone marrow, fibrin glue was injected. Fifty-two hips (32.7%) were considered to have achieved radiologic and clinical success without additional surgery after a minimum 5-year follow-up. Thirty-six
of 56 (64.3%) hips with Ficat stage IIa disease and 26 of 46 (56.5%) hips with stage IIb disease were considered clinically successful after a minimum 5-year follow-up. However, after femoral head collapse had occurred (stage III), the success rate (24/57, 42.1%) was poor. Multiple drilling and stem cell transplantation did not change the fate of ONFH. Significant differences in outcome were observed in patients who had the greater number of transplanted cells, as opposed to patients with a decreased number of progenitor cells in the iliac crest and a decreased number of transplanted cells.
of 56 (64.3%) hips with Ficat stage IIa disease and 26 of 46 (56.5%) hips with stage IIb disease were considered clinically successful after a minimum 5-year follow-up. However, after femoral head collapse had occurred (stage III), the success rate (24/57, 42.1%) was poor. Multiple drilling and stem cell transplantation did not change the fate of ONFH. Significant differences in outcome were observed in patients who had the greater number of transplanted cells, as opposed to patients with a decreased number of progenitor cells in the iliac crest and a decreased number of transplanted cells.
Total Hip Arthroplasty
More than half of the patients who underwent THA in Korea have ONFH, a condition especially common in young, active patients. Wear-induced osteolysis and subsequent aseptic loosening is the most important factor limiting long-term results in THA. Age and activity of patients are critical factors influencing wear and loosening. Traditionally, patients with ONFH have a higher rate of failure of total hip prostheses than patients with other diagnoses, especially when the acetabulum is cemented. However, a recent systemic literature review provides evidence that ON itself, or when associated with the most common risk factors and/or diagnoses, is not associated with poor outcomes of THA (6). The necrosis can be extended to the proximal femur and acetabulum and compromise the fixation of the prostheses, however; Yoo et al. (19) reported osteogenic potentials of BMSCs are not defective in patients with ONFH. There was no difference in long-term clinical and radiographic results of cementless THA and hybrid THA in patients with ONFH (20).
Bearing Surfaces
There are three kinds of alternative bearing surfaces: the new, highly cross-linked polyethylene, metal-on-metal, and ceramic-on-ceramic, the last being specifically used for young active patients to reduce the wear-induced osteolysis.
Ceramic Bearings Including Alumina-on-Alumina and Delta-on-Delta Articulation
Ceramic-on-ceramic is now the most frequently used bearing surface for THA in Korea. We previously reported excellent midterm results of THA using alumina-on-alumina articulation without loosening, osteolysis, and fracture in young (mean age 39 years) and active patients with ONFH (21). However, noise developed in 14 (20%) of the 71 hips in the study. One alumina head fracture and one alumina liner fracture subsequently developed without trauma (unpublished data). Kim et al. (22) also reported excellent long-term results of cementless THA using alumina-on-alumina articulation without loosening, osteolysis, or ceramic fracture with minimum 10-year follow-up in patients younger than 45 years (mean age 38 years) with ONFH. Osteolysis was analyzed using radiographs and computed tomographic (CT) scans also. Two of 93 hips (2%) had click or squeaking sound. In general, Koreans require a greater range of hip joint motion because of frequent squatting and cross-legged sitting posture on the floor in daily life than do patients from western cultures. The prevalence of ceramic fracture is relatively higher in Korea than that of global data. Koo et al. (23) reported 5 hips (1.4%) of alumina head fracture in 359 hips underwent alumina-on-alumina THA.
For the last few years, THA using delta-on-delta articulation has been widely used in Korea substituting THA using alumina-on-alumina articulation.
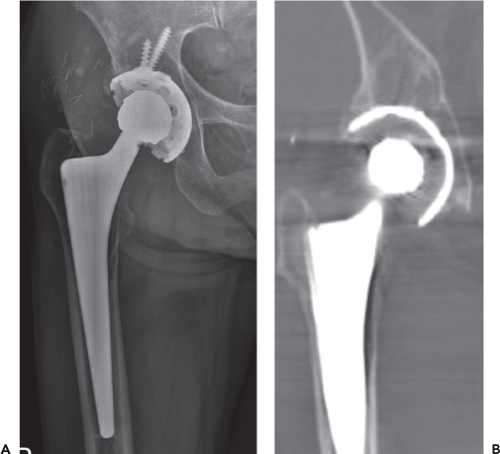
Metal-on-Metal Articulation
We previously reported midterm results of THA using second-generation Metasul metal-on-metal articulation in a major portion (87%) of 59 patients having a diagnosis of ONFH (24). There was no aseptic loosening and only one pelvic osteolysis was found. However, the incidence of osteolysis increased compared with previous intermediate-term results. After a minimum of 11-year long-term follow-up, osteolysis was identified in the acetabulum of 10 hips (14.7%) and in the femur of 4 hips (5%). In three hips, osteolytic lesions were found in both the acetabulum and the femur (Fig. 65.2). Three loose acetabular components with extensive pelvic osteolysis and a subsided femoral stem were revised. One patient underwent staged revision arthroplasty on a hip due to infection. Two patients underwent open reduction and internal fixation due to periprosthetic fracture. Survivorship with revision for any cause was 88.9% (95% confidence interval, 85.7% to 96.3%) (unpublished data).
Hwang et al. (25) also reported excellent long-term results of cementless Metasul metal-on-metal THAs in 70 patients (78 hips) with a minimum follow-up of 11 years. Survivorship with revision for any cause was 98.7% (95% confidence interval, 98% to 100%), and survivorship due to the development of osteolysis for any lesion was 97.5% (95% confidence interval, 95% to 99%). Only two patients (two hips) experienced early, progressive osteolysis. Only a few hip surgeons had performed resurfacing metal-on-metal THA. Recently, resurfacing THA using metal-on-metal articulation was abandoned in Korea.
Highly Cross-linked Polyethylene
We previously reported excellent midterm (minimum 7-year follow-up) results with a decreased wear rate and a low incidence of osteolysis of 113 cementless THAs using metal on first-generation highly cross-linked polyethylene (HXLPE) (Longevity, Zimmer, Warsaw, IN, USA) in a major portion (72%) of 109 patients with a diagnosis of ONFH (26). There was no component loosening. Acetabular osteolysis was found in 12 hips (10.6%). The mean linear HXLPE wear rate was 0.031 ± 0.012 mm/yr. Only the cup position was related significantly with the wear rate of HXLPE. There was no mechanical failure of HXLPE in Koreans, who require extreme range of hip joint motion because of frequent squatting and cross-legged sitting posture on the floor in their daily life. Kim et al. (27) reported excellent midterm (mean 8.5 years) results of 73 cementless THA with alumina on HXLPE bearing in young patients with ONFH. The mean polyethylene liner penetration was 0.05 ± 0.012 mm/yr and no hip had loosening or osteolysis.
Surgical Approaches
The majority of arthroplasty surgeons in Korea use the posterior approach when repairing the short external rotator and capsule. Two modified surgical approaches to THA had been introduced recently. Kim et al. (28) introduced a modified posterior approach to THA to enhance joint stability. He preserved the piriformis, superior gemelli, and obturator internus. The inferior gemelli and obturator externus was sectioned at the bony insertion and the posterior part of the joint capsule was excised to the maximal extent possible. Using this approach, after 1 year he reported no early hip dislocation among 220 THAs. Yoon et al. (29) modified the traditional two-incision posterior approach. He used intramuscular dissection in the lateral decubitus position. The dissection was made between gluteus medius and tensor fascia lata anteriorly, and posteriorly between gluteus medius and piriformis. He suggested this approach could reduce the lateral femoral cutaneous nerve injury associated with dissection between tensor fascia lata and sartorius and could allow early rehabilitation due to less soft tissue damage.
Development of New Prostheses
BENCOX Hip System
Recently the BENCOX hip system (Corentec, Seoul, Korea) was designed by Korean orthopedic surgeons. The acetabular component is a hemisphere, whose external diameter is larger by 1.7 mm than the reamer of the same size, maximizing both peripheral and polar contact. The two screw holes are designed based on the anatomical position of the hip, effectively securing the fixation strength and enhancing the convenience for operation by allowing sufficient angle for insertion (Fig. 65.3A). The femoral component is a typical double-tapered wedge stem, designed to suit the anatomical structure in the marrow cavity (Fig. 65.3B). The BENCOX stem is manufactured from a titanium alloy (Ti6Al4 V ELI), according to ASTM F136/ISO 5832-3, and has a proven grit-blasted surface finish (4 to 6 μm) designed after two decades of clinical history as a guide. To maximize bone ingrowth, the surface of the stem is treated with microarc oxidation (MAO), maintaining average 5.5 μm of surface roughness. The proximal geometry features a collarless dual taper design with a rectangular cross section. The rectangular cross section provides rotational stability whereas the proximal lateral-to-medial taper provides an additional medial locking effect for added primary implant stability. The proximal fins taper both proximal to distal and lateral to medial and are designed to optimize proximal primary fixation in cancellous bone. The tapered distal design acts mainly to centralize the implant within the femoral canal and the anatomical medial–proximal portion aids in stress distribution. The distal taper design also results in a low incidence of thigh pain. The neck is 135 degrees which is similar to the normal anatomical angle. The BENCOX stem has neck geometry optimized for increased range of motion which is also the core design concept. The enhanced neck is a patented trapezoidal design which allows wide angulations and protects impingement and prevents dislocation.
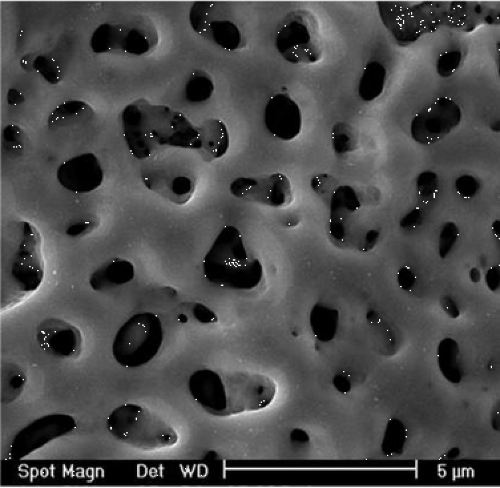
The surface treatment of the femoral components uses MAO (Fig. 65.4). In the dental field, the MAO method has recently been developed to enhance osseointegration. This
provides nanoporous pits, thick oxide layers, and the incorporation of calcium and phosphorus into the coating layer which results in improved osteoblast cell responses, such as an enhanced rate of actin, vinculin cytoskeletal reorganization, and the formation of integrins mediating osteoblast adhesion. The average roughness of a Ti-alloy surface, treated by the MAO process, is about 0.3 to 0.5 μm. Smooth surfaces are sufficient for dental implants for early fixation and long-term mechanical stability possibly owing to the screw fixation and their small size. But cementless femoral stems require rough surfaces for early fixation and long-term mechanical stability because these are more or less cylindrical and large in size. The average roughness of Ti-alloy surfaces treated by the MAO process is too low to apply to the cementless femoral stem. Therefore, the BENCOX stem modified the surface of the Ti alloy by grit-blasting, then employed the MAO method to enhance the surface roughness to take advantage of its superior biocompatibility, which was demonstrated in a pilot study by Lim et al. (30).
provides nanoporous pits, thick oxide layers, and the incorporation of calcium and phosphorus into the coating layer which results in improved osteoblast cell responses, such as an enhanced rate of actin, vinculin cytoskeletal reorganization, and the formation of integrins mediating osteoblast adhesion. The average roughness of a Ti-alloy surface, treated by the MAO process, is about 0.3 to 0.5 μm. Smooth surfaces are sufficient for dental implants for early fixation and long-term mechanical stability possibly owing to the screw fixation and their small size. But cementless femoral stems require rough surfaces for early fixation and long-term mechanical stability because these are more or less cylindrical and large in size. The average roughness of Ti-alloy surfaces treated by the MAO process is too low to apply to the cementless femoral stem. Therefore, the BENCOX stem modified the surface of the Ti alloy by grit-blasting, then employed the MAO method to enhance the surface roughness to take advantage of its superior biocompatibility, which was demonstrated in a pilot study by Lim et al. (30).
Kim et al. had excellent short-term clinical and radiographic results (unpublished data). Fifty-five patients (60 hips) underwent primary cementless THA using the BENCOX hip system. The mean follow-up was 42.2 months (range, 38 to 54 months). The mean Harris hip score improved from 48.4 points (range, 32 to 69 points) preoperatively to 95.6 points (range, 87 to 100 points) at final follow-up. At the time of the final follow-up one patient (one hip) had a mild limp, but no patient required any kind of walking support. No patient reported a squeak or any other noise in the operated hip. During the follow-up period, no revision surgery was required.
Short Metaphyseal-fitting Proxima Stem
Kim YH had been involved in developing a new short metaphyseal-fitting porous-coated cementless femoral component (Proxima; DePuy, Leeds, United Kingdom). The main objectives were to preserve bone and to provide more physiologic loading. The short Proxima femoral component was designed to have a close fit within the proximal femur with the aim of maximizing primary stability, particularly in torsion, thereby limiting bone resorption due to stress shielding. It is manufactured using Ti alloy and is entirely porous coated with sintered titanium beads having a mean pore size of 250 mm, to which a 30-μm thick hydroxyapatite coating is applied, except for the distal tip. The design features are a longer proximomedial portion of the stem, a highly pronounced lateral flare, and preservation of the femoral neck. Kim et al. (31) reported stable fixation in young and elderly patients and minimal stress shielding bone resorption in the calcar region.
Genetic Study
Background
As was stated earlier in this paper, ONFH is believed to have multifactorial causes and is associated in some cases with both a genetic predisposition and exposure to certain risk factors. Most definite or probable risk factors of nontraumatic ONFH includes corticosteroids, alcoholism, lipid disturbances, sickle cell anemia, coagulopathies as well as associated idiopathic conditions, and causes (32,33,34).
The incidence of corticosteroid or alcohol-induced ONFH may also reflect ethnic differences and susceptibilities (35). Some patients who use corticosteroids or have excessive alcohol intake develop ONFH, but others do not, indicating the presence of individual differences in sensitivity to these risk factors. The fact that only ∼5% of patients with a history of high-dose corticosteroid use or alcohol abuse develop ON, (36,37) means there is a likely genetic predisposition to ONFH. Particularly, idiopathic ONFH in twins and a clustering of cases in families (38,39) also imply that genetic factors are involved. Therefore, many groups are studying genetic traits that may predispose individuals to the development of ON. Although most early studies focused on coagulation system and clotting disorders, newer studies have shown that other predisposing factors may be associated with the risk of ONFH. In recent years, we have focused on new candidate genes, participating hypoxia, angiogenesis, adipogenesis, osteogenesis, etc. On the basis of review of the literature (40) and our studies, we briefly summarized the papers regarding genetic association studies of ONFH which were related to three major etiologies: idiopathic, steroid-induced, and alcohol-induced.
Genetic Studies of ONFH
Among the pathogenic mechanisms of ONFH that have been suggested to date, a vascular hypothesis is considered to be the most persuasive. It assumes that if thrombosis occurs, it is followed by a sequential process of blood flow obstruction, increased venous pressure, impaired arterial flow, osseous hypoxia, and bone death (41,42) which appear to be significant in ONFH development.
Factor V Leiden (G1691A, Arg506Gln) generates coagulation factor V, which is less effectively degraded by activated protein C, resulting in a hypercoagulable state. Heterozygosity in the mutation is associated with a seven- to eightfold increase in the lifetime risk of venous thrombosis, whereas homozygosity has an almost 100-fold increased risk (43). Although an increased tendency for intravascular coagulation has been proposed as a pathogenic mechanism of ONFH, the association between genetic predisposition and thrombotic tendency may differ between ethnic groups. Several studies have reported that the factor V Leiden mutation increases the risk of primary ON (41,42,44) yet other studies have failed to observe these associations (45). Moreover, neither factor V Leiden nor the prothrombin G20210A mutation has been found in the Korean population (46,47). Plasminogen-activating inhibitor-1 (PAI-1) was also studied in patients with ON. PAI-1 is a critical factor that regulates coagulation and fibrinolytic systems. Reduced plasma fibrinolytic activity, mainly attributable to increased levels of PAI-1, is associated with ONFH development (45,48




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree