CHAPTER 27 Technique for Chemonucleolysis of Lumbar Disc Herniation
INTRODUCTION
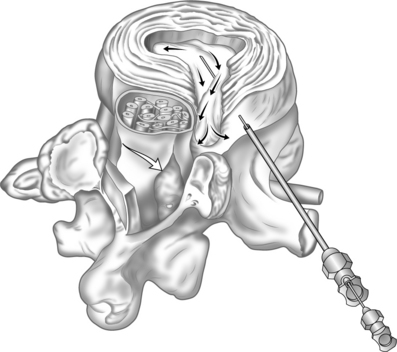
Chemonucleolysis is a method for the dissolving of displaced nucleus pulposus of the spinal intervertebral disc (Fig. 27.1).1 Chymopapain, a non-specific proteoglycanase derived from the fruit of papaya plants, remains the only clinically proven substance for the purpose of treating displaced discs in humans and animals by chemonucleolysis.2 The technique of chemonucleolysis was perfected over a period of more than 40 years primarily for the use of chymopapain although other agents including the enzymes collagenase3 and chondroitinase ABC4 have been studied for this purpose.
BACKGROUND/HISTORY
The non-specific proteolytic action of chymopapain is destructive to delicate microvascular tissues which can result in severe neurologic complications5 and therefore is very dangerous if injected into the wrong places in the spine. Consequently, a very specific and safe technique for injecting this enzyme into the intervertebral disc has evolved for what would seemingly be an easily performed procedure.6–8
Chymopapain not only has the potential for severe local tissue toxicity but it is also very allergenic dispite its wide use in food additives. As much as 3% of the North American population has been sensitized to papaya enzymes. During the early clinical experience with this enzyme there were several preventable fatalities and severe neurologic complications in humans following chymopapain injection.9
INDICATONS/CONTRAINDICATIONS
Patient selection is of paramount importance for the safe outcome of the chemonucleolysis procedure.10 Candidates for chemonucleolysis are otherwise healthy individuals who suffer from lumbar disc displacement causing primarily radicular pain, with or without mild to moderate neurologic deficit(s), who have not responded to an adequate course of medical rehabilitation and interventional spine treatment. Pregnant patients, children under the age of 16, those with uncontrolled medical conditions, and psychologically impaired individuals are not candidates for this procedure. It is contraindicated to inject patients with a history of allergy to papaya fruit, pervious injection with chymopapain, or with IgE antibody to chymopapain. Patients who suffer from severe and/or progressive neurological deficits or cauda equina syndrome are not candidates for chymo-papain, but should be operated upon as an emergency.
Relative contraindications for this procedure are patients who require large amounts of narcotic medications, morbidly obese individuals, and smokers. Recurrent disc herniations at previously operated levels should not be injected with chymopapain.11
Ideal candidates for the procedure have a one-level lumbar disc herniation primarily causing leg pain, who have not responded to 6 weeks of conservative care, which may have included one to three selective nerve root injections and who do not have any of the contraindications listed above. They are patients who are in good health or would be cleared for surgery by their internist and would likely experience some relief of pain following a surgical disc excision. Patients should be informed of the nature, benefit and risks of chemonucleolysis compared to surgical disc excision. Although chemonucleolysis fails and surgery is required in 20% of patients compared to reoperation rate of less than 10% with laminectomy, the severe complication rate is 10 times more with surgery as compared to chymopapain injection.12 Patients should be informed of the high rate of satisfactory outcomes achieved with prolonged observation and no treatment at all for proven symptomatic lumbar disc displacement.13 Chemonucleolysis with chymopain does not adversely effect the outcome from subsequent surgical disc excison.11
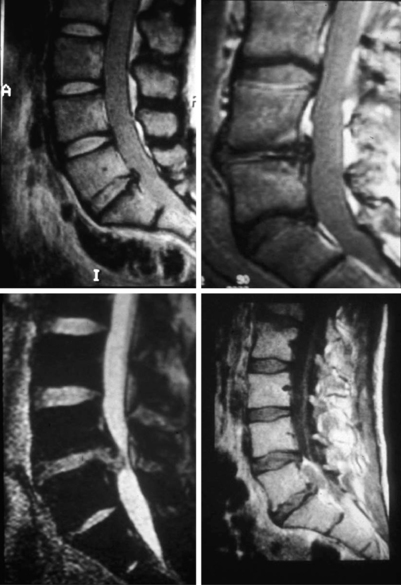
Confirmation of the diagnosis of proven symptomatic lumbar disc displacement should almost always be made with a good-quality magnetic resonance imaging study (MRI).14
As emphasized throughout this text, it is absolutely imperative to identify a displaced disc that is compressing a spinal nerve that corresponds to the patient’s symptoms and signs. Remember that totally asymptomatic individuals may have a herniated disc on MRI.15 The use of a contrast-enhanced MRI to detect suspected intrathecal tumors or underlying disc space infections should be considered if the patient has progressive and severe night pain with sleep disturbance or if the first MRI shows abnormal signal intensities in the disc or vertebral body suspicious for infection.
MRI is the only imaging technique that can distinguish among the various degrees of disc displacement,16 i.e. contained disc displacement with the anulus fibrosus intact, bulging and prolapsed discs versus noncontained discs, extruded and sequestered discs where the nucleus pulposus has displaced through the ruptured anulus fibrosus into the spinal canal. An extruded nucleus pulposus is partially displaced into the spinal canal whereas the sequestered fragment of disc is completely displaced into the spinal canal at various distances from the disc space (Fig. 27.2).
Massive disc displacement with almost complete compromise of the spinal canal is not a contraindication for chemonucleolysis as long as it is not causing severe or progressive nerve injury. Additionally, central disc displacement causing primarily low back pain can be successfully managed by chemonucleolysis.17
TECHNIQUE
Patient preparation for the procedure is important. Determination of the presence of IgE antibody to chymopapain is an important precaution to prevent injection of potentially allergic individuals.18 In North America there is a commercially available test, ChymoFast™, to determine even traces of IgE in the serum. Skin testing has not proven to be helpful in screening patients who are susceptible to an anaphylactic reaction to chymopapain.19
Pretreatment of the patients with H1 and H2 histamine receptor blockers to ameliorate the severe consequences of a systemic allergic reaction have not been proven to be effective. H1 blockers such as diphenhydramine must be given in such high doses for an extended period of time prior to exposure to antigen that the patient becomes sedated and difficult to manage as an outpatient. Administration of corticosteroids as H2 histamine blockers must be given for at least 24 hours prior to chymopapain injection and their effectiveness in preventing a full-blown anaphylactic reaction has not been proven. When given in large doses they are not without complications, such as gastrointestinal bleeding or making the patient susceptible to infection. For these reasons the author does not advocate the use of H1 and H2 blockers in preparation of the patient for chemonucleolysis with chymopapain.18
Chemonucleolysis with chymopapain should be performed under local anesthesia with careful supplemental intravenous sedation so that the patient can alert the physician if the needle stimulates a spinal nerve. It has been estimated that needle penetration of a nerve occurs in 7% of patients undergoing the procedure under general anesthesia.18 Penetration of the neural elements may lead to inadvertent intrathecal injection of the enzyme where neurological damage may occur. The incidence of catastrophic neurologic complications was higher in patients undergoing the procedure under general anesthesia versus local anesthesia.18 General anesthesia masks the early symptoms of systemic allergic reaction at a time when it is critical to initiate administration of epinephrine.20 Some agents utilized in induction and maintenance of general anesthesia enhance histamine release during an anaphylactic reaction, thus making the reaction more severe.21 It is therefore important to perform the procedure under local anesthesia with the patient alert enough to relate the symptoms of a systemic allergic reaction and to warn the operator if the injection needle is touching a nerve, so that the operator can redirect it.
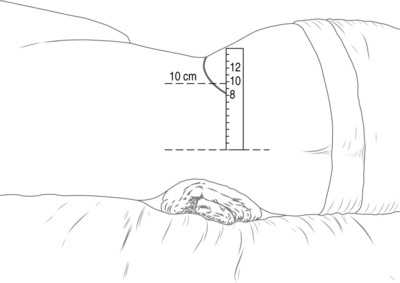
An anesthesiologist should insert a large-bore intravenous access line and administer conscious sedation and be prepared with a syringe containing 1:200 000 dilution of epinephrine. The patient is positioned in a lateral or prone position (operator’s preference). The author’s preference is the left lateral decubitus position with a bolster under the left side between the ribs and iliac crest (Fig. 27.3). Tape the patient in the true lateral position. Bring the bipolar fluoroscopy unit into play and line up the disc space that is to be injected. Have the patient’s MRI scan in the room and review it just before doing this to confirm the appropriate level. You must be able to clearly see the bony end-plates of the disc to be injected in both an anterior–posterior and lateral projection before proceeding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree