Anterior Cruciate Ligament Reconstruction
J. Richard Steadman
One of the most common knee injuries during sporting activities is a torn anterior cruciate ligament (ACL). Various treatments have been described in the literature through the years; however, the most common treatment has been the ACL reconstruction. Although several surgical techniques are currently in use, my personal choice is the two-incision bone-tendon-bone patellar tendon operation. More than 30 years of experience and 1,800 reconstructions have led to a repeatable technique with predictable outcomes. Several factors are required for success. These include patient selection, the timing of surgery, technical considerations, and postoperative rehabilitation.
The most common injury seen is the acute injury. If patients with these injuries are unwilling to modify their active lifestyle, then ACL surgery is recommended. In the chronic ACL-injured knee, an ACL is reconstructed if functional instability is interfering with sports or the patient’s occupation. A reconstruction is also recommended for the patient who is experiencing giving way because this places the menisci and articular cartilage at risk of injury. Another option for treatment, the “healing response,” is discussed in Chapter 10.
Patient Selection
There are many factors to consider in patient selection, one of which is age. In the skeletally immature patient, the possibility of epiphyseal injury must be considered. Although few cases of growth disturbances have been documented, a recent study that surveyed the ACL study group showed 15 disturbances.1 In my practice, the risk of even one growth disturbance limits the use of ACL reconstruction in the skeletally immature patient.
ACL reconstruction in the older athlete has been controversial. In a review of a series of my patients, the increased age of a patient was not a factor if the patient met other patient selection criteria.2 Older patients are given the choice of modifying their activity level. However, as “baby boomers” age, more and more people are staying active later in life. Also, if the patient has the appropriate
injury pattern, the older patient is given the option of a less-invasive procedure, the healing response. This technique has also been used in treating the skeletally immature athlete.3 Most patients whose exercise consists of cycling, swimming, and walking do not require a reconstruction. However, those patients participating in sports requiring more stability in the knee, such as skiing and change-of-direction sports, may need an ACL reconstruction.
injury pattern, the older patient is given the option of a less-invasive procedure, the healing response. This technique has also been used in treating the skeletally immature athlete.3 Most patients whose exercise consists of cycling, swimming, and walking do not require a reconstruction. However, those patients participating in sports requiring more stability in the knee, such as skiing and change-of-direction sports, may need an ACL reconstruction.
The timing of surgery following injury has previously been debated.4,5,6,7,8,9 In one study of my patients, we showed that there were no differences in the prevalence of arthrofibrosis between patients operated within 3 weeks of injury compared with patients operated at more than 3 weeks, if they met defined preoperative criteria.10 The criteria for performing an ACL reconstruction on an acutely injured patient included (i) a minimum active range of motion of 0 to120 degrees, (ii) performing a straight-leg raise similar to the unaffected side with no loss of extension, and (iii) active quadriceps control demonstrated by quadriceps definition symmetric to the unaffected side, while performing quadriceps contraction. In recent years we have added a fourth criterion. Only minimal temperature differential between the patient’s knees is acceptable. Increased temperature is an indication of inflammation and could predispose the knee to arthrofibrosis. The presence of a stable meniscal tear that is not locked is not a contraindication to aggressive range of motion. The physical environment around the knee is a more important factor to consider than the number of days since the injury.
Another important consideration in patient selection is the presence of injuries associated with the ACL injury. Some injuries may require changes in surgical technique or timing. If the patient has an unstable or locked meniscal tear, which is repairable, the repairs are done in two stages. The meniscus is repaired and rehabilitated prior to reconstruction. This is because of the required differences in rehabilitation. The meniscus repair is followed by 8 to 12 weeks of rehabilitation, which is followed by the ACL reconstruction.
Other injuries that may change patient selection include chondral injuries of the patellofemoral compartment, which may require that an allograft ACL reconstruction be done in order to place less pressure on the defect. If microfracture of the trochlea or patella is required, surgery may be done in two stages, with microfracture done first, and the reconstruction done after initial rehabilitation is completed. This takes approximately 3 months.
Surgical Technique
The goal of ACL reconstruction is to re-create the constraints on motion supplied by the native ACL. To create success after ACL reconstruction, several conditions must be met.
The tunnels must be properly positioned to assure ideal graft length.
The graft must have adequate strength.
Impingement must be avoided for the reconstruction to be successful.
The fixation of the graft in the tunnels must allow for early range of motion.
The reconstruction must restore normal biomechanics of soft tissue.
The ACL can be reconstructed using a variety of techniques. My preference is the two-incision bone-tendon-bone patellar tendon.
Graft Choice
Patellar tendon bone-tendon-bone, semitendinosus or semitendinosus and gracilis, quadriceps tendon, and allograft can all replace the ACL.11,12,13 My personal choice for graft is the patellar tendon bone-tendon-bone autograft or allograft with a two-incision technique. The patellar tendon provides adequate strength,13 and allows for bone-to-bone fixation and healing,14 and the tendon graft site regenerates. For any technique to be successful, it must be reproducible. The tunnel position must be correct 100% of the time. There must be no graft impingement, either medial to lateral or superior to inferior. The technique allows for reliable fixation. One must always have a backup plan if an unexpected complication occurs.
The use of allograft has increased because of improved graft testing for disease transmission and better preparation techniques, which have minimal effect on graft strength. This graft is used if there are patellofemoral problems in revisions, and if the patient has a preference after hearing the preoperative explanation. A recent study of our patients has shown that results from allograft reconstructions are similar to autograft results.
The Two-Incision Technique
The technical advantages of the two-incision technique include the reproducibility, the ability to check the posterior position and adjust the graft’s position on the femur, and the flexibility of the anterior position. The fixation is predictable, and if complications occur a backup plan can be implemented. The two-incision technique also decreases the risk of potential pitfalls that exist with the single-incision technique.15,16 The outside-in drilling on the femoral side allows the femoral position to be near the most posterior attachment of the native ACL.
TIP: If problems are encountered during a single-incision technique, this technique is an ideal option allowing for excellent fixation and anatomic placement.
Arthroscopic Evaluation and Notch Preparation
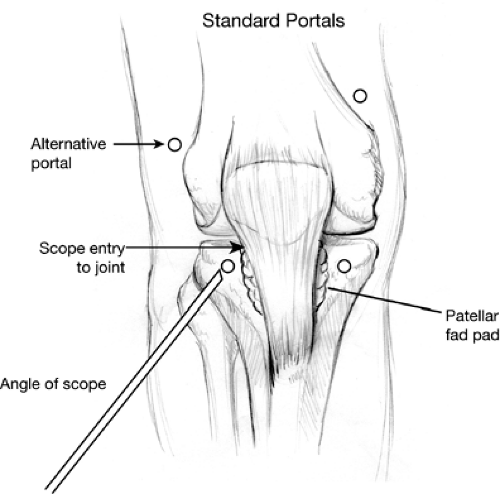
Three arthroscopy portals are made in the superomedial, inferomedial, and high inferolateral positions. The high inferolateral portal (Fig. 8.1) is based lateral to the lateral patella, 0.5 cm proximal to the distal pole of the patella in a “soft spot.” The 11-blade knife is angled 20 to 30 degrees cephalad. Care is taken to go through the capsule only, in order to avoid lacerating the articular cartilage of the patella or lateral condyle. The inflow cannula is placed through the superomedial portal, the camera is placed through the inferolateral portal, and the working instruments are shuttled in and out of the inferomedial portal. A diagnostic arthroscopy of the knee is performed. All compartments of the knee are examined to determine if any other injuries exist, which could be a contraindication to ACL reconstruction. The ACL rupture is examined arthroscopically.
An anterior notch width of at least 18 mm is desirable to help avoid lateral wall impingement (Fig. 8.2). Most arthroscopic pituitary rongeurs are 18 mm in width when fully opened, and can be used as a guide for notch size. A stenotic notch is widened using a curved osteotome and/or a motorized burr on the lateral wall. The posterior notch is also important. Using a 70-degree scope, the lateral wall is contoured to form an oval surface, avoiding impingement in this important area.
Graft Harvest
Along the central patellar tendon a longitudinal skin incision is made between a point 1 cm proximal to the inferior pole of the patella and the tibial tubercle, with the knee passively flexed (Fig. 8.3). The subcutaneous tissue is dissected down to the level of the peritenon. The peritenon is incised and elevated as a distinct layer to allow closure after harvesting of the tendon is completed (Fig. 8.4). The peritenon is kept intact throughout its entirety. Dissection under the peritenon is performed until the medial and
lateral borders of the tendon are defined. The width of the tendon is measured (Fig. 8.5). One third of the tendon is harvested, with a 10-mm graft usually chosen. If the width is less than 27 mm, a 9-mm graft is used. The tendon is divided in line with its fibers from the patella and down to the tubercle.
lateral borders of the tendon are defined. The width of the tendon is measured (Fig. 8.5). One third of the tendon is harvested, with a 10-mm graft usually chosen. If the width is less than 27 mm, a 9-mm graft is used. The tendon is divided in line with its fibers from the patella and down to the tubercle.
 Figure 8-2. Pituitary rongeurs are used to measure the width of the anterior notch. The desired width is 18 mm, which is the width of most pituitary rongeurs when fully opened. |
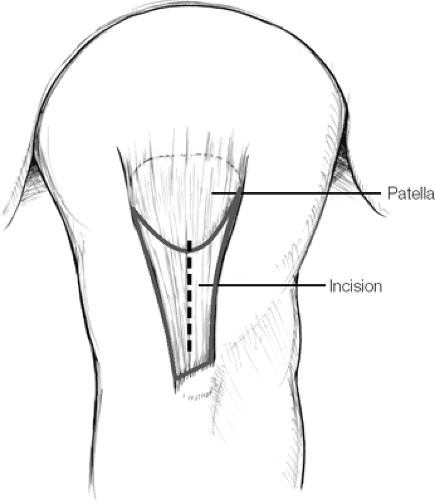 Figure 8-3. The skin incision for the harvest of the patellar tendon autograft. The incision is 1 cm proximal to the inferior pole of the patella and the tibial tubercle. |
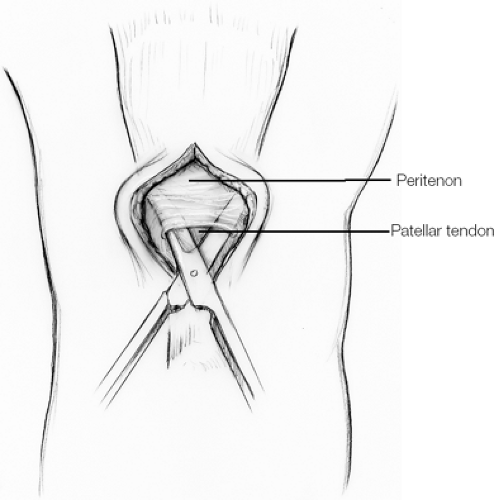 Figure 8-4. The elevated peritenon is excised as a distinct layer to allow for closure after harvesting is complete. |
A 2-mm drill bit is used to weaken the distal attachments of the tibial bone block (Fig. 8.6), which is 30 to 40 mm in length. (If an oscillating saw is used at the corners, it could go past the point and leave a stress riser, making the area more susceptible to fracture.) Cuts perpendicular to the tibia are then made on the medial and lateral sides of the graft. A curved gouge connects the drill holes and the saw cuts. Two drill holes are placed through the bone plug and a number 5 FiberWire (Arthrex, Naples, FL) suture is placed through the holes. The tendon is freed from the underlying fat pad.
Next, a knife is used to outline a 25 ÷ 10 mm area on the distal patella. On the patellar side, a 2-mm drill is used again to define the corners of the bone blocks and across the proximal edge of the patellar graft. The patellar block is about 25 ÷ 10 mm. Lateral saw cuts are made at a 10-degree angle to make a more trapezoidal graft. A curved gouge is used to remove the bone piece (Fig. 8.7). A pick is used to make holes in the patella just posterior to the tendon, weakening the patella at the inferior pole so that the patellar bone block does not break into the joint on harvest.
Graft Preparation
Bone plugs are trimmed with scissor and bone rongeurs until they can be passed through a 9-mm graft sizer (Fig. 8.8). All bone that is removed is saved to fill the patellar and tibial defects on closure. Maximizing the size of the bone plugs within the respective tunnels is important to obtain rigid fixation of the graft. Two number 5 FiberWire sutures are placed in each bone block. The tibial block is generally
35 mm in length ÷ 10 mm, and the patellar block is usually 25 ÷ 9 mm. If 25 mm represents more than one third of the length of the patella, a shorter graft is generally harvested instead. In this case, the minimum patella graft length is 20 mm.
35 mm in length ÷ 10 mm, and the patellar block is usually 25 ÷ 9 mm. If 25 mm represents more than one third of the length of the patella, a shorter graft is generally harvested instead. In this case, the minimum patella graft length is 20 mm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree