7.15 The fascial distortion model Mainstream medicine takes little advantage of this most complex information network. Physicians increasingly ignore it and instead use technological investigation devices. The patient gets the impression that his perception and description of pain or discomfort disturbs, rather than supports, the diagnostic process. Accordingly, magnetic resonance imaging (MRI) scans are used to locate the disorder even though key studies suggest that MRI scans are, in spite of their spectacular resolution, questionable tools to locate the source of pain (Jensen 1994; Chou 2009). This frustrating experience was the origin of Stephen Typaldos’ fascial distortion model (FDM) (Typaldos 2002). Typaldos, an osteopath and emergency physician, found it a frustrating experience to learn how little medical and osteopathic treatments could help patients suffering from so-called soft tissue injury. Conditions such as sprained ankles, lower back pain, and neck pain seemed to be almost unresponsive to the treatments he could offer within an emergency department. Improving his manipulation skills or increasing the diagnostic effort (MRI, ultrasound, nerve conduction, etc.) did not improve the outcome. Typaldos’ impression was that the patients had subconscious understanding of the nature of their condition and of possible solutions. Studying the patients’ stories and gestures, he found recognizable entities for which he saw fascia as the common denominator. Typaldos postulated three-dimensional alterations of fascia that could apparently be repaired by the maneuvers and techniques he had successfully performed under the guidance of his patients. Typaldos discovered six “fascial distortions”, as he called these new diagnoses (Table 7.15.1). Table 7.15.1 Fascial distortion types as described by Typaldos
The patient as expert – the Typaldos model
Fascial distortion type
Description
Trigger band (TB)
Longitudinal crack within a band
Herniated triggerpoint (HTP)
Gap opening within a sealing fascia, with resultant protrusion
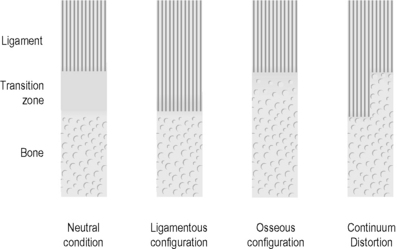
Continuum distortion (CD)
Shift of minerals within transition zone between bone and ligament
Folding distortion (FD)
Overstretching of folds in “accordion”-like structure
Cylinder distortion (CyD)
Entanglement of cylindrical coils in skin
Tectonic fixation (TF)
Loss of gliding ability in a joint
Musculoskeletal Key
Fastest Musculoskeletal Insight Engine