Tendon Disorders
William D. Stanish MD, FRCSC, FACS
Horacio Yepes MD
Amro Al-Hibshi Mbchb, FRCSC
Chronic tendon disorders are widely called tendinosis.
Inflammatory response to trauma seems most prevalent in tenosynovium and peritenon giving rise to the term ‘peritendinitis.’ Older patients with long-standing symptoms and a history of repetitive activity will be more likely to have tendinosis. Young patients with acute onset of symptoms will be more likely to have peritendinitis.
Quadriceps tendon disorders may be silent on presentation. They are asymptomatic in the majority of cases, until a major traumatic event occurs. The mean age of the patient is older than 40 years old and the male to female ratio is from 6:1 to 10:1.
In complete ruptures, a superficial prepatellar hematoma with a central gap is easily seen.
Operative treatment is indicated for complete tears and partial tears involving more than 50% of the tendon. If enough of the tendon is present distally, the tendon can be repaired directly with non-absorbable sutures. If the tendon distally is not long enough to accept sutures securely, repair of the tendon to the patella is indicated.
The four phases of jumper’s knee are: Phase I, pain after activity; Phase II, pain during and after activity; Phase III, same as in Phase II, but with diminished performance; and Phase IV, complete rupture of the patellar tendon.
Runner’s knee is a condition that involves the lateral side of the joint with the iliotibial band rubs against the lateral epicondyle of the femur. It is most symptomatic when the patient is running downhill.
Injuries and disorders of the tendons around the knee can be a devastating problem for the athlete and his/her physician. The accurate identification of these problems is extremely important to achieve proper treatment and rehabilitation. In this chapter we will review the basic science, clinical evaluation, and treatment of some of the common disorders involving the tendons in and about the knee in athletes.
Anatomy
The tendons around the knee are of great importance for the stability of the joint. As muscle-tendon units, they function as primary movers of the knee joint. Knowledge of the anatomy is critical for the team physician. It helps the physician to understand the pathologic processes that he/she may encounter with different athletes suffering with tendon disorders.
The quadriceps group consists of four muscles that converge through a conjoined tendon to insert into the superior pole of the patella (1). Other than being a major part of the extensor mechanism and a stabilizer of the knee joint, the vastus medialis (with its oblique portion) and the vastus lateralis help maintain the patella centralized. The patella works to increase the effective lever arm of the quadriceps.
The hamstring group consists of the biceps femoris laterally and the semimembranosus and semitendinosus medially. Except for the short head of the biceps, they all span the hip and knee joints (1).
The pes anserinus is the tendinous insertion of the sartorius, gracilis, and semitendinosus muscles that insert into the anteromedial aspect of the proximal tibia. A bursa separates these structures from the medial collateral ligament.
The patellar tendon is closely related to the capsule, although its function is distinct from it. The tendon forms part of the extensor mechanism. The tendon extends in a slightly oblique fashion from the inferior pole of the patella to the tibial tuberosity. The infrapatellar bursa lies in close proximity to the patellar tendon (2,3,4).
The popliteus tendon lays posterolateral to the knee joint between the capsule and the synovial membrane. An area of bare tendon lies in contact with the lateral meniscus (2,5,6).
The iliotibial band is a thickened strip of the fascia lata that inserts into Gerdy’s tubercle. The band lies anterior to the lateral femoral epicondyle in full knee extension. At 30 degrees of flexion, the iliotibial band translocates posterior to the epicondyle.
Biomechanics
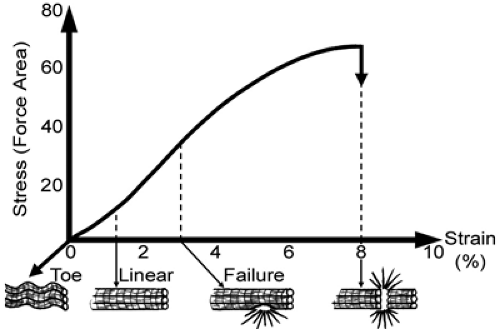
There is a large gap between the stress that causes tendon failure and physiologic loads. The latter are reported to produce less than 4% strain (7). This is the “safe zone” of the stress-strain curve (Fig 42-1). The safe zone represents the straightening of the crimped collagen fibers when the tendon is perfectly elastic and recovers its original length after the load is removed. At 4% to 8% strain, the collagen fibrils slide past one another. At 8% to 10% strain, the tendon begins to fail and resist less force. Tendon healing will be discussed in the next section on biology; the healed tendon may be up to 30% weaker biomechanically than the normal healthy tendon (8).
Biology of Healing
The body’s response to any injury is an immediate inflammatory reaction. Tendinitis is the word used to describe inflammation of the tendon. A new concept has emerged for chronic tendon disorders. They are now widely called tendinosis. This refers to a degenerative condition of the tendon that seems to be related to both age and activity level. Histologically, surgical specimens show very few inflammatory cells and are more likely to show degeneration, with fatty mucoid and hyaline features. Inflammatory response to trauma seems most prevalent in tenosynovium and peritenon giving rise to the term “peritendinitis.” It is easier to understand these terms as points of a continuum rather than discrete clinical entities. In general, older patients with long standing symptoms and a history of repetitive activity will be more likely to have tendinosis. Young patients with acute onset of symptoms will be more likely to have peritendinitis. Tendonitis occurs when the tendon bears more load than it can withstand repeatedly. Damage and its sequelae inflammation and degeneration occurs. This can be due to excessive high loads across normal tendons or normal loads across degenerative tendons (8).
Tendons heal through three phases: inflammatory, reparative, and remodeling. The inflammatory response begins with the injury and may last from 2 to 7 days. Repair may start as early as 48 hours and last for 6 to 8 weeks. Remodeling starts from day 14 and may last up to one year (8).
Disorders of the Quadriceps Tendon
History
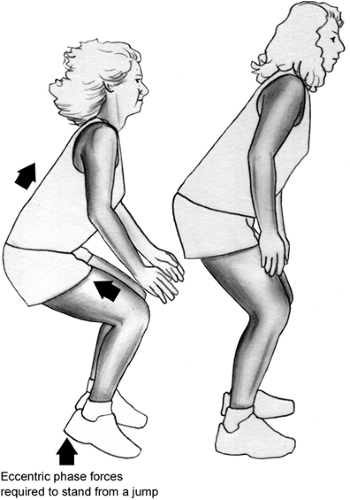
Quadriceps tendon disorders may be silent on presentation. They are asymptomatic in the majority of cases, until a major traumatic event occurs. The mean age of the patient is usually older than 40 years. The male to female ratio is 6:1 to 10:1. The reduced tensile strength of the tendon is multifactorial. Aging and hypoxic degeneration of the tendon, combined with eccentric and compressive forces over the femoral condyles are proposed as risk factors for micro- and macroruptures. Injuries may also occur in younger athletes participating in high power sports such as basketball, high jump, volleyball, and weightlifting (Fig 42-2). A chronic cycle of stiffness and pain with exercise may be experienced by the athlete, but in many cases no symptoms are experienced. In some cases, the history of quadriceps weakness and difficulties going down hill may bring the clinician a key for considering this pathology.
Patients experiencing ruptures commonly have an antecedent traumatic event with or without an eccentric force. Forceful quadriceps contraction within a degenerative and weak tendon in patients with rheumatologic or collagen diseases (as systemic lupus erythromatosus, rheumatoid arthritis, psoriasis, polyarteritis nodosa, or gout) may lead to rupture of the tendon. Patients with history of diabetes mellitus, hyperparathyroidism, uremia, chronic corticosteroid use, renal failure, or chronic acidosis are also at increased risk for developing non-traumatic ruptures. Cortisone injections lead to weakness of the tendon and increase the risk of non-traumatic ruptures. A complete medical history (including past history) should be obtained (9,10).
Physical Findings
Examination usually elicits tenderness and swelling in the central portion of the quadriceps tendon close to its insertion into the superior pole of the patella. Some patients experience the tenderness close to the musculotendinous junction. The commonest site of non-traumatic ruptures is between 1.0-2.0 cm from the insertion into the patella (Fig 42-3). The commonest site for traumatic ruptures is at the insertion into the patella.
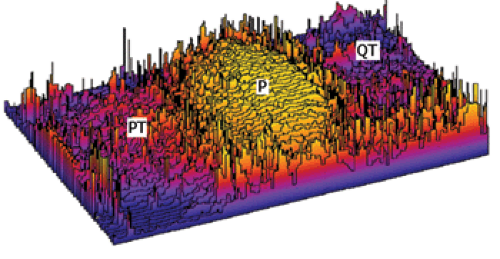
In our vascular laboratory, we have studied the vascular supply of the quadriceps tendon and patellar tendon using an injection technique of lead oxide gel and water. This mixture is injected into the femoral arteries. Angiograms of the tendons are created, and the density of vascularity is determined with image analyzer software. Our studies (paper in progress) identified a zone of hypovascularity within 2 to 3 cm from the insertion of the quadriceps into the patella (Fig 42-3). This finding correlates well with the site of clinical ruptures of the tendon.
In partial ruptures, the presence of a gap is not often easy to palpate. Partial tears might not be easily diagnosed initially until the size of the gap increases enough to be detected. Most patients with partial tears will still be able to perform straight leg raises.
In complete ruptures, a superficial prepatellar hematoma with a central gap is easily seen. The defect can get exaggerated if the patient is asked to perform active extension of the involved knee (Fig 42-4). Failure to actively extend the knee and/or to straight leg raise indicate a complete tear of the tendon (9,10).
Imaging Modalities
These may include radiographs which are not specific for quadriceps tendon injury. With complete tears, patella infera (baja) may be identified (Fig 42-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree