Tendon Transfers for Radial Nerve Palsy
Harry A. Hoyen
DEFINITION
Radial nerve palsy that is distal to the triceps innervation affects the forearm musculature. A lesion that does not recover results in predictable wrist, finger, and thumb extensor deficits.
ANATOMY
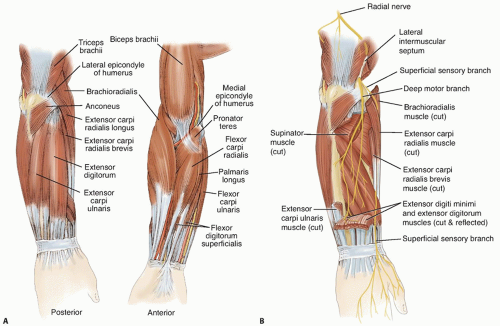
The brachioradialis (BR) and forearm extensor musculature originate in the lateral humeral epicondyle and the interosseous membrane (IOM) (FIG 1A).
Each of the extensor muscles has a relatively flat muscle belly before forming a flat, broad tendon.
The myotendinous junction for the wrist extensors is in the midforearm, whereas the myotendinous junction of the finger and wrist extensors is in the distal forearm.
The radial nerve arises from the posterior cord of the infraclavicular brachial plexus (FIG 1B). Multiple triceps motor branches are present as the nerve courses in the posterior compartment of the upper arm. The nerve traverses into the anterior compartment through the intramuscular septum. The nerve then lies between the brachialis and BR before it enters the forearm. The BR, extensor carpi radialis longus (ECRL), and extensor carpi radialis brevis (ECRB) are innervated as the nerve divides into the deep radial nerve, the posterior interosseous nerve (PIN), and the superficial radial nerve. The PIN innervates the extrinsic extensors after exiting the supinator musculature.
The motor point for each nerve is fairly consistently located just proximal to the myotendinous junction. In most cases, there is one larger motor branch from the radial nerve or PIN to each muscle.
The sequence of muscle innervation is an important distinction when considering the anatomy of the radial nerve. Whereas some nerves distribute their nerve branches in a tree-like fashion, the radial nerve innervates the extensor musculature in an orderly pattern, from proximal to distal. The proper radial nerve supplies the BR, the ECRL, and occasionally the ECRB.
The PIN innervates the ECRB, the extensor digitorum communis (EDC), the extensor carpi ulnaris (ECU), the extensor indicis proprius (EIP), and the extensor pollicis longus (EPL).
The order of innervation is important in differentiating a radial nerve injury from a mechanical myotendinous injury or muscle disruption after a forearm laceration.
Understanding the innervation also is helpful while observing and assessing the clinical recovery after radial nerve injury or repair.
PATHOGENESIS
Most radial nerve deficits result from traumatic injuries. Idiopathic and neoplastic etiologies are less common.
NATURAL HISTORY
The type of traumatic injury is an important predictor of recovery after humerus trauma.
Neurapraxic lesions typically result from low-energy injuries. Recovery can be expected over the course of 3 months. The clinical recovery can be followed by observing the advancing Tinel sign and the previously described reinnervation sequence.
Conditions that persist after 3 months can be further evaluated with electrodiagnostic studies. In the clinical setting of a nonadvancing Tinel sign and electromyographic findings of axonal loss, exploration with intraoperative electrophysiologic testing is warranted. Nerve grafting across the injury is indicated in lesions that do not demonstrate improvement after external neurolysis.19,25,26
Exploration of open and penetrating injuries is recommended. The choice of primary repair or nerve grafting depends on the injury zone. Recent evidence warrants exploration of highenergy injuries because these lesions have not demonstrated recovery. It is difficult to determine the injury at the acute setting. Interposition nerve graft is often necessary.19
PATIENT HISTORY AND PHYSICAL FINDINGS
A deficit in radial nerve innervation of the extrinsic wrist and finger extensors results in no active wrist, finger, and thumb extension.
The clinical presentation of radial nerve and PIN palsies is differentiated by the fact that the BR and ECRL are preserved in PIN palsies. Thus, a patient with a PIN deficit will have some retained composite wrist radial deviation and extension, whereas a radial nerve lesion proximal to the elbow will not have a voluntary wrist extension.
The BR can be palpated during resisted, neutral position elbow flexion, and the wrist assumes a radial-deviated position during attempted active extension.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Electrodiagnostic studies (eg, nerve conduction studies and electromyography) are used initially for assessment and for determining subsequent treatment.
Axonal loss injuries are evident about 4 weeks after the injury; therefore, the initial study is obtained until at least 4 to 6 weeks after the injury.
The electrodiagnostic study also can identify other nerve injuries that were not as evident on the initial evaluation.
Recovery can be followed by clinical examination or with supplemental studies. Reinnervation or polyphasic waveforms are seen in the muscles of a regenerating nerve.
A final study is obtained before tendon transfer at 12 to 18 months.
DIFFERENTIAL DIAGNOSIS
Muscle or tendon laceration
Closed myotendinous rupture
Cervical spinal disease
Joint or tendon subluxation (especially if there is lost digital extension)
NONOPERATIVE MANAGEMENT
Wrist and finger extension splint, especially a wrist extension splint initially after the injury, to counteract the wrist flexion position. Some finger extension can be afforded with the hand intrinsics.
Active and passive motion exercises to maintain motion and prevent contracture29 while the nerve is regenerating and in event that transfers may be necessary
SURGICAL MANAGEMENT
Tendon transfer is the mainstay of treatment. Microvascular repair and nerve graft are discussed in another chapter.
The goal of treatment is independent wrist, finger, and thumb extension with thumb abduction. Donor muscles include the pronator teres (PT), flexor carpi ulnaris (FCU), flexor carpi radialis (FCR), flexor digitorum superficialis (FDS) 3 and 4, and palmaris longus (PL).
Timing of surgical intervention is controversial. Conventional surgical recommendations are to proceed after the patient has reached a documented clinical and electromyographic plateau of useful radial nerve regeneration. This typically occurs 1 year after the nerve lesion.26 Tendon transfer primarily for wrist extension may be performed early, at the same setting as nerve surgery, to improve function and minimize brace reliance as the nerve regenerates. In securing the tendon transfer, two methods can be used. The more traditional method is a Pulvertaft weave in which the donor tendon is passed through the recipient tendon three times at respective right angles. The tension is set with appropriate tension on the donor and recipient tendons. The weave is secured with multiple mattress and figure-8 sutures. Another method involves one pass of the donor tendon through the recipient tendon, with then a side-to-side coaptation of the two tendons over 3 to 5 cm with a running, locking suture. The side-to-side transfer has demonstrated better biomechanical characteristics but require greater recipient tendon for the transfer. The surgeon needs to be familiar with both methods as they can be used in specific locations as it relates to the patient anatomy.4
Preoperative Planning
Positioning
The patient is positioned supine with arm table support and a tourniquet.
Approach
Three general exposures are used:
Radial incision with volar exposure for FCR and PT and dorsal exposure for the ECRB and ECRL
Distal dorsal incision for EDC exposure
Individual approaches for harvest of the FCU, FCR, and FDS
The ideal tendon transfer tension is based on the individual muscle properties. In general, the optimal tension is established at the peak of the length-tension curve for the donor muscle while the wrist and fingers are maintained in the ideal position. Because this donor muscle position is difficult to determine intraoperatively without specialized equipment, this point reasonably corresponds to the midpoint of the passive muscle excursion. The ideal joint position for each transfer is discussed with the individual transfers.
TECHNIQUES
▪ Wrist Extension Restoration through Pronator Teres to Extensor Carpi Radialis Ligament and Extensor Carpi Radialis Brevis2,9,28
Make a longitudinal radial incision over the midshaft of the radius.
This allows exposure of the PT and the wrist extensors through a single incision.
Identify and expose the PT volarly while protecting the radial artery and superficial radial nerve (TECH FIG 1A).
Extend the pronator insertion by harvesting a strip of periosteum distally (TECH FIG 1B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree