The Dermatophytoses
Bernhard L. Wiedermann
Dermatophytosis refers to colonization of the skin with members of the dermatophytic fungi of the genera Trichophyton, Microsporum, and Epidermophyton. Clinical disease may appear as a consequence of the host’s response to this colonization. The condition has been recognized since antiquity and was termed herpes by the Greeks, in reference to the tendency of lesions to creep in a circular fashion. Later, the Romans used the term tinea, meaning “worm” or “moth,” to indicate a presumed association of the disease with insects. The modern term ringworm is a combination of these two historical names.
The affected body site is incorporated into commonly used clinical nomenclature. Thus, tinea capitis refers to dermatophytosis of the scalp, lesions of the trunk and extremities are termed tinea corporis, foot involvement is named tinea pedis, perineal disease is known as tinea cruris, and dermatophytosis of the nails is called tinea unguium.
ETIOLOGY
The three genera of dermatophytes refer to asexual (imperfect or anamorph) stages of the fungi. A completely different nomenclature is used to speak of the sexual (perfect or teleomorph) forms, which will not be discussed here. Confusion may arise from this distinct nomenclature and from the classification of dermatophytes according to natural habitat as geophilic
(soil saprophyte), zoophilic (animals as primary hosts), or anthropophilic (humans as primary hosts). Nonetheless, this latter classification is useful in the evaluation of outbreaks or persistence of infection in individuals.
(soil saprophyte), zoophilic (animals as primary hosts), or anthropophilic (humans as primary hosts). Nonetheless, this latter classification is useful in the evaluation of outbreaks or persistence of infection in individuals.
To date, approximately 40 different dermatophytes have been identified, but only 11 commonly cause disease in humans. The most common organisms causing disease in the United States are Trichophyton tonsurans, T. rubrum, T. mentagrophytes, Microsporum canis, and Epidermophyton floccosum.
EPIDEMIOLOGY
Age is a determinant for some dermatophyte infections. For example, tinea pedis is found commonly in adults but rarely in children. In contrast, tinea capitis occurs commonly in children but rarely after puberty. However, previous data suggesting that tinea capitis clears at puberty probably are incorrect; most cases resolve within a year regardless of therapy or age of the patient.
Gender also may play a role in some dermatophyte infections. Tinea capitis caused by Trichophyton in adults appears to occur more commonly in women. Tinea cruris occurs more commonly in men, which may be related in part to anatomic differences rather than genetic causes.
Similarly, associations of infections with specific populations, such as tinea capitis with African American children, may relate more to physical (coiling of hair shafts) than to genetic factors. Other environmental issues, such as geographic site, animal exposure, presence of trauma, or immunocompromising conditions (particularly those involving cell-mediated immunity) may predispose to development of dermatophytosis.
PATHOGENESIS AND PATHOLOGY
Infecting organisms are acquired from soil, animal, or human sources and colonize keratin-containing tissues. Direct contact may not be necessary for transmission. The dermatophytes possess the relatively unique ability to use keratin as a substrate for growth, which allows them to invade keratin-rich tissues. During the initial incubation period, the organism grows in the stratum corneum of the skin and then progresses in accord with the growth rate of the particular organism and the rate of squamous cell turnover in the host. The site of disease enlarges and spreads locally. Histopathologic features vary with the body site involved, but they generally consist of a mixed infiltrate of lymphocytes, histiocytes, eosinophils, and plasma cells in the stratum corneum. Fungal elements may be visualized using periodic acid-Schiff or methenamine silver staining. In circular lesions of the skin, active fungal invasion and growth occur at the rim of the lesion; the center of the lesion contains relatively few organisms. Formation of kerions in tinea capitis is marked by an intense polymorphonuclear cell infiltrate.
CLINICAL MANIFESTATIONS AND COMPLICATIONS
The clinical features of dermatophytoses vary with the site of the infection.
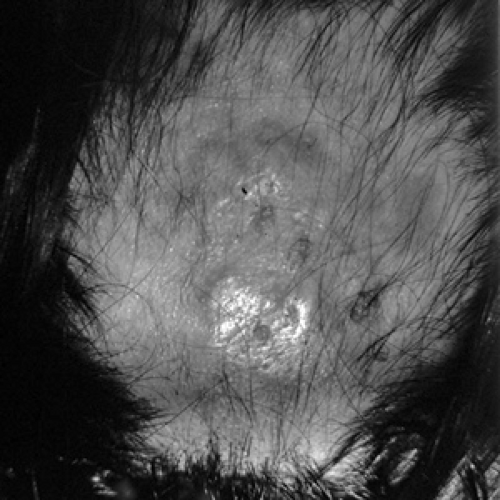
Tinea Capitis (Fig. 209.1)
Ringworm of the scalp in the United States usually is caused by T. tonsurans; M. canis and Microsporum audouinii are less common etiologic agents. In the noninflammatory variety, the lesion begins at the base of the hair shaft as an erythematous papule that then spreads peripherally as hairs break just above the level of the scalp, leaving areas of alopecia. Pruritus is a common finding. Patches, sometimes grayish, may appear at separate areas and may become confluent. The inflammatory type, more commonly associated with M. canis, may result in a pustular folliculitis and regional lymphadenopathy. Kerions are inflammatory, tender, purulent boggy masses that form as a result of the host’s immune response and generally do not represent secondary bacterial infection.
Black-dot tinea capitis is the most common presentation of tinea capitis in the United States and usually is associated with T. tonsurans. It is characterized by numerous small, round patches where hair shafts have broken off at the level of the follicle and appear as dots on the skin surface.
Tinea Corporis (Fig. 209.2)
Tinea corporis refers to dermatophytosis involving the glabrous skin in all parts of the body, with the exception of the palms, soles, and groin. The most frequent causes are T. mentagrophytes, T. rubrum, and M. canis. The typical ringworm lesion is pruritic and appears as an erythematous, annular lesion with an elevated, scaly, papular, and sometimes vesicular border spreading in a centrifugal manner while clearing centrally. Formation of kerions rarely is seen. Occasionally, tinea corporis may be confused with secondary syphilis, psoriasis, or seborrheic dermatitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree