Tenolysis following Injury and Repair of Digital Flexor Tendons
David Netscher
Kate Kuhlman-Wood
DEFINITION
Before the late 1960s, tendon repair within the flexor sheath was so wrought with complications (mainly stiffness and adhesions) that primary repair was never undertaken, leading to the term no man’s land, until the work of Harold Kleinert dispelled these misgivings.28
Originally, tendon adhesions were felt to be a necessary part of flexor tendon healing within the flexor tendon sheath.42
However, it was subsequently understood that intrasynovial intrinsic tendon healing was adequate to support tendon repair.35,37
Nonetheless, gapping of the repair site of 3 mm or more is sufficient to cause restrictive tendon adhesions.18,44,48
Improved tendon suture techniques with strength sufficient to enable early motion in postoperative therapy combined with early active postoperative range of motion aim to reduce tendon adhesions.19,22
In spite of these innovations, tendon adhesions still may occur following digital flexor tendon repair with a reported incidence of about 10%, and so these repairs in zone II still remain a challenge.
Tendon adhesions may occur between both the flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) as well as between the tendons and the flexor tendon sheath. This results in limited tendon excursion within the sheath and consequently reduced and dysfunctional digital range of motion.
Tenolysis is the surgical release of tendon adhesions to restore tendon gliding and digital motion. This is only undertaken when
The patient is motivated and cooperative and will undertake the directed postoperative hand therapy.
A minimum of 3 to 6 months has elapsed since initial tendon repair—risk of devascularizing rupture of the tendon is much higher if tenolysis is performed before that time.
Maximum maturation of the healing scars has occurred so that the wound after the initial tendon repair is soft and supple.
Maximum passive mobility of interphalangeal joints has been reached. It makes no sense to perform flexor tenolysis in the face of a stiff and swollen finger.
The patient has plateaued in hand therapy with no further functional advances being made.
There is a substantial difference between active and passive digital range of motion, with the former being considerably less. Furthermore, outcome of tenolysis correlates significantly with total passive range of motion before tenolysis.64
The skin condition is adequate. Even if scar maturation has fully occurred but there are skin scar contractures due to soft tissue deficiency or linear scarring, this problem must be treated first by Z-plasty or local flap or skin graft before embarking on flexor tenolysis.
Overall condition of the digit—for example, a painful dysesthetic finger will be no more functional if improved range of motion is achieved.
When embarking on flexor tenolysis, both patient and physician should have a clear understanding that intraoperatively, depending on the quality of the repair site and the extensiveness of the scarring, one may need to make a decision for tendon grafting and even two-stage tendon repair with pulley reconstruction.
Proper patient selection is crucial to outcome of tenolysis. Interphalangeal joint fusion and even digit amputation may potentially be a better decision for the patient based on time away from work, older patient age, extent of external scarring, and joint stiffness.
ANATOMY
Tenolysis needs to take into consideration the pulley system of the flexor tendon sheath. Thus, access to the tendon must be carefully planned, avoiding destruction especially of A2 and A4 pulleys.11
Digital tenolysis is made even more complex by the changing interrelationships between the bifurcating FDS and its return to the midline dorsal to the FDP in the Camper chiasm.
PATHOGENESIS
The repair response to tendon injury is similar to elsewhere in the body.
Adhesions occur as a response to the healing process, and in zone II, the opportunity for restricting adhesions is much greater, occurring between two gliding tendons in a confining fibro-osseous tunnel.
Both the tendon(s) and tendon sheath are injured and thus the body repair response occurs at both locations, resulting in scarring between the tendons as well as of the tendons to the tendon sheath.
There is initially an inflammatory phase of tendon healing (48 to 72 hours), followed by the fibroblastic (collagen) phase (5 days to 6 weeks) and remodeling that lasts up to 6 months (similar to other body tissue types). The initial cellular response is largely phagocytic, followed by collagen deposition. When extrinsic healing predominates, adhesions between tendon and surrounding tissues are likely, whereas healing that is predominantly intrinsic cellular activity results in fewer adhesions.
Factors that may influence formation of excursion-restricting tendon adhesions include the extent of the initial trauma to tendon and tendon sheath,43 tendon ischemia (including loss of vincular blood supply),40 tendon immobilization, and gapping at the repair site.
Early passive and especially active therapy protocols apply stress across the repaired tendon and lead to increased repair site tensile strength, fewer adhesions, and better excursion.19,22 Thus, primary tendon repair now has as its goal a strong, gap-resistant suture technique, followed by early postoperative motion protocol.
Although motion-restricting scar-forming adhesions are no longer felt to be an inevitability following zone II flexor tendon repair, it is unrealistic to expect a tendon to heal without any adhesions at all. Exclusive intrinsic tendon healing can only occur with in vitro experimental situations. Loose adhesions may then possibly be disrupted by postoperative therapy protocols.
The role of distant cytokines has been evaluated in the pathogenesis of scar tissue and adhesions,31,57 most prominent of which has been transforming growth factor beta (TGF-β), although its exact role is still under research, and also fibronectin. The importance of understanding this cytokine activity lies in the potential to modify its activity in adhesion formation, and experiments have been performed on physical factors, such as shear stress,16 neutralizing antibodies,65 and chemical modulations (such as 5-fluorouracil).39
NATURAL HISTORY
Once mature tendon adhesions have developed, the only effective treatment is tenolysis because the adhesions will not resolve.
Progressive stretch (serial casting and dynamic external fixation with Digit Widget, [Hand Biomechanics Lab, Sacramento, CA]) may resolve joint contractures but will have no effect on tendon excursion.
Untreated, the patient remains with reduced active range of motion to the finger. The patient may learn adaptive measures by catching the affected finger between the adjacent digits into a clenched fist.
Symptomatic tendon adhesions may result in substantial morbidity through diminished range of motion and reduced hand strength. They may lead to secondary joint contractures.
Tenolysis is by far the most common secondary procedure after digit replantation.60 Even with more current forms of tendon repair and postoperative therapy, it is estimated that 10% of repaired digital flexor tendons require surgical tenolysis.54 Proximal to zone II, the need for flexor tenolysis is less common.
PATIENT HISTORY AND PHYSICAL FINDINGS
The hallmark of the diagnosis of flexor tendon adhesions is that active finger flexion is substantially less than passive flexion.
The aims of the examination are four-fold:
Assess that scars are fully mature and that joints are maximally supple before embarking on tenolysis.
Assess the quality of volar scars and soft tissue. Preliminary scar releases may potentially be required, or even provision of added quality soft tissue through flaps or skin grafts may be necessary.
Determine if tenolysis should be undertaken at all. This may be relatively contraindicated or even deemed unnecessary or delayed until conditions are more favorable—in patients of older age or age younger than 11 years,54 patients with mild functional deficits, patients with low-demand functional needs, uncooperative and noncompliant patient, very severe scarring or dysesthetic finger (in which case a “salvage” procedure such as arthrodesis or even amputation may be better options), duration since the original tendon repair (generally considered to be at least 3 months since primary repair and 6 months since tendon graft before performing tenolysis out of concern for devascularizing the tendon and sustaining tendon rupture),15,62 and vascularity of the digit (either due to direct prior traumatizing vascular injury or due to systemic effects such as in a smoker or diabetic or patient with preexisting peripheral vascular or collagen vascular disease).
Making the correct diagnosis and excluding other differential diagnoses. This involves not only excluding but also considering other potential associated conditions that may limit active finger flexion and also potentially result in joint flexion contracture.
Thus, specifically, the clinical assessment of the digit involves the establishment of a definitive diagnosis of flexor tendon adhesion (and exclusion of other causes) as well as determination of the severity of these adhesions. The examination therefore involves the following:
Have the patient actively flex the affected digits. Measure the angle of flexion of the metacarpophalangeal (MP), distal interphalangeal (DIP), and proximal interphalangeal (PIP) joints as well as determination of the total arc of active motion (summation of all three joints). Next, passively flex the finger.
Evaluate the seesaw defect.30 This results when a contracted element spans two joints:
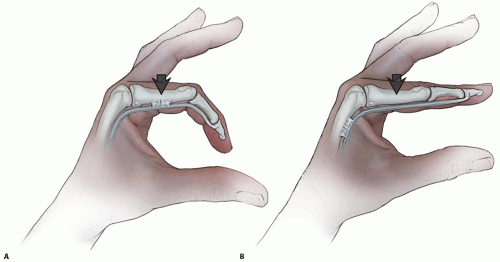
If, for example, the extrinsic flexor tendons are adherent proximal to the level of the MP joint, passive flexion of that joint will result in correction of an apparent PIP flexion contracture that results from tethering of the flexor tendons. Failure to correct the PIP contracture would mean that the contracture is inherent to the PIP joint itself (FIG 1).
In contrast, if the extrinsic extensor tendon is adherent to the metacarpal, the limitation of extensor tendon excursion distal to that joint will prevent simultaneous flexion of the MP and PIP joints (FIG 2). This is the test of extrinsic extensor tightness.32,33 Additionally, passive flexion in this case will also be limited.
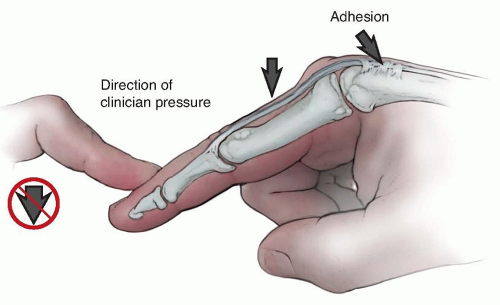
The Bunnell test for intrinsic tightness results from a seesaw phenomenon in which the band occurs across two joints but is an extensor at one joint and a flexor at the next adjacent joint.12 If this system is foreshortened, extension of the MP joint, actively or passively, will restrain flexion of the PIP joint (FIG 3). If flexion of the PIP joint is greater when the MP joint is flexed than when it is extended, intrinsic tightness is present.
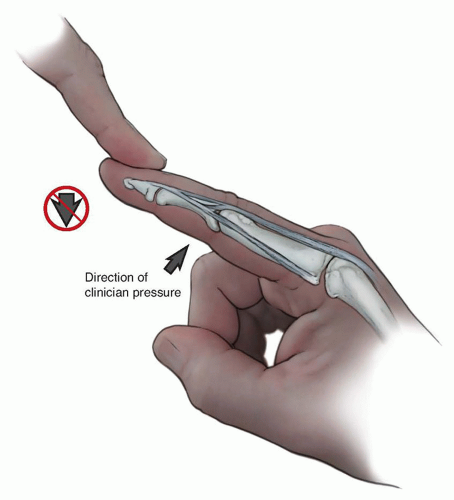
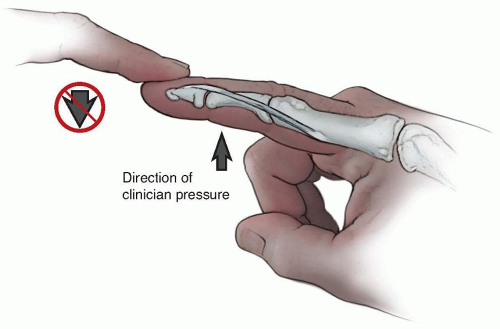
A similar volar to dorsal seesaw effect may occur at the DIP joint secondary to the action of the oblique retinacular ligament and lateral bands, resulting in an
extension contracture at that joint (ie, difficulty flexing that joint). In this boutonniere test (sometimes also called the Landsmeer test), because the oblique retinacular ligament is foreshortened, when the PIP joint is extended, passive DIP joint flexion is difficult34 (FIG 4).
Distinguish between tendon rupture and tendon adhesions. Immediately following flexor tendon repair, this distinction may be difficult because the finger is still swollen, painful, and stiff. However, later, this distinction is seldom difficult, as there is, at least, some active finger flexion with generation of stabilizing tension in the more distal joints. If active range of motion is, however, very poor, it may either be due to dense tendon adhesions or an intact but attenuated repair or even tendon ends connected through scar tissue. Special imaging will help in these circumstances.
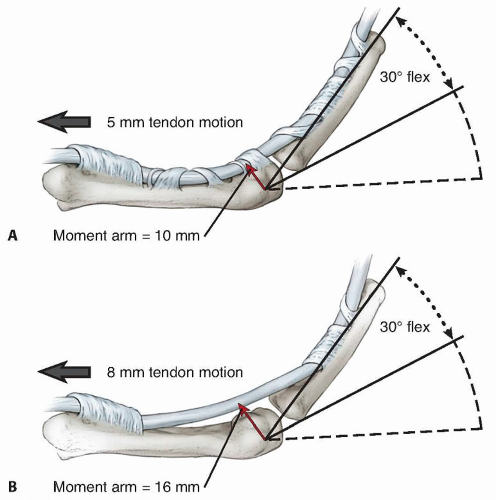
Finally, assess for flexor tendon bowstringing. Palpate for the tensing flexor tendon immediately under the skin with resisted finger flexion (FIG 5). If there is bowstringing, linear tendon excursion is “wasted” and not available for finger flexion as the tendon is displaced forward from the joint (FIG 6).6 Scar will also form dorsal to the tendon sheath in the concavity of the affected joint and add to the intrinsic joint contracture. In the presence of volar soft tissue scarring from prior injury and tendon repair, potential tendon bowstringing may be difficult to assess and may require special imaging if it is suspected.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standard radiographs of the hand are necessary to evaluate for bone or articular pathology. A true lateral image of contracted joints is important to assess the congruity of the articular surfaces.
Computed tomography (CT) scans may occasionally be selected to assess bone and articular pathology.
DIFFERENTIAL DIAGNOSIS
Following flexor tendon injury, either through sharp laceration or crushing injury, or even from previous replantation (where both flexors and extensors were repaired), active finger flexion may be reduced secondary to the following:
Rupture of the original tendon repair
Quadriga phenomenon (but adjacent uninjured fingers are also affected), if excessive advancement of tendons have been performed at the original repair site
Intrinsic tightness (if associated with severe crushing injury of the hand)
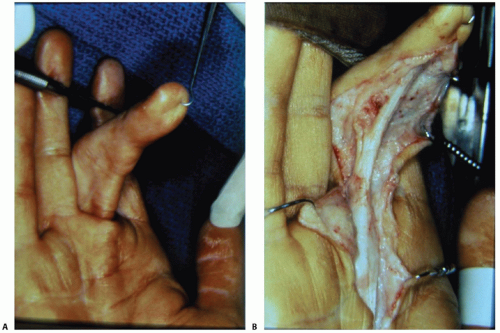
FIG 5 • A,B. Bowstringing. Tensing of the flexor tendon immediately under the skin indicates bowstringing.
Lumbrical plus phenomenon (generally applies more to tendon grafting where the graft is relatively too long and slack)
Associated extensor tendon injuries where not only is active flexion limited but there is also restriction of passive flexion
Flexor tendon adhesions, if sufficiently tight, may cause a deforming flexion force on the next most distal joint, resulting in a flexion contracture. This distinction may be partly resolved by eliciting “the seesaw effect” and flexing the preceding more proximal joint to see if the flexion contracture at the next joint improves or resolves. This phenomenon may also occur with any other associated problem that potentially crosses more than one joint, such as a soft tissue scar contracture.
Specifically, conditions initially associated with a flexor tendon injury and repair that result in PIP joint flexion contracture may include the following:
Soft tissue scar contracture
External visible clinical deformity may result from malunited fracture or direct joint injury.
Tendon bowstringing resulting from the increased volardirected vector by the tendons on the joint
Secondary scar contracture of the ligaments and volar plate of the PIP joint itself by simply being maintained in a flexed posture for prolonged period, secondary to the tendon adhesions
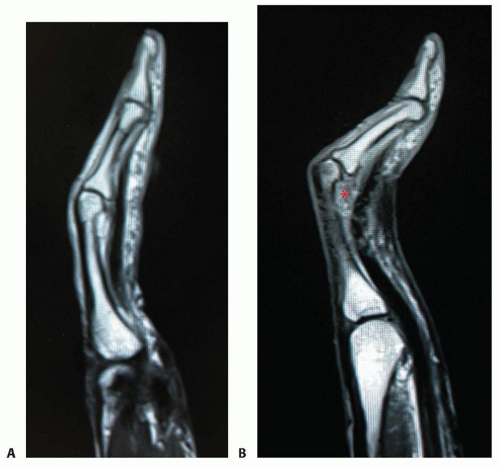 FIG 7 • MRI. A. Normal position of flexor tendon on MRI. B. Flexed PIP joint and volar displaced flexor tendons (bowstringing). Also, note scar formation dorsal to the flexor tendon in the concavity of the PIP joint (red asterisk).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|