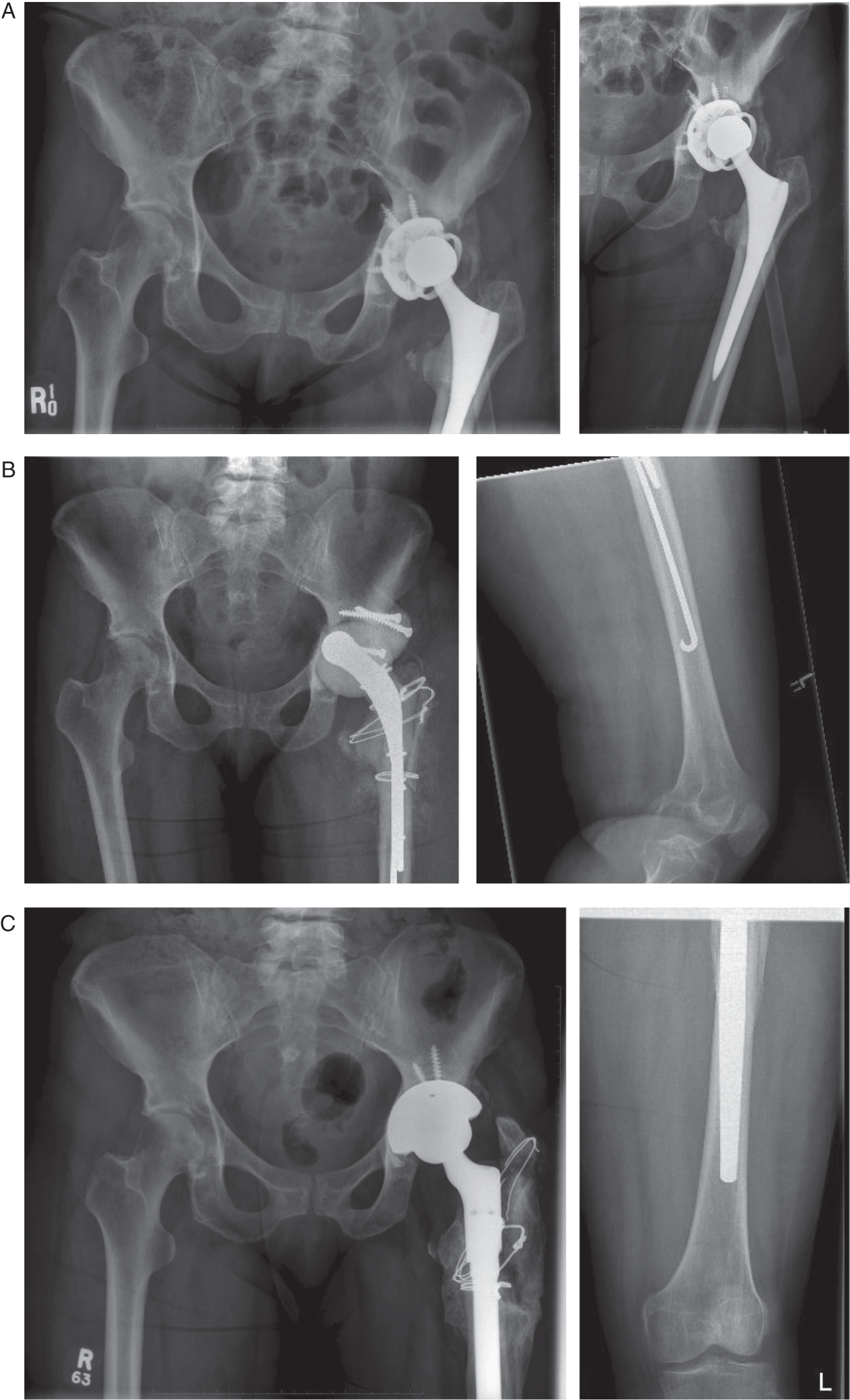
Sebastián A. León MD1, Xin Y. Mei MD2, and Paul R. Kuzyk MD MASc3 1 Hospital San José, Santiago, Chile 2 Division of Orthopaedic Surgery, Department of Surgery, University of Toronto, Toronto, ON, Canada 3 Mount Sinai Hospital, University of Toronto, Toronto, ON, Canada Figure 31.1 Radiographs: (A) preoperative; (B) first‐stage; (c) second‐stage. Source: Sebastián, Xin Y. Mei, Paul R. Kuzyk. Current guidelines recommend a combination of blood tests (ESR, CRP) and synovial fluid analysis for workup of suspected PJI. Recent studies have shown promising results using synovial fluid biomarkers in the diagnosis of PJI. PJI affects 1–2% of patients after primary THA,1,2 and is responsible for 12.8% of revision THAs.3 Current guidelines from the Musculoskeletal Infection Society (MSIS) and the International Consensus Group recommend obtaining serum ESR and CRP levels in the workup of all patients with suspected PJI.4,5 Despite their universally accepted use, neither test is completely reliable in diagnosing PJI. To improve the accuracy of this diagnosis, several synovial fluid biomarkers have been investigated and shown to outperform traditional tests in diagnosing PJI.4,6 Of these, alpha‐defensin and leukocyte esterase (LE) have shown promising results. Alpha‐defensin is an antimicrobial peptide released by activated neutrophils that has the ability to adhere to and destroy the bacterial cellular membrane.7 It is unique to neutrophils found in infected joints, and is not released by neutrophils in aseptic joint inflammations such as gout.8 There are currently two commercially available methods for measuring alpha‐defensin in synovial fluid. The enzyme‐linked immunosorbent assay (ELISA)‐based alpha‐defensin immunoassay measures the fluorescent signal released by tagged antibodies binding to alpha‐defensin antigen, and provides a quantitative readout within 24 hours. By contrast, the alpha‐defensin lateral flow test is a paper‐based platform that detects the presence or absence of alpha‐defensin in three drops of a diluted aspirate placed on a test device, and provides a binary readout within 20 minutes.9 Although these tests are easy to perform, they are much more costly than conventional tests. LE is an enzyme secreted by activated neutrophils and is currently part of the minor diagnostic criteria of PJI according to MSIS and International Consensus Meeting guidelines.10,11 Its presence in synovial fluid can be detected using colorimetric strip tests.12 Blood‐contaminated synovial fluid samples can interfere with interpretation of the colorimetric strip; however, the use of a centrifuge to separate synovial fluid from contaminant blood can help yield accurate results.13 Advantages of the LE test include it being quick and easy to perform, as well as the low cost of the colorimetric strip. A recent systematic review and meta‐analysis by Wyatt et al. evaluated the diagnostic accuracy of alpha‐defensin (six studies) and LE (five studies) for PJI.15 The pooled sensitivity and specificity of alpha‐defensin were 1.00 (95% confidence interval [CI]: 0.82–1.00) and 0.96 (95% CI: 0.89–0.99), respectively. The pooled sensitivity and specificity of LE were 0.81 (95% CI: 0.49–0.95) and 0.97 (95% CI: 0.82–0.99), respectively. Diagnostic accuracy, as defined by the area under the receiver operating characteristic curve, was 0.99 (95% CI: 0.98–1.00) for alpha‐defensin and 0.97 (95% CI: 0.95–0.98) for LE. Emerging evidence suggests that the alpha‐defensin lateral flow test may have lower diagnostic accuracy than its ELISA‐based immunoassay counterpart. A 2018 systematic review comprising 601 patients across seven studies showed the ELISA‐based immunoassay to have superior overall diagnostic value compared with the lateral flow test (AUC, 0.98 vs 0.75) with higher sensitivity (96%, 95% CI: 90–98% vs 71%; 95% CI: 55–83%; p <0.001) but no difference in specificity (96%, 95% CI: 93–97% vs 90%; 95% CI: 81–5%; p = 0.060).9 A meta‐analysis by Berbari et al. evaluated the diagnostic accuracy of serum biomarkers for PJI.14 Data were pooled from 30 eligible studies. The pooled sensitivity and specificity of ESR were 75% (95% CI: 72–77%) and 70% (95% CI: 68–72%), respectively. The pooled sensitivity and specificity of CRP were 88% (95% CI: 86–90%) and 74% (95% CI: 71–76%), respectively. The diagnostic odds ratio was 7.2 (95%: CI 4.7–10.9; 25 studies) for ESR and 13.1 (95% CI: 7.9–21.7; 23 studies) for CRP. Shahi et al. evaluated the diagnostic odds ratios (DORs) of five routine laboratory markers for PJI in 4662 revision THAs.17 The DORs for PJI, from highest to lowest, were LE: 30.06 (95% CI: 17.8–50.7), synovial fluid white blood cell count: 29.4 (95% CI: 20.2–42.8), CRP: 25.6 (95% CI: 19.5–33.7), synovial fluid PMN percentage: 25.5 (95% CI: 17.5–37.0), and ESR: 14.6 (95% CI: 11.5–18.6). The authors concluded that among the minor diagnostic criteria, LE has the best performance. Tarabichi et al. reviewed the records of 319 patients who had ESR and CRP screening prior to LE testing for diagnosis of PJI.18 The authors reported that when LE is concordant with ESR and CRP levels it can effectively rule out or diagnose PJI with >95% certainty. When discordant, only stricter LE thresholds (2+ or negative) are adequate to suggest a change in clinical decision‐making. In this context, intermediate LE values require further diagnostic testing. Shahi et al. reported that prior antibiotic administration is associated with lower ESR and CRP values in comparison with no antibiotics, with difference of medians (DOM) of 15 mm/h (p = 0.018) and 58 mg/L (p = 0.038), respectively, which may lead to increased risk of false negative tests.16 The same group later reported that alpha defensin levels did not vary significantly with antibiotic administration (DOM 0.68; 95% CI: −0.98–1.26; p = 0.451).19 Alpha defensin was also found to have higher sensitivity (100%; 95% CI: 88.4–100.0%) in diagnosing PJI than ESR (69.0%; 95% CI: 49.17–84.72%; p = 0.001) and CRP (79.3%; 95% CI: 60.3–92.0%; p = 0.009). Preliminary studies have shown alpha defensin to be highly sensitive and specific in diagnosing PJI, with superior performance compared to ESR and CRP. Results also appear to remain unaffected by prior antibiotic administration. However, the high cost of the test remains a barrier to its routine use. The LE strip test is inexpensive and has also shown superior performance in comparison to routine serum biomarkers such as ESR and CRP. Results are most promising when used in conjunction with ESR and CRP. The 2018 International Consensus Meeting on Musculoskeletal Infection supported the use of the alpha‐defensin lateral flow test and the LE test strip in the diagnosis of PJI.20
31 The Infected Total Hip Arthroplasty
Clinical scenario
Top three questions
Question 1: In patients with suspected PJI, are novel biomarkers such as alpha‐defensin and leukocyte‐esterase better screening tests for than ESR, CRP, and synovial fluid PMNs?
Rationale
Clinical comment
Available literature and quality of the evidence
Findings
Resolution of clinical scenario
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





