Tendon Transfers for Ulnar Nerve Palsy
Michael S. Bednar
DEFINITION
Ulnar nerve palsy refers to loss of sensory and motor function after injury to the ulnar nerve above or below the wrist (high vs. low ulnar nerve palsy).
ANATOMY
The ulnar nerve is the terminal branch of the medial cord (C8 and T1).
The ulnar nerve consists of motor and sensory fibers. There are no muscles innervated by the ulnar nerve in the arm. In the forearm, the flexor carpi ulnaris receives its nerve branches after the ulnar nerve passes through the cubital tunnel. The other muscles innervated in the forearm are the flexor digitorum profundus of the ring and small fingers.
The muscles innervated in the hand (by order of innervation) are the following:
Hypothenar muscles
Abductor digiti minimi
Flexor digiti minimi
Opponens digiti minimi
Ring and small lumbricals
Dorsal and palmar interosseous muscles
Adductor pollicis
Deep head of flexor pollicis brevis
First dorsal interosseous (last muscle innervated by the ulnar nerve)
The sensory fibers of the ulnar nerve supply the small finger and the ulnar half of ring finger over the entire palmar surface and the dorsal surface distal to the proximal interphalangeal (PIP) joint. The dorsal surface proximal to the PIP joint of the small finger and the ulnar half of the ring finger and ulnar dorsum of the hand are innervated via the dorsal sensory branch of the ulnar nerve, which arises from the ulnar nerve 7 cm proximal to the wrist. The sensory branch crosses from volar to dorsal at the level of the ulnar styloid.
PATHOGENESIS
Ulnar nerve palsy can arise from a laceration anywhere along its course. Proximal injuries to the medial cord may present with additional sensory loss in the distribution of the medial brachial or antebrachial cutaneous nerves. Nerve compression typically occurs either at the cubital tunnel at the elbow or the canal of Guyon at the wrist.
A variety of systemic conditions may mimic ulnar neuropathy, including Charcot-Marie-Tooth disease, syringomyelia, and leprosy. In Charcot-Marie-Tooth disease and syringomyelia, there is weakness involving other nerves. In leprosy, there is a profound loss of sensation in the ulnar nerve distribution in addition to the claw deformity of the fingers.
NATURAL HISTORY
The severity of the nerve palsy depends on the degree of the nerve lesion and the presence of anomalous innervation patterns (Martin-Gruber, Riche-Cannieu) in determining the number of muscles involved and the extent of palsy. Anomalous innervation patterns can confuse the examiner.
Martin-Gruber anastomosis patterns are divided into four types:
Type I (60%): Motor branches from the median nerve are sent to the ulnar nerve to innervate “median” muscles.
Type II (35%): Motor branches from the median nerve are sent to the ulnar nerve to innervate “ulnar” muscles.
Type III (3%): Motor branches from the ulnar nerve are sent to the median nerve to innervate “ulnar” muscles.
Type IV (1%): Motor branches from the ulnar nerve are sent to the median nerve to innervate “median” muscles.
With prolonged nerve palsy, secondary abnormalities of the hand occur, such as stretching of the central slip of the extensor mechanism at the PIP joint or fixed joint flexion contractures.
PATIENT HISTORY AND PHYSICAL FINDINGS
An important point is to identify the cause and timing of palsy to determine whether the pathology can be reversed. Treatment is first addressed at improving nerve function by procedures such as decompression of a compressed nerve or acute repair of a lacerated nerve. Recovery can be gauged by progression of symptoms, such as advancing Tinel sign, return of muscle function, and return of sensation. Tendon transfers are indicated when nerve recovery is not expected or possible.
Loss of sensation in the medial arm or forearm indicates a proximal lesion. Loss of sensation to the dorsal side of the ulnar hand indicates a lesion proximal to the wrist to affect the dorsal sensory branch.
The following specific tests of motor dysfunction are used to determine the functional loss of the hand:
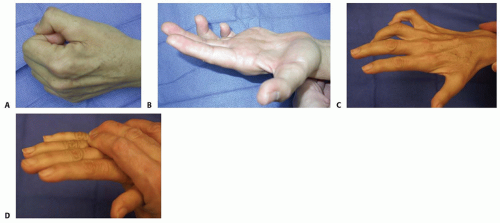
Froment sign: hyperflexion of thumb interphalangeal joint (FIG 1A); indicates substitution of flexor pollicis longus (FPL) (median nerve) for adductor pollicis (ulnar nerve)
Jeanne sign: reciprocal hyperextension of thumb metacarpophalangeal (MCP) joint (see FIG 1A); indicates substitution of FPL for adductor pollicis
Wartenberg sign: abduction of small finger at MCP joint; indicates paralyzed palmar intrinsic muscle (ulnar nerve) with abduction from extensor digiti minimi (radial nerve)
Duchenne sign: clawing of ring and small fingers, hyperextension of MCP joints, and flexion of PIP joints (FIG 1B); indicates paralysis of interosseous and lumbrical muscles of the ring and small fingers (low ulnar nerve), more pronounced in low rather than high ulnar nerve palsy
secondary to functioning flexor digitorum profundus of ring and small fingers (high ulnar nerve)
Bouvier maneuver: inability to actively extend PIP joint when MCP joints are hyperextended and ability to actively extend PIP joint when MCP joints are blocked from hyperextension (FIG 1C,D). When active PIP joint extension is possible with the MCP joints blocked, this indicates competence of the central slip (positive test). When PIP joints cannot actively extend (negative test), this implies central slip attenuation. In this case, tendon transfers will need to block MCP joint hyperextension and provide PIP joint extension.
Andre-Thomas sign: clawing of ring and small fingers, hyperextension of MCP joints and flexion of PIP joints, flexion of wrist (FIG 1C). An increase in the claw deformity as the patient tries to extend the fingers by flexing the wrist indicates a poor prognosis for tendon transfer surgery.
Masse sign: flattening of the metacarpal arch (see FIG 1B); inability to oppose the small finger carpometacarpal joint
Pollack sign: inability to flex the distal interphalangeal joint of the ring and small fingers; used to differentiate high from low ulnar nerve palsy
In assessing for tendon transfers in ulnar nerve palsy, the primary functional concerns are the following:
Lack of thumb adduction and lateral pinch
Claw deformity of fingers that impairs object acquisition and grip
Loss of ring and small finger flexion (high palsy)
IMAGING AND OTHER DIAGNOSTIC STUDIES
Electromyographic and nerve conduction velocity studies are used to isolate the ulnar nerve pathology and rule out other diagnoses. Serial studies may demonstrate the potential for recovery.
DIFFERENTIAL DIAGNOSIS
Cervical radiculopathy
Lower brachial plexopathy
Charcot-Marie-Tooth disease
Syringomyelia
Leprosy
NONOPERATIVE MANAGEMENT
When the Bouvier test is positive (active PIP joint extension is possible when MCP joint hyperextension is prevented), a dorsal MCP blocking splint for the ring and small fingers is fabricated to preserve the integrity of the PIP joint central slips.
If a fixed flexion contracture of more than 45 degrees occurs at the PIP joint, a supervised hand therapy program consisting of serial casting is required.
If the fixed flexion contracture does not respond to therapy, preliminary surgical joint release is necessary before tendon transfers.
SURGICAL MANAGEMENT
Tendon transfers address the primary functional concerns listed earlier9:
Lack of thumb adduction and lateral pinch
Claw deformity of the fingers that impairs object acquisition and grip
Loss of ring and small finger flexion (high palsy)
Considerations
Restoring Thumb Adduction
The first factor to consider in performing a transfer to restore thumb adduction is what donor muscle to use.
The extensor carpi radialis brevis (ECRB)10 and the flexor digitorum superficialis (FDS)5 are the most commonly used.
The FDS of the ring finger can be used in low ulnar nerve palsy when the flexor digitorum profundus of the ring finger is functioning.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree