The Envelope of Function
Scott F. Dye
The primary goal of orthopaedic surgical treatment is universally considered to be “restoration of musculoskeletal function.” Until now, the definition of restoration of musculoskeletal function has been conceptualized primarily in structural and biomechanical terms. It is a common belief that if one can restore normal structural and biomechanical characteristics following a joint injury such as the achievement of normal instrumented laxity in an anterior cruciate ligament (ACL)-reconstructed knee, then that joint has been “fixed” and its function restored. Further, it is thought, if function has been restored then it will be safe to return such a knee to high-demand sports like soccer and, in addition, the development of long-term arthritis will be prevented.
Recent reports have documented, however, that despite the achievement of normal structural and biomechanical indicators in knees having undergone ACL reconstruction procedures (normal laxity measurements, full range of motion, excellent muscle strength, and normal short-term x-rays), many such joints are manifesting the very disturbing development of early degenerative arthritis.1,2,3,4,5 Such joints are emblematic of the failure of what can be termed the structural and biomechanical paradigm. This structural paradigm currently forms the conceptual foundation for most clinical orthopaedic practice (i.e., restore structural and biomechanical normalcy and function is restored). However, it is becoming increasingly apparent that restoration of normal structural and biomechanical characteristics is insufficient to prove the restoration of full physiological function of an injured musculoskeletal system. The consideration of metabolic and physiological factors—biological characteristics of living tissues—is essential to understand the full meaning of restoration of musculoskeletal function.
A new and alternative orthopaedic paradigm characterized by the term tissue homeostasis has been developed in recent years that takes into account metabolic characteristics of living musculoskeletal systems.6,7,8 The term tissue homeostasis may be new to the reader. The word “homeostasis” is most often associated with the constant maintenance, within a certain range, of soluble factors in the blood such as levels of glucose, CO2, or ionic calcium. The concept of tissue homeostasis encompasses the more complex phenomenon of normal physiologic processes of volumes of living cells within a certain range. All living musculoskeletal structures are composed of cells that, under normal circumstances, are constantly metabolically active, representing continuous molecular maintenance of these tissues. Presently, the most readily available method of manifesting tissue homeostasis is by means of technetium bone scintigraphy, which is capable of geographically revealing osseous homeostasis9 (Fig. 4.1). The paradigm of tissue homeostasis has been formulated into a practical concept by means of the envelope of function, which represents the safe, homeostatic loading capacity of a joint or musculoskeletal system.7 These concepts will be discussed further in this chapter.
The Knee as Biologic Transmission
If our task as orthopaedic surgeons is to restore musculoskeletal function, what then, is the function of a joint such as the knee? In 1988, Alfred Menschik of Vienna, Austria, in a personal communication to this author, stated that he thought the knee could be best thought of as a kind of “stepless transmission.” After much consideration and discussion with many members of the international orthopaedic community, it became clear that this was an accurate and profoundly valuable insight into musculoskeletal function. The function or purpose of the knee (and by extension, all diarthrodial joints) is to accept, redirect, and dissipate a broad range of biomechanical loads without either metabolic or structural failure.
A transmission, in an automobile, for example, is a highly complex system designed to accept, redirect, and dissipate a range of mechanical loads without overheating or outright structural failure. In this analogy, the knee ligaments represent sensate, adaptive nonrigid linkages within the biologic transmission. An ACL-injured knee, for example, can thus be understood as a transmission with linkage failure that is vulnerable to symptoms of giving way, analogous to a mechanical transmission slipping out of gear. The menisci can be visualized as mobile, sensate bearings within the transmission. A knee with a torn meniscus is like a transmission with structural failure of a bearing. The patellofemoral joint functions as a large slide-bearing withstanding the highest loads within the biologic transmission. The muscles in this analogy function as living cellular engines that provide (in concentric contraction), motive forces across the knee, and (in eccentric contraction) also act as brakes and dampening systems.
The Envelope of Function
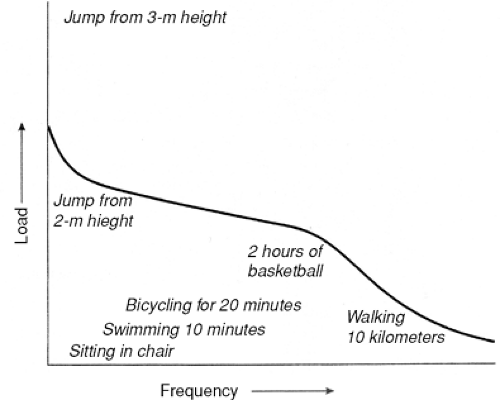
The functional capacity of a mechanical transmission—its torque envelope—is defined as the range of loading (torque) that can be safely placed across such a system without failure (overheating or overt structural damage). One can similarly represent the safe load-transference capacity of a living human joint such as the knee, by a load/frequency distribution, which defines and delineates this safe range of load acceptance and transference in a given period of time.7 This range of homeostatic loading is termed the envelope of function (Fig. 4.2). An alternative term I frequently use in communications with the lay public is the envelope of load acceptance.
In its simplest form, the envelope of function is a two-dimensional graph with increasing load applied across a joint on the vertical (Y) axis and increasing frequency of loading on the horizontal (X) axis. Loads applied across a living joint within the envelope of function are not only compatible with physiologic normalcy (tissue homeostasis) of all components, but are actually inductive of it as well. If, for example, a normal 20-year-old person is forced to decrease loading across the knees for a prolonged period of time by being kept at strict bed rest for a month, loss of tissue homeostasis manifested by muscle atrophy and calcium loss from bone will likely ensue. The pathophysiologic effects of such persistent subphysiologic underloading are often described as “disuse”10 (Fig. 4.3).
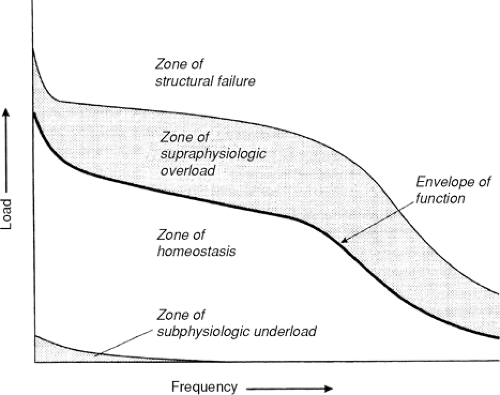 Figure 4.3 Graph showing the four different zones of loading across a joint. The area within the envelope of function is the zone of homeostasis. The region of loading greater than that within the envelope of function but insufficient to cause macrostructural damage is the zone of supraphysiologic overload. The region of loading great enough to cause macrostructural damage is the zone of structural failure. The region of decreased loading over time resulting in a loss of tissue homeostasis is the zone of subphysiologic underload. (Adapted from
Get Clinical Tree app for offline access
Dye SF. The knee as a biologic transmission with an envelope of function. Clin Orthop Relat Res 1996 Apr; (325):10–18, with permission.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|