Tetralogy of Fallot
William H. Neches
Sang C. Park
Jose A. Ettedgui
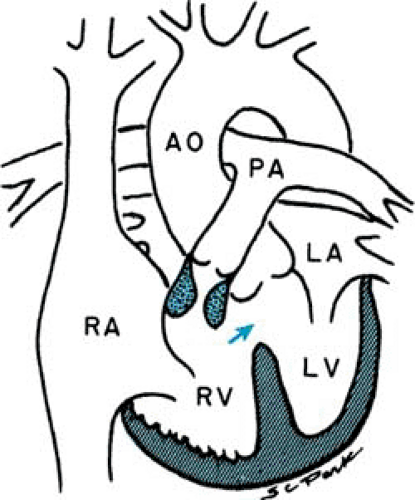
Tetralogy of Fallot refers to a spectrum of anatomic abnormalities that have in common a large, unrestrictive ventricular septal defect and right ventricular outflow tract obstruction—the two major features of the condition, although right ventricular hypertrophy and overriding of the aorta are additional features that complete the tetralogy (Fig. 265.1). Clinical presentation varies from the asymptomatic acyanotic child with a heart murmur to the severely hypoxic newborn infant. Severity of presentation depends largely on the nature and degree of the outflow obstruction. The anatomic hallmark of tetralogy of Fallot is the anterocephalad deviation of the outlet portion of the interventricular septum. The severity of the infundibular stenosis ranges from mild to severe pulmonary stenosis and to pulmonary atresia. Further obstruction to pulmonary blood flow often occurs at other levels. Pulmonary valve stenosis is a common finding, and stenoses often are found also in the supravalvar region, at the bifurcation of the pulmonary artery branches, or in the distal pulmonary arteries.
The typical ventricular septal defect in tetralogy of Fallot is large and unrestrictive and is the result of malalignment of the outlet portion with the rest of the interventricular septum. Muscular ventricular septal defects, an inlet defect, or a complete atrioventricular septal defect also may be present.
Other possible associated abnormalities include an atrial septal defect (so-called pentalogy of Fallot) or coronary artery abnormalities such as a left anterior descending coronary artery arising from the right coronary artery, which may limit the surgical approach. Approximately 25% of patients with tetralogy of Fallot have a right-sided aortic arch, an important consideration if a patient undergoes a systemic–to–pulmonary artery anastomosis. Severity of presentation depends largely on the nature and degree of the outflow obstruction.
Tetralogy of Fallot occurs in approximately 6% of infants born with congenital heart disease. The etiology is obscure. Although tetralogy of Fallot and most other forms of congenital heart disease generally occur as isolated abnormalities, children with tetralogy of Fallot are afflicted with additional major extracardiac malformations significantly more often (15.7%) than are patients with other congenital heart defects (6.8%). In addition, the extracardiac malformations may be more serious in patients with tetralogy of Fallot and include cleft lip and palate, hypospadias, and skeletal malformations. Although tetralogy of Fallot commonly is not part of specific hereditary malformation syndromes or chromosomal abnormalities, it often is found in many malformation associations, including cardiofacial, VACTERL (vertebral, anal, cardiac, tracheal, esophageal, renal, limb), and CHARGE (coloboma, heart disease, atresia choanae, retarded growth and development and/or central nervous system anomalies, genital hypoplasia, and ear anomalies and/or deafness) associations, and 22q11 deletion, as well as De Lange, Goldenhar, and Klippel-Feil syndromes.
PHYSIOLOGY AND HEMODYNAMICS
Equalized right and left ventricular pressures, along with normal or reduced pulmonary artery pressure, are the hemodynamic features produced by anatomic abnormalities in patients with tetralogy of Fallot. Because the ventricular septal defect is large and unrestrictive and the right and left ventricles contract simultaneously, the end result is, in effect, a common ventricular chamber ejecting into systemic and pulmonary circulations. Pulmonary and systemic blood flows therefore depend on the relation between pulmonary and systemic resistances. Normally, pulmonary resistance is approximately 10% of systemic resistance, and these resistances are determined by their respective distal arteriolar beds. In tetralogy of Fallot, however, pulmonary vascular (arteriolar) resistance usually is normal or less than normal, and resistance to right ventricular ejection into the pulmonary vascular bed is related instead to pulmonary stenosis.
The presenting symptoms and severity of clinical manifestations in patients with tetralogy of Fallot depend on the relation between the resistances to systemic and pulmonary outflow. When the total right ventricular outflow obstruction is such that pulmonary outflow resistance is less than systemic resistance, a net left-to-right shunt is present, and clinical manifestations are similar to those of patients with a ventricular septal defect of small to moderate size. When pulmonary and systemic resistances are similar, there is a balanced shunt with nearly equal pulmonary and systemic blood flows at rest. Finally, when resistance to pulmonary outflow exceeds systemic resistance, a net right-to-left shunt is seen, and systemic flow is greater than pulmonary flow.
Cyanosis may be mild or undetectable at rest in patients with tetralogy of Fallot but usually becomes apparent or increases with physical activity. With exercise, increased cardiac output and decreased systemic arteriolar resistance result in a considerable increase in the degree of right-to-left shunting.
Although effective cardiac output is maintained, right-to-left shunting produces a rapid decrease in systemic arterial oxygen saturation and results in exertional dyspnea and decreased tolerance for exercise. In contrast to episodes of paroxysmal hypoxemia (tetralogy spells), the systemic desaturation is limited by the duration of exercise and improves as soon as activity ceases.
Although effective cardiac output is maintained, right-to-left shunting produces a rapid decrease in systemic arterial oxygen saturation and results in exertional dyspnea and decreased tolerance for exercise. In contrast to episodes of paroxysmal hypoxemia (tetralogy spells), the systemic desaturation is limited by the duration of exercise and improves as soon as activity ceases.
Squatting is a common posture in patients with tetralogy of Fallot, particularly in young children who easily assume the more comfortable knee-chest position. Squatting often is seen in children after exercise. They also frequently are seen to assume this position while playing quiet games with their peers who are sitting. Squatting likely results in an increase in systemic arterial resistance caused by kinking and compression of the major arterial circulation to the lower extremities. This increase in peripheral resistance, in the presence of relatively fixed pulmonary outflow resistance, decreases the degree of right-to-left shunting and increases pulmonary blood flow. The result is an immediate increase in systemic arterial oxygen saturation.
Episodes of paroxysmal hypoxemia, also called hypercyanotic or tetralogy spells, often are seen in infants and children with tetralogy of Fallot and other cardiac malformations with similar physiologic features. These spells usually are self-limited and last less than 15 to 30 minutes, although they may be longer. The spells are seen more often in the morning but may occur during the day and may be precipitated by activity, a sudden fright, or injury, or they may occur spontaneously without any apparent cause. The spell is characterized by increasing cyanosis and an increased rate and depth of respiration. The physiologic change that produces a hypoxemic spell is an increase in right-to-left shunting and concomitant decrease in pulmonary blood flow. The exact mechanism by which this phenomenon occurs is unknown.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree