The insensitive foot
Jennifer M. Bottomley
Introduction
Insensitivity of the foot is the usual end result of numerous pathological conditions that affect the elderly. Chronic diseases such as diabetes mellitus, Hansen’s disease, peripheral vascular disease, Raynaud’s disease, deep vein thrombosis, spinal cord injury (e.g. spinal stenosis, tumors), peripheral nerve injuries, hormonal imbalances and vitamin B-complex deficiencies produce breakdown of the microvascular structures with diminution of sympathetic nerve endings and somatic sensory receptors leading to neuropathic conditions of the foot. These pathologies lead to a decrease in circulatory and peripheral nerve integrity, which results in edema, discoloration, diminished skin status, increased pain, absence of sensation and, ultimately, a decrease in functional mobility (Birke, 2002; Jeffcoate & Harding, 2003; Driver et al., 2010).
Typical warning signs such as changes in gait patterns and pain associated with foot pathologies are absent in the insensitive foot. Repetitive stress, coupled with the loss of protective sensation, is the primary cause of foot ulcerations. The lack of a warning system for pain and abnormal stress on the plantar surface of the foot predispose the neuropathic foot to injury and ulceration (Boulton, 2012). However, if the mechanism of injury and the risk factors are recognized (Table 49.1), foot ulcerations are preventable and treatable (Bottomley, 2012).
Table 49.1
Risk factors in the neuropathic foot
| Risk Factor | Possible Injury |
| Loss of protective sensation | Absence of pain-warning input |
| High plantar pressures | Ulcers occurring at peak pressure sites |
| Autonomic neuropathy | Dehydrated inelastic skin |
| Previous ulceration or amputation | Concentration of stress over scar or lesion |
| Foot deformities | Increased local pressures |
| Neuropathic fractures | Increased plantar pressures and foot instability |
| Abnormal foot function | Abnormal load application |
| High activity level | Increased cumulative stress |
| Vascular disease | Devitalized tissue susceptible to injury, poor healing |
| Inadequate footwear or foot care | Decreased protection, instability, poor hygiene |
| Visual loss | Inappropriate assessment of environment, inability to inspect feet |
| Poor insulin regulation | Complications of diabetes |
Neuropathic changes in the insensitive foot include progressive distal polyneuropathy, ischemic mononeuropathy, amyotrophy and neuroarthropathy (Boulton, 2012). A combination of sensory, autonomic, and motor neuropathies of the foot results in symmetrical or asymmetrical loss of perception of pain and temperature. Sympathetic denervation can lead to a progressive mixed-fiber neuropathy with a loss in light touch and vibratory sensation and motor loss in the intrinsic muscles of the foot (Birke, 2002; Jeffcoate & Harding, 2003). Characteristic foot deformities such as hyperextension of the metatarsophalangeal joints, clawing of the toes and distal migration of the adipose cushions (fat pads) under the heel and metatarsal heads result in abnormal weight-bearing patterns and increased plantar pressures (Lemaster et al., 2003). Tissue damage to the insensitive foot may result from continuous pressure that causes ischemia or from concentrated high pressure, heat or cold, repetitive mechanical stress, or infection of the tissues (Driver et al., 2010).
Amyotrophic changes result from a lack of nourishment to the musculature. There is progressive weakening and wasting of muscles accompanied initially by an aching or stabbing pain and resulting in the total loss of muscle function due to atrophy, paresthesia, paralysis, and loss of sensory input (Jeffcoate & Harding, 2003).
Neuropathic arthropathy results from joint erosions, unrecognized fractures, demineralization and devitalization of the bones and articulations of the foot. Typically, these changes result from routine weight-bearing activities in the absence of normal protective proprioceptive and nociceptive functions of the peripheral sensory system. In the limb with intact sensation, pain inhibits functional activities and further trauma to the joints so that the hypertrophic or reparative phases of callus formation can commence. In the insensate limb; however, the injured part is repeatedly traumatized, leading to increased hyperemia and resorption of damaged bone (Pai & Ledoux, 2011; Resnik & Borgia, 2011).
Loss of sensation in the joints and bones of the foot predisposes the neuropathic foot to bony destruction. Midtarsal fractures or dislocations and hypertrophic bone formation may lead to a Charcot’s deformity, which is the collapse of the foot into severe rocker-bottom foot deformity. Charcot’s fracture is evidenced by swelling and increased temperature in the area of bone involvement (Frykberg & Belczyk, 2008). Clinically, neuropathic fractures should be suspected in all patients with signs of inflammation in the absence of an open wound. Differential diagnosis includes: cellulitis, osteomyelitis, pyarthrosis and reflex sympathetic dystrophy.
Evaluation of the neuropathic foot
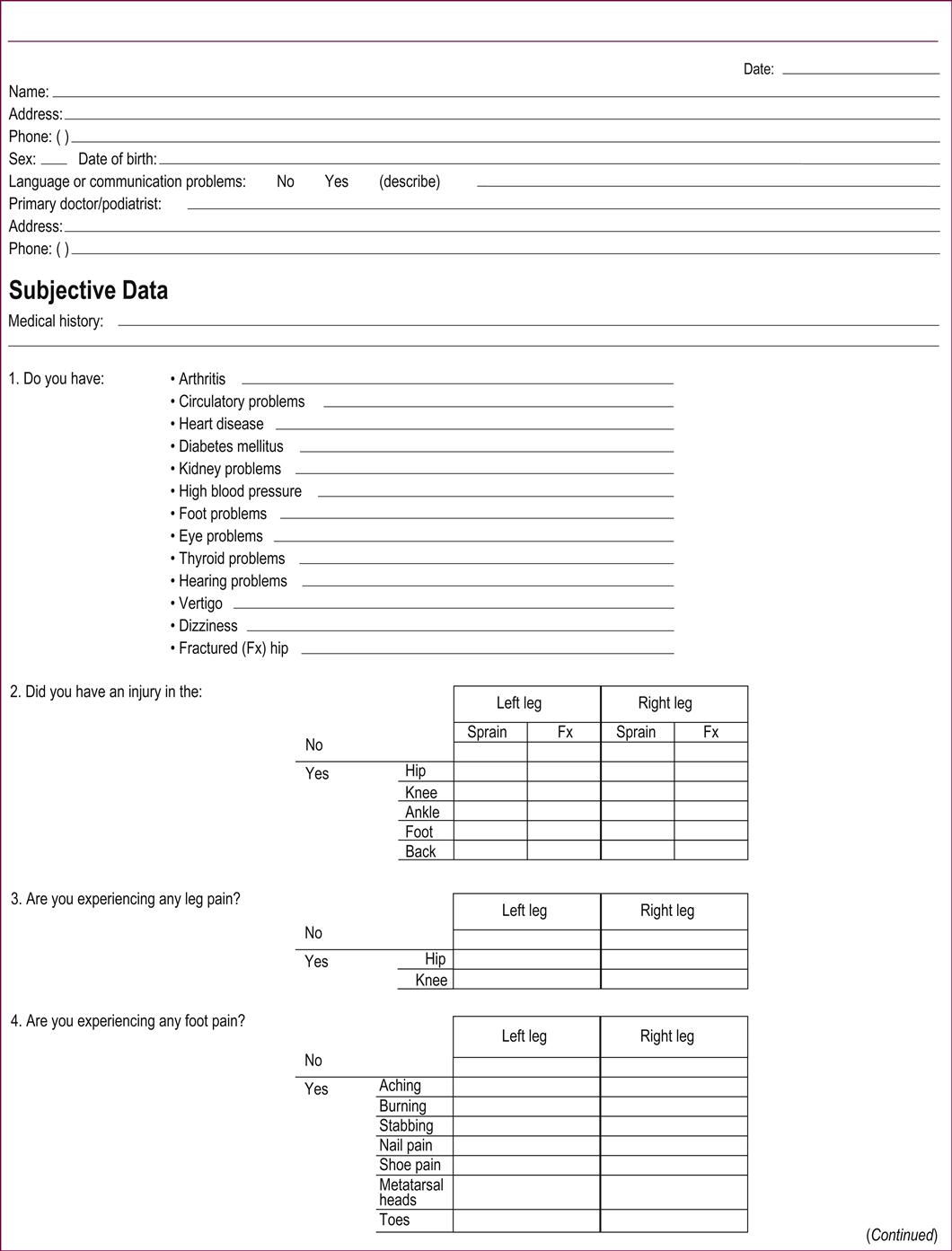
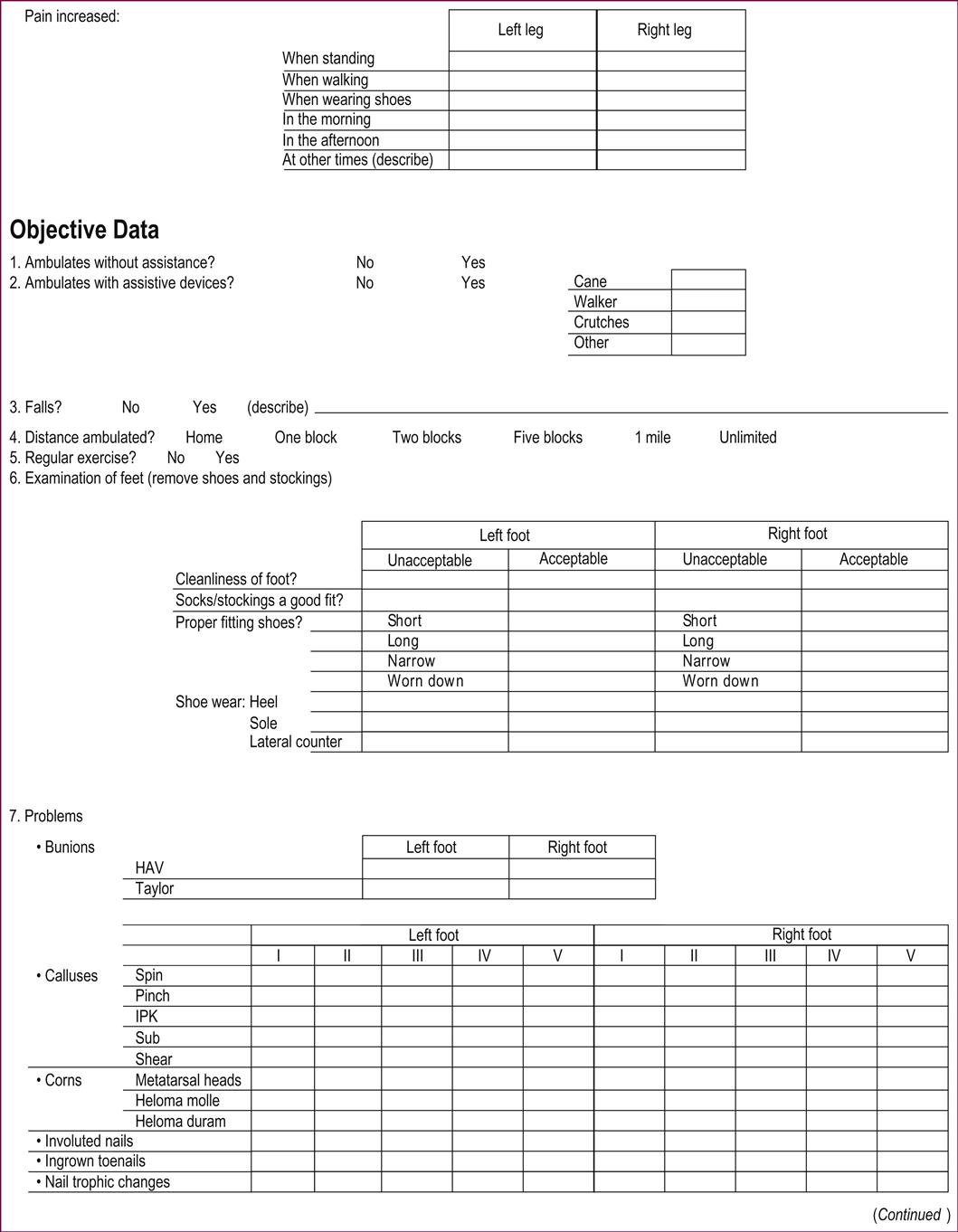
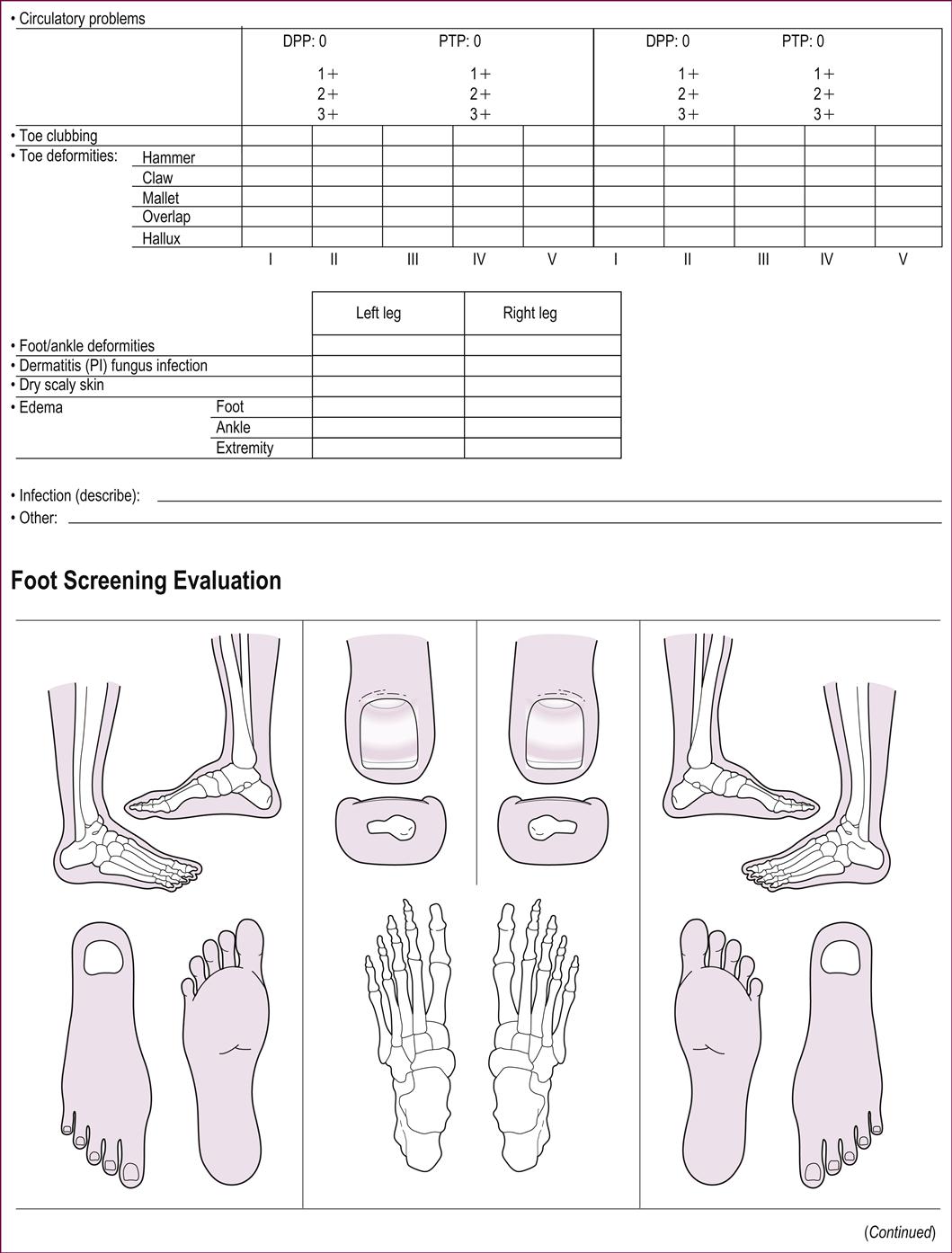
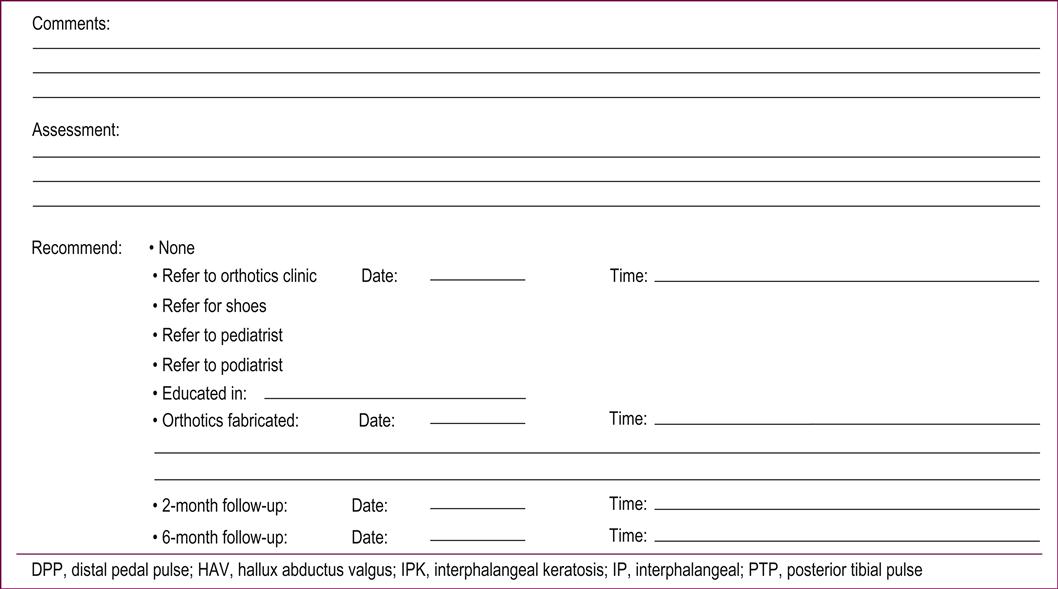
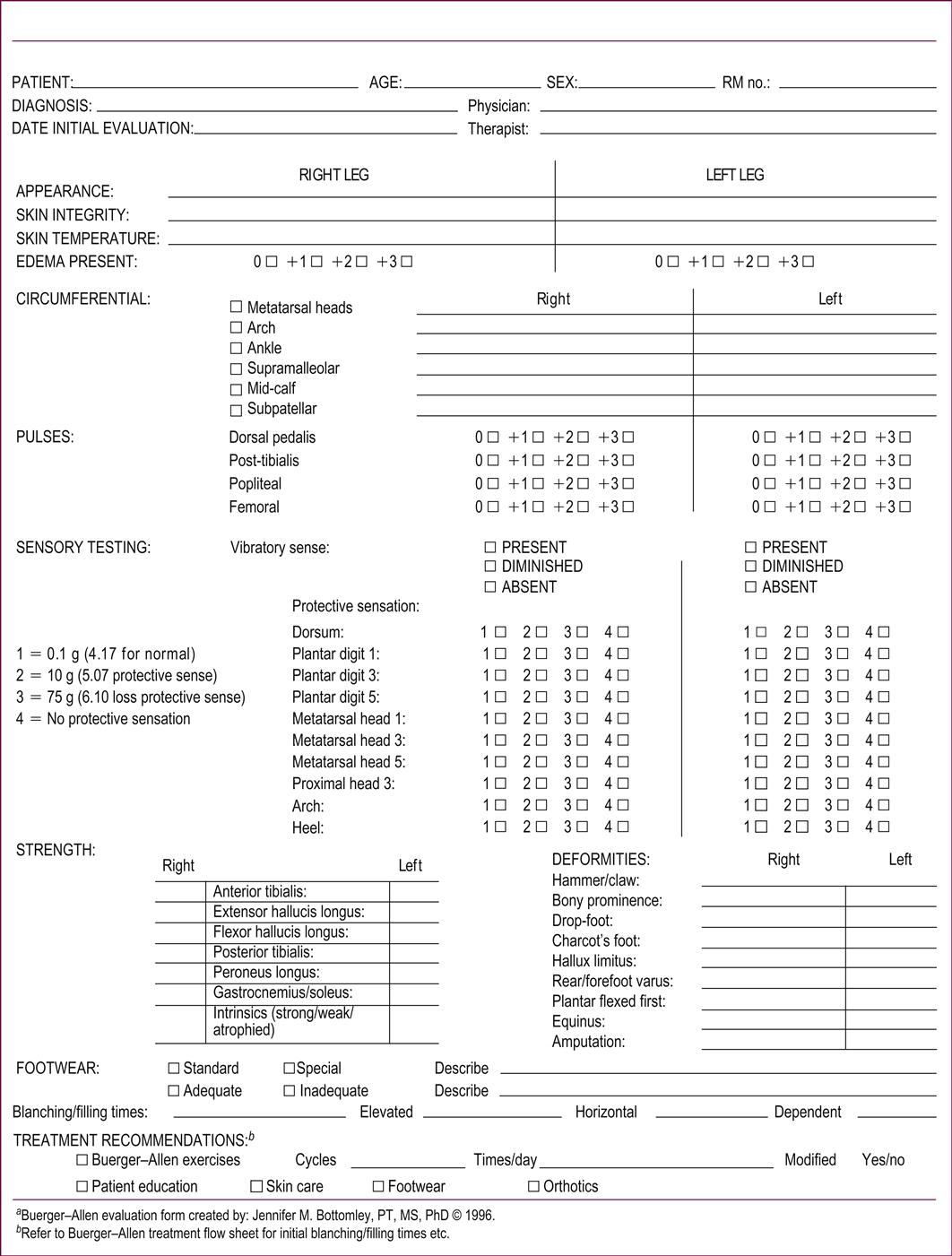
Regular and comprehensive screening of the neuropathic foot is essential for early identification of risk factors that may predispose an elderly individual to injury (Form 49.1). The foot screening is a brief examination to identify the history of any previous ulceration, motor weakness, sensory dysfunction, or deformities that would predispose the foot to local areas of high stress. Circulatory status, color, temperature, general condition and the presence of edema or skin lesions should be assessed. Based on the foot screening, the relative risk of foot complications can be determined for each individual (Bottomley, 2012).
The level of sensory loss that places an individual at risk for foot injury is referred to as loss of protective sensation. The use of nylon monofilaments calibrated to bend at 10 g of force (Semmes–Weinstein monofilaments) is a precise method of determining loss of sensation. The inability to feel a monofilament of 5.07 g has been determined to be the level at which loss of protective sensation occurs (Birke, 2002). A risk classification scheme identifies the individuals most likely to benefit from protective footwear and education (Box 49.1).
Evaluating sensation and neurological involvement
Protective sensation, as defined by Nawcozenski and Birke, is 5.07 g of pressure using the Semmes–Weinstein monofilaments. Specific evaluation of the entire plantar surface of the foot determines areas of sensory loss that are vulnerable to breakdown (Birke, 2002; Van Schie, 2005).
Vibratory and temperature sense are diminished very early in the process of peripheral vascular disease, and that loss compromises proprioception, kinesthesia and awareness of temperature gradients.
The neurological examination requires a reflex hammer, a tuning fork (128 cps) and Semmes–Weinstein filaments. Testing for vibratory, proprioceptive, temperature and protective sensation should be done with the patient’s eyes closed. Distinguish the boundaries of any hyper- or hypoesthesia and determine whether these patterns are symmetrical or asymmetrical. The absence or presence of sweating should be noted. Reflexes to be tested include the patellar reflex and the ankle jerk. As the ankle jerk is increasingly difficult to elicit with increasing age; it may appear to be absent. To aid eliciting this reflex, gently pronate and dorsiflex the foot putting tension on the Achilles tendon and gently tap the tendon. Test for the Babinski reflex to determine whether there is a superficial plantar response. To determine if there is clonus, forcibly dorsiflex the foot at the ankle and clonus will be initiated at end range. To test for loss of balance, have the individual stand with eyes closed and feet close together and compare this to the same stance with the eyes open (Romberg’s sign) (Chantelau et al., 2007; Kruse et al., 2010; Ites et al., 2011).
Muscle strength should be tested in all lower extremity muscles using a graded manual muscle test. Again, symmetry should be noted. Gait evaluation is a helpful adjunct to muscular evaluation to determine unsteady gain patterns, foot-drop or the presence of a ‘steppage’ gait. Range of motion and joint mobility should be evaluated and any deformities (e.g. Charcot joints, hammer, claw, or mallet toes, hallux abductus valgus) should be noted, as these abnormalities are usually indicative of intrinsic foot muscle weakness. Trophic nail changes should also be evaluated (Driver et al., 2010).
The Semmes-Weinstein monofilament instrument is a reproducible and accurate way to test sensation, and is reliable in predicting which individuals are at risk for ulceration due to loss of protective sensation. The Carville group from the G.W. Long Hansen’s Disease Center in Carville, LA, measured protective sensation using the Semmes–Weinstein monofilaments and found that individuals who could not feel the 5.07 monofilament were at greater risk for skin breakdown than those who could feel this level of stimulation. They demonstrated that 5.07 was the threshold of protective sensation. Standardization of sensory testing is crucial in evaluation, so that adequate protective measures can be taken to prevent feet at risk from developing ulcers (Birke, 2002; Boulton, 2012).
Evaluation of circulatory status
Vascular evaluation should include the palpation and grading of the femoral, popliteal, dorsalis pedis and posterior tibial pulses, and the observation of other clinical signs and symptoms indicating vascular compromise in the lower extremities. These include intermittent claudication, foot temperature (i.e. cold feet), nocturnal and rest pain (including pain relieved by dependency), blanching on elevation, delayed venous filling time after elevation, dependent rubor, atrophic skin, absence of hair growth and presence of gangrene. Any lesions or areas of hyperkeratosis or discoloration should be observed and documented (Young et al., 2011).
To differentiate an organic disorder such as blockage of the lumen of the vessel from a vasospastic condition, temporary dilation of the vessel in question is a useful vascular test. This is accomplished by using an arterial tourniquet for 3 minutes and then releasing it. The perfusion distal to the tourniquet should increase if the condition is due to vasospasm (Chantelau et al., 2007).
Observation of blanching and filling times is accomplished by using the Buerger–Allen vascular assessment (see Forms 49.2 to 49.4). A stopwatch is used to determine the time it takes the veins in the distal part of the foot to fill with blood after they have been drained by elevating the leg. Basically, this is a means of appraising the general circulation in the foot. The arterial blood being pumped into the dependent leg diffuses into the arterioles, the capillaries and the venules, and then into the veins of the foot. The time of venous filling is subject to several variables: arterial blood pressure, the caliber of the arteries, the volume of blood reaching the capillary bed of the foot with each thrust of the heart and the rate of venous return. A filling time of up to 20 seconds indicates reasonably good collateral circulation. A venous filling time longer than 20 seconds is indicative of a compromised peripheral vascular system and of venous insufficiency (Young et al., 2011).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







